Chapter 34 Congenital Abnormalities
Definition and causes
Chromosome and gene abnormalities
Genetic disorders (Mendelian inheritance)
 A dominant gene will produce its effect even if present in only one chromosome of a pair. An autosomal dominant condition can usually be traced through several generations: for example, achondroplasia, osteogenesis imperfecta, adult polycystic kidney disease or Huntington’s chorea.
A dominant gene will produce its effect even if present in only one chromosome of a pair. An autosomal dominant condition can usually be traced through several generations: for example, achondroplasia, osteogenesis imperfecta, adult polycystic kidney disease or Huntington’s chorea.
 A recessive gene needs to be present in both chromosomes before producing its effect: for example, cystic fibrosis or phenylketonuria.
A recessive gene needs to be present in both chromosomes before producing its effect: for example, cystic fibrosis or phenylketonuria.
 In an X-linked recessive inheritance the condition affects males almost exclusively, although females can be carriers. X-linked recessive inheritance is responsible for conditions such as haemophilia A and B and Duchenne muscular dystrophy.
In an X-linked recessive inheritance the condition affects males almost exclusively, although females can be carriers. X-linked recessive inheritance is responsible for conditions such as haemophilia A and B and Duchenne muscular dystrophy.
Teratogenic causes
A teratogen is any agent that raises the incidence of congenital abnormality. The list of known and suspected teratogens is continually growing (Box 34.1).
Box 34.1 Known and suspected teratogens
Multifactorial causes
These stem from a genetic defect in addition to one or more teratogenic influences.
Gastrointestinal malformations
Most of the abnormalities affecting this system call for prompt surgical intervention.
Gastroschisis and exomphalos
Gastroschisis (Fig. 34.1) is a paramedian defect of the abdominal wall with extrusion of bowel that is not covered by peritoneum.

Fig. 34.1 Gastroschisis showing prolapsed intestine to the right of the umbilical cord.
(From Rennie & Roberton 1999, with permission of Churchill Livingstone.)
Immediate management of both is as follows:
Atresias
Oesophageal atresia
 The midwife should attempt to pass a wide orogastric tube but it may travel less than 10–12 cm.
The midwife should attempt to pass a wide orogastric tube but it may travel less than 10–12 cm.
 Radiography will confirm the diagnosis.
Radiography will confirm the diagnosis.
 The baby must be given no oral fluid but a wide-bore oesophageal tube should be passed into the upper pouch and connected to gentle continuous suction. Usually a double-lumen 10FG (Replogle) tube is used and the baby nursed head up.
The baby must be given no oral fluid but a wide-bore oesophageal tube should be passed into the upper pouch and connected to gentle continuous suction. Usually a double-lumen 10FG (Replogle) tube is used and the baby nursed head up.
 He or she should be transferred immediately to a paediatric surgical unit and continuous suction must be available throughout the transfer.
He or she should be transferred immediately to a paediatric surgical unit and continuous suction must be available throughout the transfer.
Cleft lip and cleft palate
Cleft lip may be unilateral or bilateral and is very often accompanied by cleft palate.
 If the defect is limited to unilateral cleft lip, breastfeeding is encouraged.
If the defect is limited to unilateral cleft lip, breastfeeding is encouraged.
 Where there is the additional problem of cleft palate, arranging for the baby to be fitted with an orthodontic plate may facilitate breastfeeding but will not afford the same stimulus as nipple to palate contact.
Where there is the additional problem of cleft palate, arranging for the baby to be fitted with an orthodontic plate may facilitate breastfeeding but will not afford the same stimulus as nipple to palate contact.
 Cup or spoon feeding is an alternative method, and if bottle feeding there is a wide variety of specially shaped teats available to accommodate the different sizes and positions of palate defects.
Cup or spoon feeding is an alternative method, and if bottle feeding there is a wide variety of specially shaped teats available to accommodate the different sizes and positions of palate defects.
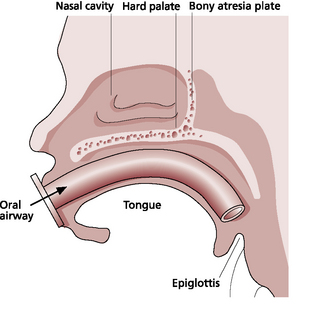
Abnormalities relating to respiration
Diaphragmatic hernia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree