Chapter 19 COMPONENTS OF THE NURSING PROCESS
Essentially the nursing process is a series of planned steps that produce a particular end result. Specifically, the nursing process is a modified scientific method of systematic problem solving. In simple terms the nursing process is a method used to assess the clients’ needs and plan, deliver and evaluate nursing care. The process of nursing, or scientific method of problem solving, remains the same whether the nursing care provided is a simple measure or a sequence of complicated nursing activities.
AN OVERVIEW OF THE NURSING PROCESS
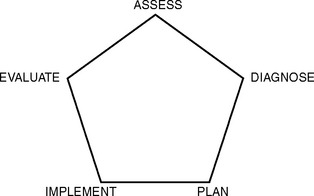
It is important for the nurse to recognise that the process is ongoing and cyclical in that each step relies on the step preceding and the step following. Figure 19.1 shows diagrammatic representation of the nursing process.
To meet clients’ changing needs it is essential to revise and update any plan of care continually. Using the nursing process, each individual’s specific needs are addressed, any problems are identified, and a care plan is developed and implemented to meet those needs. The effectiveness of any care given is continuously evaluated in terms of meeting clients’ needs (Alfaro-LeFevre 2005).
ASSESSMENT
Subjective data are the client’s, or other significant person’s, perceptions, ideas and sensations about a health problem. For example, a client may supply information about their sensations of a painful and itching skin, and state that they feel hot. Objective data are the pieces of information observed or measured by the nurse. For example, the nurse may observe the presence of a rash on the client’s body, and may then measure their temperature and observe that it is elevated. Methods of obtaining both subjective and objective data include the nursing history, physical examination and observation, and laboratory and diagnostic tests (Alfaro-LeFevre 2005).
The nursing history
A nursing history should be obtained as soon as possible after the client’s admission to the health care agency and should be conducted, when feasible, by the nurse with primary responsibility for planning the client’s care. Before beginning the interview the nurse must explain its purpose so the client understands why certain questions will be asked. The interview setting should be quiet and private for the client to feel comfortable about discussing personal details. If a client is too ill or is unable to communicate effectively (perhaps because of language barriers), a nursing history may be obtained by talking with a family member. It is important to record on the nursing assessment form from whom the information is obtained. The nurse may need to reassure the client that the conversation will be confidential (Crisp & Taylor 2005).
Physical examination and observation
The head-to-toe assessment involves assessing factors such as skin colour, general appearance, degree of mobility and independence, emotional status and the presence of obvious abnormalities, such as a rash. Information about the client’s general physical status is obtained by measuring body temperature, pulse, ventilations and blood pressure. The client’s weight (mass) and height are also measured and recorded. This information provides baseline data on which to assess the client’s present health status and may be useful for identifying actual or potential nursing problems (Jarvis 2008).
Cultural considerations in health assessment
Values provide the foundation for beliefs, attitudes and behaviours.
Heredity is any information concerning ethnic, cultural or racial heritage and is also important for assessing the person’s susceptibility to specific genetic disorders (Jarvis 2008).
Socioeconomic status is important in assessing health. Public health records show that people in lower socioeconomic groups have the highest rates of death and disease resulting from virtually every health problem. For more information on cultural diversity, see Chapter 9.
Laboratory and diagnostic tests
Laboratory and diagnostic tests, which are the most objective form of assessment data, provide another source of information about the client. Both subjective and objective data are required for comprehensive assessment of the client, as they provide more information than either could provide alone. For example, during the nursing interview a client may reveal that she feels tired constantly (subjective data). The nurse observes that she looks extremely pale and the laboratory test results indicate that her haemoglobin level is below normal (objective data). Thus, the laboratory test data provide verification of the alterations from normal (tiredness and pallor) identified during the interview. (See Clinical Interest Box 19.1 for a case study of the assessment phase.)
CLINICAL INTEREST BOX 19.1 Case study — the assessment phase
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree