Chapter 34 Contraception
Learning outcomes for this chapter are:
1. To identify contraceptive services available
2. To describe the role of the midwife in providing contraception counselling
3. To identify the factors that influence the selection of a suitable method of contraception for a woman or couple
4. To discuss the impact of culture, disability and pre-existing health problems on the choice of contraception
5. To explain the efficacy of various methods of contraception with typical and perfect use
6. To differentiate the changed patterns of contraceptive use at different times of a woman’s reproductive life
7. To describe the way in which the following methods of contraception act, the reasons they may be selected as a method, and their suitability for use during lactation and the postpartum period: lactational amenorrhoea method; fertility-awareness-based methods; barrier methods; intrauterine devices/systems; hormonal contraception; spermicides; vaginal douche; coitus interruptus; and sterilisation.
This chapter gives an overview of the methods of contraception used in Australia and New Zealand and will provide midwifery students with a beginning knowledge in this area. It is not within the scope of this chapter to provide complete information about each method of contraception. Rather, it should be viewed as an introduction to the methods with key points of information. Completion of a course offered at local family planning organisations and undertaking wider reading will provide additional invaluable information for midwives working with women in the antenatal and postnatal periods in particular.
INTRODUCTION
Attempts to control fertility have been documented throughout history and have included methods such as the insertion of objects (e.g. stones) into the vagina or uterus, douches made of carbonated beverages and plastic wrap to simulate the function of condoms (Varney 1997). Fortunately there are many more-efficacious methods of contraception available to women. In the 20th century Margaret Sanger, a nurse, made an important contribution to women’s quest for planning their families and the right of children to be born when they are wanted. She recognised the correlation between poverty and high birth rates and in 1952 founded the Planned Parenthood Federation of America. This organisation is now the International Planned Parenthood Federation (IPPF), and links national autonomous Family Planning Associations (FPAs) in over 180 countries worldwide.
CONTRACEPTION COUNSELLING: THE ROLE OF THE MIDWIFE
Unfortunately, provision of contraceptive information is often a hasty activity included in a checklist of other topics as part of discharge education in the postnatal ward (Glasier et al 1996). A Cochrane Review (Lopez et al 2010) concluded that there is not enough evidence to establish that current postpartum contraception education is effective, and that research is required to examine the best timing and approaches. Until such time as this is undertaken, it would be reasonable to assume that discussion about contraception should be initiated in the antenatal period and revisited in the postnatal period. It is important that the issue is adequately discussed, and in addition to provision of verbal and written information about contraceptive methods, referral to a primary healthcare provider for ongoing contraceptive needs is also essential. An up-to-date list of providers is a useful adjunct for counselling by the midwife.
Timely advice about contraception is critical because in the absence of breastfeeding, it is possible that ovulation may occur from day 28 postnatally (Guillebaud 2009). A number of factors will influence the method of contraception selected by a woman or couple. These include:
• whether the individual or couple is seeking a permanent or temporary method of contraception
• their understanding of the effectiveness of the method (see Table 34.1)
• the perceived or actual side-effects of the method
• the woman’s age and lifestyle
• previous positive or negative experience(s) of a method(s)
• the cost and convenience of the method
• the ease of use of particular methods
• the number of sexual partners
• the current popularity of a particular method
• the influence of the media, friends and family
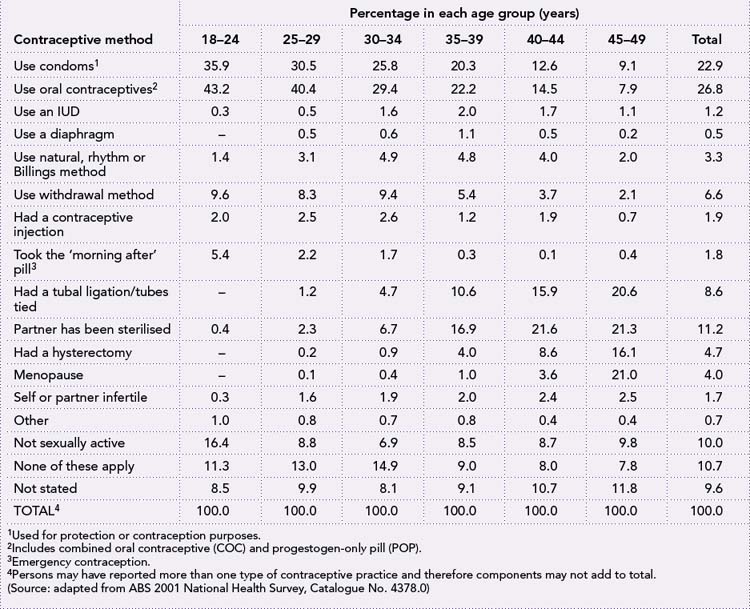
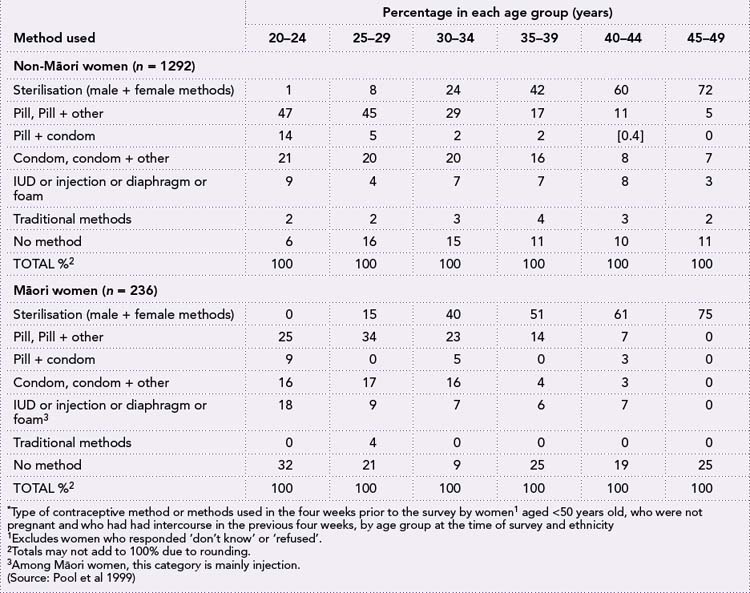
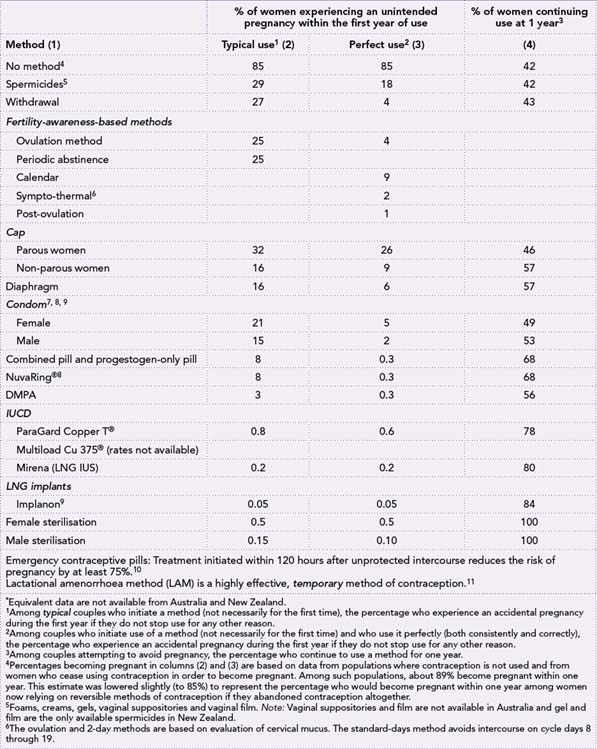
Choices of contraceptive method change at various times in the childbearing years, as exemplified in Tables 34.2 and 34.3. Information should be provided about the effectiveness of various methods, none of which are 100% effective other than non-reversible methods (see Table 34.1), their action, potential side-effects and the benefits and risks of the method as they relate to the individual woman. The time it takes for fertility to return after cessation of the method is also important when couples want to have more children, and whether the method also affords protection from sexually transmitted infections will be important for some women. Midwives should be aware of when particular methods can be commenced in the postpartum period, and their suitability during lactation. Some women have existing health problems that affect the suitability of some methods. These are summarised in the Appendix. In the past, most women with intellectual disabilities, particularly those who were institutionalised, had induced amenorrhoea using continuous progestogens or by surgical approaches (Grover 2002). Now, their choices are the same as for non-disabled women, with infrequent use of surgical intervention (Kaplan 2006).
Table 34.1 Percentage of women experiencing an unintended pregnancy during the first year of use of a contraceptive method and the percentage continuing use at the end of the first year, USA∗
Different cultural views about the use of contraception must also be respected by midwives when discussing ongoing contraceptive needs with women. It is not possible here to discuss each cultural group represented in Australia and New Zealand; however, it is important for midwives to be familiar with the cultural mores of the common groups of culturally and linguistically diverse (CALD) women in their care. These women (like other women in the dominant culture) may have poor knowledge of contraceptive methods from their schooling or teaching within the family, particularly where virginity is highly prized and expected until marriage. Information about contraception may be withheld as being more appropriate to be discussed at the time of marriage. Some groups of women may have had particular methods of contraception used without their informed consent and may be distrustful of all methods. Other women may be refugees or have migrated from countries where access to contraceptive services was limited or unavailable. Some women may have come from countries with pro-natalist policies, and others may have come from countries where limitations are placed on family size. When discussing contraception with CALD women, traditional values must be respected and dealt with sensitively. There must also be acknowledgement that women may want to move away from traditional approaches to contraception that may at times differ from the views of their partner and/or community.
The advice and information provided must be framed within the woman’s values and beliefs. It is important that the midwives or other healthcare professionals provide non-judgemental contraceptive advice and do not allow their own values to influence the advice they give to women. The midwife’s counselling role also needs to extend beyond advice about contraception. Although the birth of a baby can strengthen a relationship and perhaps enhance sexual intimacy, resumption of sexual intercourse may take several months. Hormonal changes can result in a low libido; there can be physical discomfort from an episiotomy, perineal tear or caesarean section, and physical and emotional exhaustion from sleepless nights and the demanding role of parenting, all of which can be worse if the woman has postnatal depression (Guillebaud 2009). Other issues include decreased lubrication from reduced oestrogen secretion; bloody lochia, which may interfere with sexual feelings; changed feelings about the erotic significance of the breasts; and adjustment of the relationship to include a new family member (Kennedy & Trussell 2007).
NATURAL METHODS OF CONTRACEPTION
Lactational amenorrhoea method (LAM)
Breastfeeding can provide a natural contraceptive effect and is a method that can be used when a woman is exclusively or near-exclusively breastfeeding for the first six months following a birth. Infant suckling at the breast inhibits ovulation, and although this is often attributed to high levels of prolactin, it is actually due to the disruption of the pulsatile release of gonadotrophic hormone (GnRH) by the hypothalamus, which in turn affects the pulsatility of luteinising hormone (LH) needed for follicle stimulation of the ovary. The small amounts of secreted oestrogen are insufficient to trigger the LH surge necessary to induce ovulation (Kennedy & Trussell 2007). LAM provides 98% protection against pregnancy in the first six months following birth if all of the following three criteria are met:
• The woman must breastfeed both day and night, providing a minimum of 90% of the infant’s nutritional requirements.
If supplements are given, they can only be non-milk (e.g. water and juice), given infrequently (no more than and preferably less than 5%–15%), and not via a bottle (Kennedy & Trussell 2007). This ensures maximum suckling stimulation of the breast. Interestingly, in one study, higher rates of pregnancy (5.2%) were seen in working women using LAM, which indicates that even in the presence of good milk production and full breastfeeding, it is frequent suckling—without expressing milk manually or using a pump—that is necessary to gain the maximum effect of LAM (Valdés et al 2000).
In Australia, 64.4% of infants are breastfed at three months of age (Donath & Amir 2008); however, breastfeeding rates are lower for Indigenous infants (ABS 2008). In New Zealand, 50.9% of infants are fully breastfed at three months; this rate is lower for Māori and Pacific Island infants (Ministry of Health 2002). If women were better informed about this contraceptive method, it could gain popularity and improve breastfeeding rates, although this requires good support for breastfeeding by the healthcare system, employers, and family and friends.
Fertility-awareness-based (FAB) methods
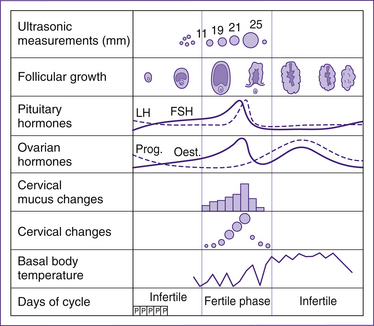
These methods, sometimes called ‘natural methods’ or ‘natural family planning’, use recognition of the changes in the woman’s body at various times of the menstrual cycle. They acknowledge that the estimation of the period of fertility needs to take into account the viability of sperm in the female genital tract—an average of three to four days with a theoretical possibility of up to seven days—and the fertile period of the ovum, which is estimated to be 24 hours (Guillebaud 2009).
Calendar (rhythm) method
The calendar method is the least reliable of these methods (see Table 34.1). It is based on the premise that ovulation occurs in the middle of the cycle and the fertile period lasts for six days—the five days before ovulation and the day of ovulation (Jennings & Arevalo 2007). Calendar methods are not particularly effective, and there are relatively few days in a cycle during which some women are not fertile, including the day of the cycle when they expect their next menstrual period (Wilcox et al 2000). These researchers found that only 30% of women were fertile in the period given in currently accepted clinical guidelines, that is, between days 10 and 17 of the cycle. Even for women who closely study their cycles to identify
shortest and longest cycle length, life events may disrupt predictions and alter the fertile period unexpectedly. Some women have less-regular cycles, which makes the method even less predictable. Refer to Guillebaud (2009, p 29), who outlines the way in which the fertile period is calculated, to maximise the effectiveness of this method.
Basal body temperature (BBT)
The BBT method is based on the fact that there is a drop in the woman’s body temperature 12 to 24 hours prior to ovulation, with a sustained rise for several days afterwards. Knowledge of temperature change is only useful in establishing when ovulation has already occurred over several cycles and thus the infertile period in which safe intercourse can occur. The temperature needs to be taken accurately each morning before the woman does any activity, using the same (oral, vaginal or rectal) route each time and charted on a temperature chart. The problem with relying on this method is that there is great individual variation in BBT, which can be affected by life events such as illness, emotional stress, irregular or disturbed sleep, oversleeping, gynaecological disorders, some medications, holidays and travel (Barron & Fehring 2005). Greater accuracy in predicting ovulation is available using ovulation detection kits (Nelson & Marshall 2007).
Cervical mucus charting (Ovulation or Billings method)
This method originated in Australia in the 1950s (Varney 1997). In this approach, the woman is taught to recognise her fertile days by both the appearance and sensation of mucus at the vulva. She learns to recognise the difference between feelings of wetness and dryness. The fertile mucus (Spinnbarkeit mucus) assists the sperm to enter the cervix and is produced under the influence of unopposed oestrogen in the follicular phase of the cycle (Guillebaud 2009). It is likely that ovulation occurs within a day before, during or one day after the last day of abundant slippery discharge (Jennings & Arevalo 2007). The method is most effective if the fertile period is considered to begin when there is any type of mucus noted before ovulation. Following ovulation, the mucus changes under the influence of progesterone in the luteal phase, becoming impenetrable and hostile to sperm, and sticky (Guillebaud 2009). A disadvantage of this method is that some women may not secrete adequate amounts of mucus to notice cyclic changes.
Sympto-thermal method
This method incorporates cervical mucus observation and BBT as described previously with additional indicators of ovulation. These include symptoms such as the recognition of the softening and lowering of the external cervical os at the time of ovulation by the woman palpating her cervix (Guillebaud 2009). Cervical palpation each day towards the end of lactation can be a useful adjunct to assist the woman to recognise the return of fertility when using the LAM method. Additional symptoms which may occur around the time of ovulation include: mittelschmerz pain caused by follicular rupture and resulting in symptoms such as dragging pain in the lower abdominal area; and rectal pain, which may occur before, during or after ovulation. Other symptoms may include increased libido, mood changes, breast tenderness and tenseness.
Breastfeeding considerations
The current WHO (2004, p 3) guidelines outline the following information in relation to FAB, which may be less effective when breastfeeding. Women who are primarily breastfeeding and are amenorrhoeic are unlikely to have sufficient ovarian function to produce fertility signs and hormonal changes during the first six months postpartum. After menses commences, when the woman notices fertility signs (particularly cervical secretions), she can use a symptoms-based method. Prior to that time, a barrier method should be offered if the woman plans to use a FAB method later.
Postpartum considerations
The current WHO (2004, p 3) guidelines outline the following information in relation to postpartum use of FAB.
After four weeks, non-breastfeeding women are likely to have sufficient ovarian function to produce detectable fertility signs and/or hormonal changes; and the likelihood increases rapidly with time postpartum. Women can use a calendar-based method as soon as they have completed three postpartum menses. Methods appropriate for the postpartum period should be offered prior to that time.
BARRIER METHODS
Male condom
This is a widely available and popular male method of contraception (see Tables 34.2 and 34.3) that is readily reversible. Male condoms are one-use-only sheaths most commonly made of latex (rubber). Polyurethane (plastic) condoms are also available but are more expensive than latex condoms. They are thinner and have a higher breakage rate than latex condoms, although they provide a good alternative for individuals with allergies, sensitivities or personal preferences that might prevent the use of latex condoms (Gallo et al 2006). In some countries, ‘lambskin’ condoms are available, and although they are effective as contraceptives, they are not effective in preventing the transmission of infections. They are not available in Australia or New Zealand.
Condoms rarely break or slip off, and provide high contraceptive efficacy if used correctly and consistently (Walsh et al 2004). Refer to Table 34.1 for efficacy of the method. Male condoms can be used alone or with a spermicide, and can also be used as an adjunct to other methods of contraception when there is a risk of STI transmission.
Condoms come in different colours and flavours, although some of these are ‘novelty’ condoms and are not safe to use to prevent pregnancy or transmission of STIs. It is important, therefore, that users check that the condoms are Australian or New Zealand standards approved where pregnancy and/or STI prevention are wanted. Condoms are available from many sources including supermarkets, pharmacies, vending machines, healthcare services and entertainment venues, and are reasonably cheap, particularly when bought in bulk. New Zealand midwives are licensed to prescribe condoms. Some manufacturers make wider and longer condoms, which suit men who find standard condoms uncomfortable. Condoms are most effective against STIs transmitted to and from the male urethra. These include HIV, gonorrhoea, chlamydia, trichomoniasis and hepatitis B. They are less effective against STIs transmitted by skin-to-skin contact or contact with mucosal surfaces, for example genital herpes, human papilloma virus and syphilis because the infected areas may not be covered by the condom (Warner & Steiner 2007).
Female condom (Femidom®)
The female condom is a loose polyurethane sheath (see Fig 34.2) that is inserted into the vagina. It has a 60 mm ring at one end that fits into the vaginal fornices in contact with the cervix (in much the same way as a diaphragm) and an outer ring 70 mm in diameter that is in contact with the vulva, preventing it from retracting into the vagina. Although female condoms are not as popular as male condoms, they will suit women who want to control the use of a condom, because they can insert the female condom up to eight hours ahead of time. Female condoms are pre-lubricated; however, additional lubricant can be used to assist in reducing the noise that generally accompanies their use during thrusting of the penis during vaginal intercourse. As with male condoms, female condoms afford protection against several STIs (Guillebaud 2009). Because they are made of polyurethane rather than latex, they can be used with oil-based lubricants. It is generally recommended that female condoms are one-use only.
Diaphragm
A diaphragm is a soft, latex dome with a flexible metal spring encased in the rim (see Fig 34.3). It is inserted into the vagina to cover the cervix and is used in conjunction with a teaspoon of spermicide in the dome, which is in contact with the cervix (Cook et al 2003). Diaphragms come in circumferences ranging from 70 mm to 90 mm. They also come in different varieties named for the type of spring that holds the diaphragm in position: flat spring (flat band of lightweight stainless steel), coil spring (flexible circular coil), and all-flex (combination of flat and coil spring). Flat-spring diaphragms are not currently available in Australia or New Zealand. The spring in the circumference of the dome springs back into shape when the diaphragm is in place and holds it in position. There are no randomised controlled trials providing evidence that diaphragms provide protection against infection; however, it is likely that they provide protection of the cervix from infection (Cates & Raymond 2007).
Diaphragms need to be correctly fitted by a qualified practitioner, and should be replaced after two years, after childbirth and if a woman gains or loses four or more kilograms in bodyweight. Failure of diaphragms is caused by poor fitting of the diaphragm, improper positioning and inconsistent use (Guillebaud 2009). Diaphragms are not suitable for all women, in particular those with a shallow pubic ledge and women with poor vaginal and/or perineal muscle tone; or with latex allergy. Women who choose this method must feel comfortable with their bodies and confident in inserting and removing the diaphragm from their vagina. They must be taught how to insert their diaphragm, check that it is in place and covering the cervix, the technique to remove the diaphragm and how to recognise when the diaphragm is no longer fitting correctly. Diaphragms can be inserted up to eight hours before intercourse and require the insertion of additional spermicide before subsequent intercourse. They need to be left in for six hours after intercourse because that is how long the spermicidal preparation takes to immobilise and kill the sperm. If intercourse takes place more than once within a six-hour period, the diaphragm should be left in place and more spermicide added using a plastic applicator. Diaphragms can be left in all the time, but must be removed every 24 hours and cleaned before replacing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree