Contact Layers
Action
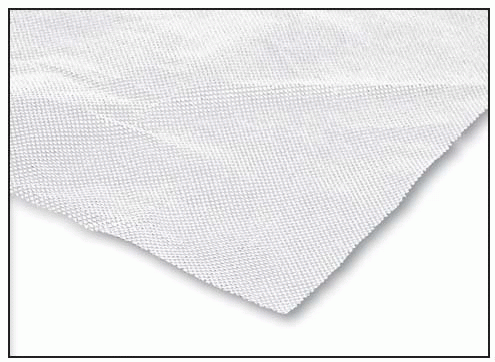
Contact layers are manufactured as single layers of a woven (polyamide) net that acts as a low-adherence material when placed in contact with the base of the wound. These materials allow wound exudate to pass to a secondary dressing. They may be used with topical medications. Contact layers aren’t intended to be changed with each dressing change.
Indications
Contact layers may be used as primary dressings for partial- and full-thickness wounds; wounds with minimal, moderate, and heavy exudate; donor sites; and split-thickness skin grafts.
Advantages
Can protect wound bases from trauma during dressing changes
May be applied with topical medications, wound fillers, or gauze dressings
Disadvantages
Are not recommended for stage 1 pressure ulcers; wounds that are shallow, dehydrated, or covered with eschar; or wounds that are draining a viscous exudate
Require secondary dressings
HCPCS code overview
The HCPCS codes normally assigned to contact layer dressings are: A6206—pad size ≤ 16 in2 A6207—pad size > 16 in2 but ≤ 48 in2 A6208—pad size > 48 in2
NEW PRODUCT
Adaptic Touch
Systagenix
How supplied
Open mesh contact layer: | 2″ × 3″, 3″ × 4 1/4″; A6206 |
5″ × 6″; A6207 | |
8″ × 12 3/4″; A6208 |
Action
Silicone assists dressing application and atraumatic removal; advanced mesh design means minimized risk of exudates pooling and secondary dressing adherence to wounds, reduced chance of maceration
 |
Indications
Indicated for use in the management of dry to heavily exuding, partial-and fullthickness chronic wounds, including venous ulcers, decubitus (pressure) ulcers, diabetic ulcers, traumatic and surgical wounds, donor sites and first-and seconddegree burns. It can be used under compression and in conjunction with negative pressure wound therapy (NPWT).
Contraindications
Not indicated for use with patients with a known sensitivity to silicone or cellulose acetate fabric or surgical implantation
Application
To prevent potential adherence of silicone to gloves, moisten gloves with a sterile solution to facilitate handling.
Prepare the wound according to wound management protocol.
Ensure skin surrounding the wound is dry.
If needed, ADAPTIC TOUCH may be cut to size with sterile scissors—leave one or two of the release papers in place when cutting.
Remove protective films from ADAPTIC TOUCH.
Place ADAPTIC TOUCH dressing directly over the wound and smooth in place around the wound.
ADAPTIC TOUCH should be applied as a single layer (no folding), as this will allow exudates to easily flow through into secondary layer.
If more than one piece of ADAPTIC TOUCH is required, ensure dressings overlap completely covering entire wound bed and surrounding edges to avoid secondary dressing adherence to the wound; however, overlap should be minimized to prevent occlusion of mesh.
Cover with an appropriate semi-occlusive secondary dressing, e.g., TIELLE Hydropolymer Dressing.
Conformant 2 Wound Veil
Smith & Nephew, Inc.
Wound Management
 |
How supplied
Sterile sheet: | 4″ × 4″; A6206 |
4″ × 12″; A6207 | |
12″ × 12″, 12″ × 24″, 24″ × 36″; A6208 | |
Sterile roll: | 3″ × 5 yards, 4″ × 3 yards, 6″ × 2 yards, 6″ × 4 yards; A6206 |
Action
Conformant 2 is a single, transparent, nonadherent wound veil made of perforated high-density polyethylene. It’s used to line wounds or to place under packing materials. It’s easy to remove and assists in the removal of other products placed over the veil. Because it’s transparent, Conformant 2 allows visualization of the wound bed.
Indications
To prevent skin breakdown and to manage pressure ulcers (stages 1 to 4), partial-and full-thickness wounds, infected and uninfected wounds, draining wounds, and red, yellow, or black wounds; may also be applied directly to the wound as a liner or used with any topical preparation or ointment
Contraindications
Contraindicated for tunneling wounds
Application
Place the sheet over the wound and surrounding tissue, and affi× it with tape or roll gauze.
Removal
Remove the tape or roll gauze.
Gently lift one corner of the sheet, and peel it back from the wound.
DERMANET Wound Contact
Layer
DeRoyal
How supplied
Sheet: | 3″ × 3″; A6206 |
5″ × 4″; A6207 | |
8″ × 10″, 20″ × 15″, 24″ × 36″; A6208 | |
Roll: | 6″ × 72″; A6208 |
 |
Action
DERMANET Wound Contact Layer is a lightweight net made from high-density polyethylene that forms a porous fine-mesh structure. It’s nonlinting, inert (totally nonreactive), soft, air- and fluid-permeable, and nonadherent. It conforms to the shapes of wounds and may be used as a primary dressing, coated with ointment for burns, or used as a liner for deep wounds that need to be packed (thus allowing easy removal of packing material).
Indications
For use as a primary dressing to protect burns, graft sites, donor sites, and granulating dermal ulcers and to line deep wounds before packing
Contraindications
None provided by the manufacturer
Application
After cleaning the wound and applying topical medications, as prescribed, carefully apply DERMANET Wound Contact Layer.
Cover the contact layer with a secondary dressing.
Alternatively, apply medications directly to DERMANET Wound Contact Layer, and place it over the wound before applying a cover dressing.
For deep, open wounds, line the wound with DERMANET Wound Contact Layer, pack the wound with appropriate packing material, and then apply a cover dressing.
Removal
Gently lift the dressing off or out of the wound.
Glucan II Wound Dressing
Brennen Medical, LLC
Action
The Glucan II Wound Dressing is a film-backed, mesh-reinforced wound dressing consisting of oat beta-glucan. This temporary wound dressing provides an optimum gas-permeable, semiocclusive covering for the wound site; decreases pain by providing a cover for sensory nerve terminals; reduces the need for painful dressing changes; decreases fluid loss; reduces heat loss; forms a barrier against bacterial contamination; may permit early physical therapy; and provides cover for donor sites. It may provide a soothing interface at the wound surface.
Indications
To manage partial-thickness burns, ulcers, donor sites, and other shallow or abrasive wounds; may be used as a wound covering immediately after initial cleansing and removal of broken blisters (unbroken blisters may be left intact)
Contraindications
Contraindicated for third-degree burns and for wounds with large amounts of eschar
Contraindicated on patients with sensitivity to plant extracts and patients with a history of multiple serum allergies
Application
Using aseptic technique, prepare the wound site. If necessary, debride or excise the wound, removing broken blisters, eschar, necrotic tissue, and foreign debris.
Apply the dressing to the wound surface. (Dressing is labeled “THIS SIDE UP.”) Smooth the Glucan II Wound Dressing into place on the wound surface to ensure intimate contact of the dressing with the wound. If necessary, moisten the dressing with sterile saline for easier manageability. Remove any wrinkles or creasing of the dressing.
Staples may be used when applying the dressing to donor sites.
Apply an absorbent dressing over the Glucan II Wound Dressing, and secure in place with a flexible net, gauze, or similar dressing.
Protect the wound from movement for 30 to 60 minutes after the dressing has been applied to ensure adherence to the wound. Dressing perforations allow normal wound drainage.
Inspect covered areas daily to detect the formation of purulent accumulations, suggesting infection. Take appropriate measures, possibly including removal of the dressing.
Abrupt temperature elevation may occasionally be observed immediately following the application of the Glucan II Wound Dressing. If the elevated temperature persists, an infection may be present and appropriate measures should be taken. Removal of the dressing may be indicated.
Removal
Inspect the wound after 24 hours to assess status.
Remove the absorbent outer dressing. Leave the Glucan II Wound Dressing open, or wrap lightly with a flexible net, gauze, or similar dressing. If any signs of infection are present, remove the Glucan II Wound Dressing, clean the wound site, and apply a new dressing. If the Glucan II Wound Dressing adheres to the wound and/or the wound is re-epithelializing, the dressing may remain on the wound as a simple barrier or protective dressing until healing is complete.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

