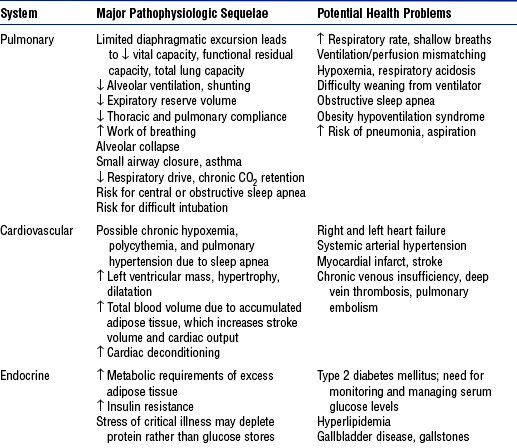
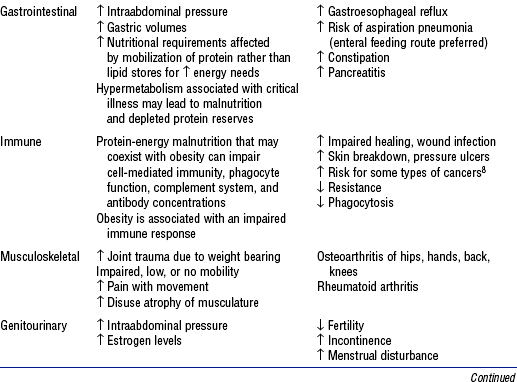
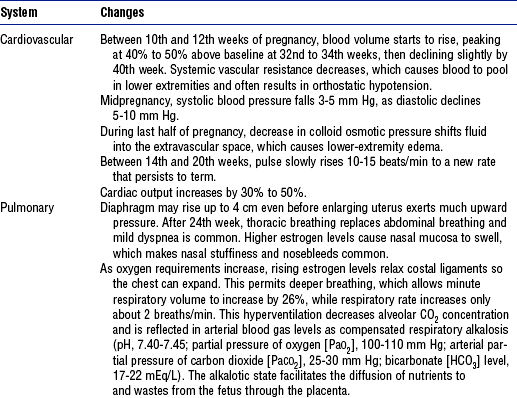
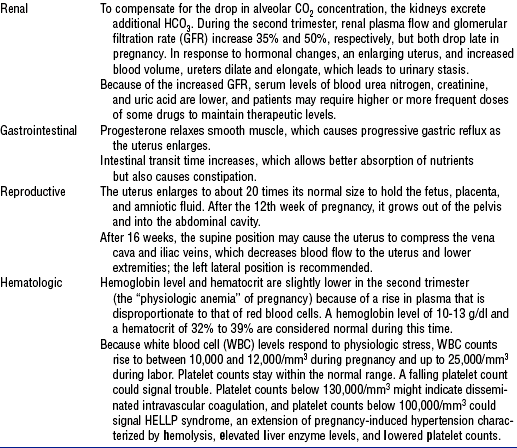
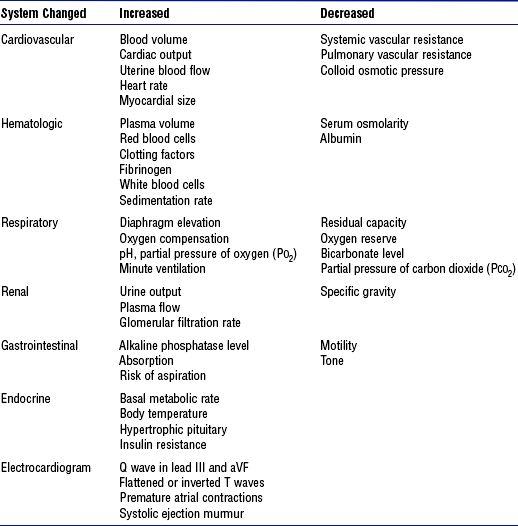
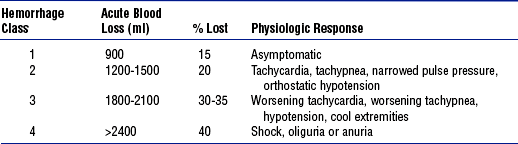
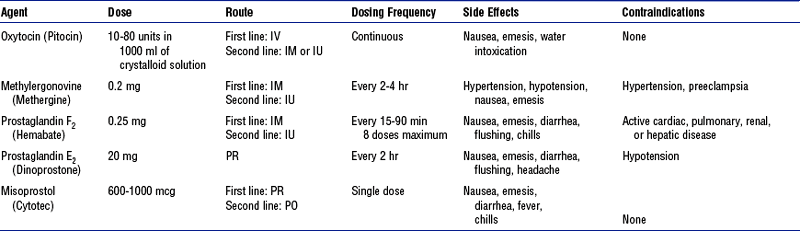
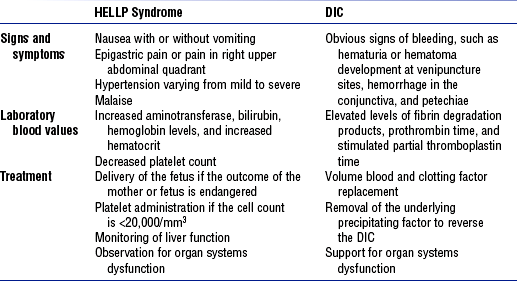
CHAPTER 11 SUSAN GALLAGHER, RN, MSN, CNS, PHD Geriatric Patients:, GINETTE A. PEPPER, PhD, RN, FAAN High-Risk Obstetric Patients:, AMY A. NICHOLS, RN, CNS, EDDPatient Transport:, RENEE HOLLERAN, RN, PhD, CEN, CCRN, CFRN, FAENPediatric Patients:, NANCY BLAKE, RN, MN, CCRN, CNAASedation In Critically Ill Patients: and JAN ODOM-FORREN, MS, RN, CPAN, FAAN 1. Description: Obesity is a multifaceted condition of excess stores of body fat 2. Etiology: Complex and multifactorial a. Causes may include behavioral, genetic, metabolic, biochemical, cultural, and psychosocial factors b. Diet, appetite control, ethnicity, and sedentary lifestyle are contributing factors 3. Definitions (American Society of Bariatric Surgery) a. Body mass index (BMI): Ratio of weight (in kilograms) to the square of height (in meters) i. Most common and widely accepted means of measuring and expressing the degree of excess weight or obesity ii. Significantly correlated with total body fat content; caution needed when interpreting BMI in children and in adults with edema, ascites, pregnancy, or highly developed muscles because elevated BMI does not accurately reflect excess adiposity in such cases iii. Normal: BMI of 18.5 to 24.9 iv. Overweight: BMI of 25 to 29 b. Overweight: Excess body weight compared to established standards (e.g., National Center for Health Statistics defines overweight as a BMI of ≥ 27.8 in men and ≥ 27.3 in women). Excess weight may come from muscle, bone, fat, and/or water. c. Obesity: BMI of 30 or higher i. Refers to an abnormal proportion of body fat ii. Individual may be overweight without being obese (e.g., body builder); however, many people are both e. Bariatrics (from the Greek baros for “weight”): Health care related to the treatment of obesity and associated conditions a. Recent estimates suggest that more than 67% of U.S. adults are overweight (Goulenok, Monchi, and Chiche, 2004) b. Among Americans aged 26 to 75 years, 10% to 25% are obese and more than 3% to 10% are morbidly obese, which reflects an increase of more than 25% over the past three decades irrespective of age, gender, ethnicity, socioeconomic status, or race c. Worldwide problem in both developed and developing countries 5. Pathophysiology of obesity: Physiologic sequelae of excess body weight adversely affect most body systems (Table 11-1) 6. Clinical significance to critical care nursing a. Recent evidence suggests that high BMI may be an independent prognostic risk factor for mortality in intensive care unit (ICU) patients b. Obesity is directly and indirectly associated with a wide spectrum of serious health disorders (see Table 11-1) that may accompany, underlie, and complicate whatever caused the patient to be admitted into a critical care unit c. When obese patients are hospitalized, they pose a number of additional challenges to health care facilities and staff i. Increased risk for all complications related to the immobility imposed by their size (i.e., skin breakdown, cardiac deconditioning, atelectasis, deep venous thrombosis, muscle atrophy, urinary stasis, constipation, bone demineralization) ii. Likelihood of longer length of stay than nonobese iii. Vulnerability to care issues more or less unique to this population (a) Technical difficulties with common procedures such as endotracheal intubation, weaning from mechanical ventilation, positioning, weighing, and ambulation (b) Challenges in establishing vascular access, managing fluid balance, and determining nutritional requirements (c) Altered pharmacokinetics for some drugs due to differences in metabolism, protein binding, distribution, and clearance in obese persons, which leads to uncertain effects (d) Inability to use some diagnostic tests due to size or weight limits (e) Lack of availability of equipment, supplies, or additional staff that optimal care might suggest a. Obesity hypoventilation syndrome (also known as Pickwickian syndrome) i. Definition: Oxygenation decreases as BMI increases, likely due to elevated intraabdominal pressure in which mass and weight compress the thoracic cavity and limit diaphragmatic excursion. Chronic CO2 retention leads to hypercapnia, respiratory acidosis, and dependence on hypoxia for ventilatory drive. ii. Related to obstructive sleep apnea, characterized by drowsiness, narcosis, daytime napping, difficulty sleeping at night, fatigue, hypersomnolence, depression, right heart failure, and further weight gain iii. Incidence of respiratory complications has a direct relationship to BMI, especially among those over 350 lb iv. Risk factors include male gender, middle age, mild sedation, BMI over 30 v. Intervention: Noninvasive positive pressure ventilation can be tried; however, mechanical ventilation must be readily available i. Obese patients are at risk for respiratory failure due to their high oxygen consumption, decreased functional residual capacity (FRC) (which decreases exponentially with increased BMI), decreased expiratory reserve volume, and decreased total lung capacity ii. FRC may fall into the range of closing capacity, which leads to small airway closure, ventilation/perfusion mismatch, arterial hypoxemia, and limited oxygen reserve iii. Obese patients often experience diaphragmatic fatigue. Pressure-supported ventilation alone or with backup allows resting of the diaphragm. (a) Mechanical ventilation initiated with a tidal volume (VT) of 5 to 7 ml/kg, based on ideal (not actual) body weight, then titrated to the patient’s ventilator mechanics (b) Placement in reverse Trendelenburg’s position at 45 degrees may improve respiratory mechanics, maximize lung function, and increase successful ventilation or weaning. Supine position leads to decreased compliance and increased airway resistance. (c) Placement in the prone position can improve FRC, compliance, and oxygenation. Placing a morbidly obese patient in the prone position is difficult but not impossible; hydraulic lifts help. Positive caregiver attitude and preplanning are essential. v. Airway management requires securing of the airway, intubation, secretion control, use of special equipment, and proper positioning (a) Assess risk factors for airway placement (6) Protruding or missing maxillary incisors (8) Unusually small or large mandible (9) Erratic head or neck movement (b) Measure the distance from the sternal notch to the tip of the chin in the neutral and maximally extended positions (extension should increase by 5 cm) (c) Intubation may be challenging, with difficulty in visualizing landmarks. The Combitube is an esophageal-tracheal double-lumen airway recognized by the American Heart Association and the American Association of Anesthesiologists as an alternative to the endotracheal tube for use in obese patients. vi. Failure to control tracheostomy secretions leads to skin breakdown, odor, and threat to a patent airway. For patients with a thick, short neck and excessive parapharyngeal fat deposits, tracheostomy surgery can be difficult, because the trachea may be buried deep in tissues. Wound is managed like any other open wound: Nonadhesive, absorbent, ¼-inch foam dressing is used to absorb excess drainage, protect the wound, and prevent injury from adhesives. Tracheostomy ties should be longer and wider to prevent trauma within skin folds. vii. Equipment should be tailored to best serve patient and caregiver needs c. Pneumonia (see also Chapter 2) i. Most common cause of death from hospital-associated infection, with a prevalence of 5 to 10 per 1000 admissions. Incidence is fourfold higher in intubated, mechanically ventilated patients, because of decreased VT, decreased mucociliary transport, increased atelectasis, and infectious complications, which lead to increased morbidity and mortality. (a) Literature suggests that the widely accepted standard of care calling for repositioning every 2 hours is seldom met; even when it is included in the hospital-mandated protocol, the standard is met only 50% of the time in critical care settings (Krishnagopalan, Johnson, and Low, 2002) (b) Until pneumonia resolves, wound healing usually plateaus or deteriorates. Use of full-body lateral rotation therapy may reduce interface pressures, promote pulmonary function, and provide therapeutic positioning. Value of rotation therapy when used to prevent physical hazards of immobility and to manage difficulties with repositioning must be determined. d. Pulmonary embolism (PE) (see also Chapter 2) 2. Potential skin integrity complications: Pressure ulcers a. Result from pressure, friction, and/or shear; often related to insufficient frequency of and/or ineffective repositioning of the very obese patient as well as the presence of multiple overlapping skin folds that can foster the growth of bacteria or yeast b. Contributing factors include moisture, dehydration, and malnutrition c. Staging depends on the depth of damage to underlying tissue d. Obese patients are at risk for atypical pressure ulcers caused by pressure within skin folds related to tubes, catheters, or an ill-fitting chair or wheelchair i. Pressure within skin folds can be sufficient to cause skin breakdown; tubes and catheters burrow into skin folds and further erode the skin surface ii. Pressure from side rails or armrests not designed to accommodate a larger person can cause pressure ulcers on the patient’s hips (a) Use equipment properly sized for the patient (b) Place and secure tubes so the patient does not rest on them (c) Reposition (including tubes, lines, catheters) at least every 2 hours (d) In patients with a large abdominal panniculus, it too must be repositioned to prevent ulceration beneath the panniculus. Alert patients can help lift the panniculus; dependent or unconscious patients can be turned onto the side to aid the nurse in lifting it. e. Rotation therapy can afford effective and timely repositioning for very large patients who otherwise pose a considerable challenge to frequent turning. Even when rotation therapy is used, precautions must be taken to prevent friction and shear by using correct pressure settings, using an appropriately sized surface, and monitoring skin integrity frequently. 3. Other potential complications related to obesity: See Table 11-1 i. Roux-en-Y gastric bypass: Bypasses the duodenum and some portion of the jejunum; most frequently performed open procedure ii. Adjustable gastric banding 2. Potential postoperative surgical problems (beyond usual surgical risks such as bleeding, infection, emboli, aspiration, etc.), especially for open abdominal (vs. laparoscopic) procedures, for the morbidly obese and for those with underlying cardiopulmonary disorders a. Potential for physical injury i. Increasing incidence, cost, and number of back injury claims associated with patient care. More than half of strains and sprains are attributed to manual lifting. Manual lifting and transferring of patients are among the most frequent causes of nursing-related injuries. ii. Lack of appropriate equipment and/or staff support at the facility b. Greater complexity: Nursing care becomes increasingly more complicated and problematic as the size and weight of the patient population increase c. Attitudes toward obese patients may include and communicate a negative bias a. Standard hospital equipment, such as chairs or bed frames, may pose safety risks for obese patients and their caregivers b. Equipment specially designed for obese patients can improve quality of care, reduce length of stay, and make care easier and safer by reducing work-related back injuries among caregivers and lowering the risk of patient injury c. Heavy-duty walkers (for patients weighing 300 to 1000 lb) and heavy-duty beds, lifts, and wheelchairs that support up to 1000 lb are available to facilitate mobilization of very large patients. Preplanning with vendors is important. a. Policy makers, insurance carriers, health care facilities, and clinicians all need to use standardized measurements and definitions when developing policies, procedures, and protocols for critically ill bariatric patients b. Bariatric patient criteria (e.g., actual weight, width at widest point, or BMI) should determine which health care professionals and resources are needed in patient care to prevent complications and improve outcomes i. Institutional policies and procedures must be available to obtain transport, transfer, and patient care devices ii. Criteria-based protocols for the use of bariatric devices are designed to ensure more appropriate, timely, and cost-sensitive use of equipment iii. Performance improvement teams can help develop and implement policies and identify resources for bariatric equipment needs c. Health care professionals on the bariatric care team (physical therapist occupational therapist, or respiratory therapist; internist; bariatric surgeon; dietitian; bariatric clinical nurse specialist; wound, ostomy, and continence nurse; pharmacologist; home care coordinator; equipment vendors) need to be interested in improving critical care for the obese patient 1. Biologic and behavioral differences between older adults and younger adults require modification of nursing care 2. Age-related changes derive from three sources, according to Sloane’s rule of thirds (1992): a. One-third are related to disease processes that are more common in older adults b. One-third are related to disuse and inactivity, which increase with age c. One-third result from the aging process and occur in virtually all people who live long enough. These changes aggravate diseases and the changes associated with disuse. 3. Normal age-related changes and implications for nursing care are summarized in Table 11-2 TABLE 11-2 Compiled from Beers MH, Jones TV, Berkwits M, et al: The Merck manual of health and aging, Whitehouse Station, NJ, 2004, Merck Research Laboratories; Ebersole P, Hess P, Luggen AS: Toward healthy aging, ed 6, St Louis, 2004, Mosby; Kane RL, Ouslander JG, Abrass IB: Essentials of clinical geriatrics, ed 5, New York, 2004, McGraw-Hill; and Timeras PS, editor: Physiological basis of aging and geriatrics, ed 3, Boca Raton, Fla, 2003, CRC Press. McGraw-Hill 1. Adverse drug reactions are more common in older adults than young adults (Routledge, Mahony, and Woodhouse, 2003) 2. Major reason older adults have more adverse drug reactions is that they have more diseases and take more medications, but age-related changes in drug pharmacokinetics also contribute. The most clinically significant pharmacokinetic changes in old age include the following (Pepper, 2004; Turnheim, 2003): a. Absorption of drugs shows few age-related changes, although decreased gastric acid alters the dissolution of some drugs (e.g., enteric-coated tablets dissolve faster and may cause irritation) b. Distribution of drugs is altered by changes in body composition. Greater fat mass increases the storage and half-life of lipid-soluble drugs (e.g., psychotropic drugs). Highly protein-bound drugs (>90% bound) are more likely to be involved in drug interactions. c. Metabolism of high-clearance drugs (those that are avidly metabolized) is decreased due to decreased liver blood flow i. If a drug reference indicates that a drug undergoes first-pass metabolism, it has a high hepatic clearance ii. Effects of agents with high hepatic clearance should be assessed carefully to detect toxicity, especially if an elderly patient is not prescribed a dose lower than the typical adult dose d. Excretion of drugs that are eliminated unchanged or as active metabolites by the kidneys is markedly impaired with aging 3. Drug interaction is another important factor in adverse drug reactions in older adults, primarily due to the number of drugs taken. The most significant drug interactions include the following: a. Drugs that decrease gastric acid production (e.g., H2-blockers, proton pump inhibitors, antacids) may alter the absorption of oral drugs b. Concurrent use of two drugs highly bound (>90%) to plasma albumin will increase the effect of one or both drugs, especially if drug elimination is impaired by age or disease. Use a current drug handbook for data on the degree of protein binding. c. Drugs that induce or inhibit cytochrome P450 (CYP) enzymes can cause drug toxicity. Use a reference source that is frequently updated, such as Drug-Interactions.com (2005). CYP inhibition is the most significant drug interaction–related cause of adverse drug effects in elderly patients. d. Drugs whose output is affected by urine pH (quinidine, amphetamines, ephedrine, phenobarbital) or that undergo tubular secretion (probenecid, cimetidine, omeprazole) can interact with and contribute to the toxicity of drugs like methotrexate, procainamide, acyclovir, nitrofurantoin, and cisplatin (Karyekar, Eddington, Briglia, et al, 2004) 4. Nonadherence to the drug regimen and prescribing error, in addition to physiologic and pharmacologic factors, may contribute to adverse drug reactions a. Nonadherence with the prescribed drug regimen is a common cause of hospitalization among the elderly, although many comply closely with the regimen for prescribed medications (Beijer and de Blaey, 2002) i. Teaching patients about medications as they are administered in the hospital may improve knowledge and result in better adherence (Barat, Andreason, and Damsgaard, 2001) ii. At a minimum, the name and purpose of the medication should be stated at the time of administration if the patient is awake and cognitively intact b. Often there is no accurate list of a patient’s medications during transitions (from home to hospital; from unit to unit in the hospital), which are times of high risk for prescription and transcription error i. Elderly patients are more likely to have errors in the medication list (Bedell, Jabbour, and Goldberg, 2000) ii. Joint Commission on Accreditation of Healthcare Organizations (JCAHO, 2005) recommends the reconciliation of medication lists at transitions to promote accuracy in medication regimens (Pronost, Weast, and Schwarz, 2003) c. Expert consensus panels have identified medications to avoid prescribing for older adults; the guidelines regarding potentially inappropriate medication use are called the Beers criteria (Fick et al, 2003) 1. Geriatric syndromes are broad categories of signs and symptoms that may have a variety of contributing factors, including normal aging changes, multiple diagnoses, and adverse effects of therapeutic interventions. Syndromes are a major focus of nursing research and best practice guidelines. 2. SPICES is a tool for assessing major geriatric syndromes (Wallace and Fulmer, 1998). Pain is another important geriatric syndrome. 3. Nutritional and hydration disorders a. Older adults with multiple illnesses are at risk for malnutrition (Lawrence and Amella, 2004). Risk factors for decreased muscle mass, poor immune function, and poor outcomes include underweight (BMI <19) and overweight (BMI >26). b. Mini Nutritional Assessment (MNA) is a quick, noninvasive screening and assessment tool to identify older adults at risk of malnutrition (Nestlé Nutrition, 2005). Seek nutritional team consultation for at-risk elderly. c. Assess hydration status using a dehydration risk appraisal checklist. If no parenteral fluids are being administered, consider shortening the nothing-by-mouth time before diagnostic tests (2 hours) and replenish fluids as soon as tests are completed (Mentes, 2004). a. “Geriatric triad” includes three conditions that can cause confusion: Delirium, depression, and dementia b. Delirium is an acute, reversible, life-threatening syndrome characterized by fluctuating alteration in mental status, inattention, and altered level of consciousness. Stereotypy (repetitive behaviors such as picking at the bedding) may be present. It is a cognitive reaction to a physiologic state. i. Prevalence is up to 25% of the hospitalized elderly and up to 65% of postoperative elderly patients older than 70 years of age (Beers, 2005). Increases the risk for death or poor outcome. ii. Mnemonic DELIRIUM summarizes the most common causes: (c) L: Lack of drugs (withdrawal) (f) I: Intracranial events (stroke, meningitis) (g) U: Urinary incontinence and fecal impaction iii. Confusion Assessment Method is used to differentiate delirium from dementia and other conditions (Inouye, van Dyck, Alessi, et al, 1990) iv. Having a family member or sitter present until the physical condition is resolved reassures the patient c. Dementia is a chronic, irreversible, progressive condition with insidious onset that is characterized by memory and thinking deficits involving orientation, visuospatial skills, language, judgment, concentration, and the ability to sequence tasks i. Present in about one third of the hospitalized elderly but undiagnosed in many. Often dementia is uncovered by the stress of hospitalization (Mezey and Maslow, 2004). Unrecognized dementia increases the risk for delirium (Fick and Foreman, 2000). ii. Question the family or identify behaviors to detect dementia (Mezey and Maslow, 2004) d. Depression is common in older adults, affecting up to 43% of older adults in acute care. Can be reversed if detected early. Untreated depression can lead to cognitive impairment, physical debilitation, and suicide (Kurlowicz, 1999). a. Incidence and severity of falls is higher among hospitalized patients than among the community-dwelling elderly. Injury rate for hospital falls is 10% to 25%. Injuries associated with falls account for 6% of medical expenses for older adults (American Geriatric Society, 2001). b. Risk for falls is multifactorial. JCAHO 2005 goals require facilities to assess and periodically reassess patients’ risk for fall. Validated risk assessment tools are the Morse Falls Scale (Morse, Morse, and Tylko, 1989) and the Fall Assessment Tool (Farmer, 2000; Hollinger and Patterson, 1992). c. Implement standardized and individualized fall prevention program (Resnick, 2003) a. Pain management principles are the same as for other age groups b. Regular assessment for pain is imperative. Cognitively impaired older adults can give reliable reports of whether they currently have pain. Pain scale most commonly preferred by older adults is a verbal descriptor scale, rather than a visual analogue, face, or numerical scale. c. Due to age-related changes in pharmacokinetics, older adults do not tolerate some analgesics (Ferrell, 2004; McCaffery and Pasero, 1999): i. Propoxyphene-containing drugs carry an excess risk of central nervous system (CNS) adverse effects with limited analgesic benefit ii. Meperidine has a toxic metabolite that accumulates in older adults due to decreased renal function, which results in irritability or even seizures. Avoid repeated dosing if used at all. iii. Mixed agonist-antagonist analgesics should be avoided in older adults due to their unreliable efficacy and cognitive and cardiovascular effects iv. Nonsteroidal antiinflammatory drugs (NSAIDs) such as ibuprofen carry a high risk of gastrointestinal adverse effects with prolonged or regular use. Cyclooxygenase-2 inhibitors (e.g., celecoxib) carry a cardiovascular risk. v. Regular dosages of acetaminophen are preferred for osteoarthritis, but the total dose should not exceed 4 g/day. Some older adults have experienced hepatic damage at 3 g/day, so the minimum effective daily dose should be used. vi. Long-acting opioids (e.g., methadone) and amitriptyline (Elavil) should be avoided due to potential adverse effects 1. Advance directives: Legal in every state, but laws vary widely (Warm and Weismann, 2000) a. There are two types of advance directive: i. Living will: Written document that specifies a person’s wishes regarding medical care if the person becomes unable to communicate at the end of life ii. Health care power of attorney, also called the durable power of attorney for health care or health care agent: Appoints someone to make decisions if the patient is unable to communicate. A financial power of attorney is different and does not permit the holder to make health care decisions. b. Nurses can help patients understand advance directives (Douglas and Brown, 2002) 2. Syndrome of imminent death (Weisman, 2000) a. Progresses through three stages over 24 hours to 2 weeks i. Early stage: Either hypoactive or hyperactive delirium or increasing sleepiness, bed bound ii. Middle stage: Further decline in mental status; pooled oral secretions from loss of swallowing reflex results in “death rattle”; fever is common iii. Late stage: Coma; altered respiratory pattern—either fast (as high as 40 breaths/min) or slow; cold extremities b. Confirm treatment goals with the family when the syndrome is recognized. Discuss the removal of treatments that do not contribute to comfort. Scopolamine may be used to dry secretions (decrease death rattle) and morphine may be used to control rapid respirations (goal is 10 to 15 breaths/min). Provide meticulous mouth and skin care. During pregnancy, nearly every body system undergoes adaptations that protect the growing fetus and prepare the mother for delivery. Some changes appear early and continue throughout gestation; others occur later. Tables 11-3, 11-4, and 11-5 summarize some of the most significant normal changes that critical care nurses need to keep in mind. Box 11-1 defines some common obstetric abbreviations that may be encountered in obstetric patients’ charts. TABLE 11-5 Comparison of Hemodynamic Profiles in Pregnant and Nonpregnant Women 1. One of the leading causes of maternal morbidity and mortality, contributing to 30% of obstetric deaths. Definitions include subjective assessments of blood loss greater than standard norms, a 10% decline in hematocrit, and need for blood transfusion. a. Average blood loss for vaginal delivery, cesarean section, and cesarean hysterectomy is 500, 1000, and 1500 ml, respectively b. Management requires understanding normal delivery blood loss, the physiologic response to and common causes of postpartum hemorrhage, and appropriate interventions 2. Physiologic response to postpartum hemorrhage a. Pregnant patients adapt more effectively to blood loss due to increased red blood cell (RBC) mass, plasma volume, and cardiac output b. Early during hemorrhage, systemic vascular resistance rises to maintain blood pressure and perfusion of vital organs. If bleeding continues, vasoconstriction affords less support, which results in drops in blood pressure, cardiac output, and end-organ perfusion. Table 11-6 classifies the physiologic responses that occur at various stages of postpartum hemorrhage. TABLE 11-6 Postpartum Hemorrhage Classification and Physiologic Response From Gary D: Postpartum hemorrhage, New Manage Options 45(2):335, 2002. 3. Etiologic factors: Distinguished by the timing of the hemorrhage a. Early postpartum hemorrhage (within 24 hours of delivery) ii. Lower genital tract lacerations iii. Lower urinary tract lacerations iv. Retained placental fragments b. Late postpartum hemorrhage (24 hours to 6 weeks after delivery) a. History of precipitous or prolonged stages of labor, overstretching of the uterus, administration of medications (e.g., magnesium sulfate for pregnancy-induced hypertension), past placental retention, use of forceps or other intra-vaginal manipulations i. Draw blood for possible cross-matching and baseline laboratory values: Hemoglobin level, hematocrit, platelet count, fibrinogen level, prothrombin time, partial thromboplastin time ii. Estimate the volume of blood loss iii. Identify the cause of the hemorrhage (a) Uterine atony: Boggy, large uterus, clots, bleeding (b) Lacerations: Firm uterus, bright red blood, steady stream of unclotted blood (c) Hematoma: Firm uterus, bright red blood, extreme perineal-pelvic pain, unexplained tachycardia (d) Retained placental fragments: Placenta not delivered intact, uterus remains large, absence of pain, bright red blood 5. Patient care specific to obstetric patients (see Chapter 3 for hemorrhagic shock interventions) a. Assess the fundus: Determine the level of firmness and the placement of the fundus b. Include estimates of the amount of lochia in intake and output assessments c. Administer prescribed uterotonic medications, which are the basis of drug therapy for postpartum hemorrhage. Table 11-7 lists available pharmacologic therapies for hemorrhage. TABLE 11-7 Medications for Postpartum Hemorrhage IM, Intramuscular; IV, intravenous; IU, intrauterine; PO, by mouth; PR, per rectum. From Dildy GA: Postpartum hemorrhage: new management options, Clin Obstet Gynecol 4(2):330-344, 2002. 6. Evaluation: Desired patient outcomes include the following: 1. Definitions: Hypertension is defined as systolic blood pressure 30 mm Hg above baseline and diastolic blood pressure 15 mm Hg above baseline. In pregnancy, abnormal proteinuria is 300 mg protein or more in 24 hours. 2. Classification of hypertensive states in pregnancy a. Gestational hypertension: Occurs in the second half of pregnancy or the first 24 hours postpartum i. Mild: Systolic less than 160 mm Hg or diastolic less than 110 mm Hg, plus proteinuria less than 1+ on dipstick and less than 5 g in 24 hours ii. Severe: Systolic more than 160 mm Hg or diastolic more than 110 mm Hg, plus proteinuria of more than 5 g in 24 hours b. Preeclampsia, or pregnancy-induced hypertension (PIH): Occurs at more than 20 weeks’ gestation i. Mild: Mild hypertension and mild proteinuria ii. Severe: Severe hypertension and proteinuria with other symptoms including headache, visual changes, epigastric or right upper quadrant pain, and shortness of breath. May also include thrombocytopenia, pulmonary edema, and oliguria (< 500 ml in 24 hours). a. Characterized by vasoconstriction, hemoconcentration, and possible ischemic changes in the placenta, kidney, liver, and brain b. Intense vasoconstriction due to dysfunction of the normal interactions of vasodilatory and vasoconstrictive substances c. Thrombocytopenia: Platelet count lower than 100,000/mm3 d. Decreased renal perfusion and reduced glomerular filtration rate e. Hepatic system: Mildly elevated liver enzyme levels, subcapsular hematomas, or hepatic rupture i. Chronic vasoconstriction that occurs in PIH causes fibrin deposits in hepatic sinusoids, which obstruct hepatic blood flow and alter liver function ii. Liver swells, stretching Glisson’s capsule and producing epigastric and right upper abdominal quadrant pain iii. Hemorrhagic periportal necrosis, subcapsular hemorrhages, and spontaneous liver rupture may occur in extreme cases. Serum liver enzyme levels rise, with aspartate aminotransferase values of 60 IU or higher (normal ≥35 IU). Jaundice and acute hepatic failure may occur. iv. Maternal hypoglycemia is a serious prognostic indicator v. Risk of developing DIC is compounded: Patients with severe HELLP syndrome (all three abnormalities) are at greater risk for developing DIC than patients with partial HELLP syndrome (one or two clotting abnormalities). Despite treatment, the syndrome can escalate into DIC because the production of many clotting factors is increased in pregnancy (Table 11-9). With DIC, the clinical picture is hemorrhage and shock (see Chapter 7). TABLE 11-9 Comparison of HELLP Syndrome and Disseminated Intravascular Coagulation (DIC) HELLP, Hemolysis, elevated liver enzyme levels, and low platelet count. From Bridges EJ, Womble S, Wallace M, et al: Hemodynamic monitoring in high-risk obstetrics patients: I. Expected hemodynamic changes during pregnancy, Crit Care Nurse 23:53-62, 2003.
Critical Care Patients with Special Needs
INTRODUCTION
NURSING CARE OF THE CRITICALLY ILL BARIATRIC PATIENT
CARE OF THE MORBIDLY OBESE BARIATRIC SURGERY PATIENT
RELATED BARIATRIC CARE ISSUES
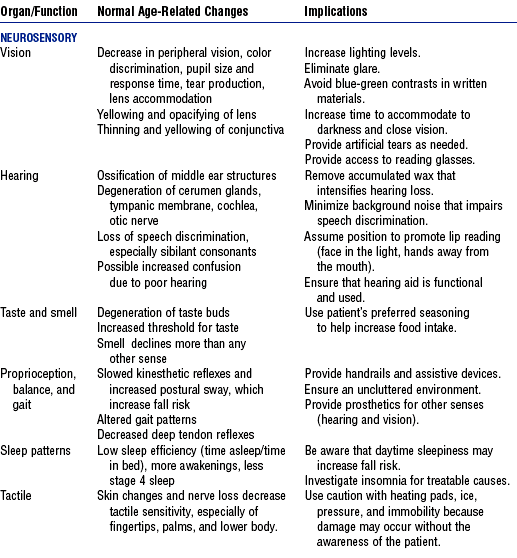
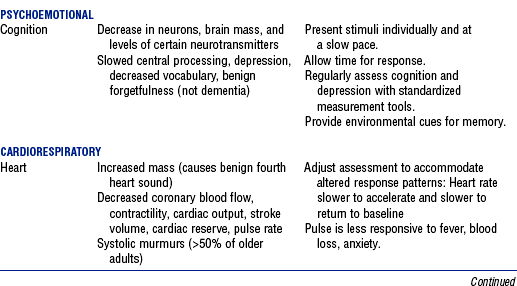
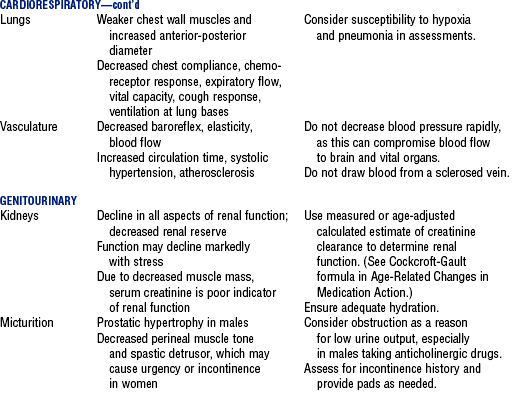
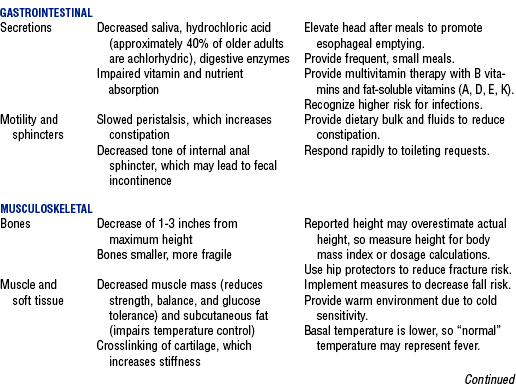
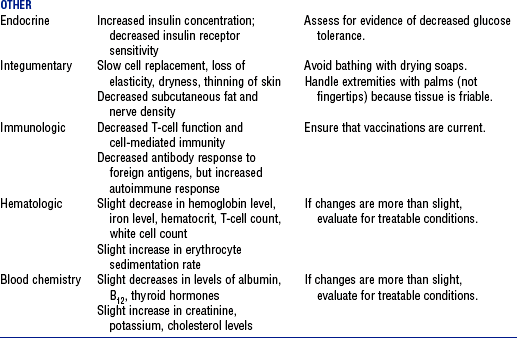
AGE-RELATED BIOLOGIC AND BEHAVIORAL DIFFERENCES
AGE-RELATED CHANGES IN MEDICATION ACTION
COMMON GERIATRIC SYNDROMES
END-OF-LIFE CARE
PHYSIOLOGIC CHANGES IN PREGNANCY
Hemodynamic Parameter
Pregnant
Nonpregnant
Cardiac output (L/min)
6.2
4.3
Central venous pressure (mm Hg)
3.7
3.6
Colloid osmotic pressure (mm Hg)
18
20.8
Heart rate (beats/min)
83
71
Left ventricular stroke index (ml/beat)
48
41
Mean arterial pressure (mm Hg)
90
86
Pulmonary capillary wedge pressure (mm Hg)
7.5
6.3
Pulmonary vascular resistance (dyne/sec/cm−5)
78
119
Systemic vascular resistance (dyne/sec/cm−5)
1210
1530
POSTPARTUM HEMORRHAGE
HYPERTENSIVE DISORDERS OF PREGNANCY
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree