Alanine aminotransferase
The alanine aminotransferase (ALT) test is used to measure serum levels of ALT, one of two enzymes that catalyze a reversible amino group transfer reaction in the Krebs cycle. ALT is necessary for energy production in tissues. It’s found primarily in the liver, with lesser amounts in the kidneys, heart, and skeletal muscles. ALT is a sensitive indicator of acute hepatocellular disease.
Purpose
♦ To detect acute hepatic disease, especially hepatitis and cirrhosis without jaundice, and evaluate its treatment
♦ To distinguish between myocardial and hepatic tissue damage (used with aspartate aminotransferase)
♦ To assess the hepatotoxicity of some drugs
Patient preparation
♦ Explain to the patient that this test is used to assess liver function.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Inform the patient that he need not restrict food or fluids.
Reference values
Serum ALT levels range from 10 to 40 U/L (SI, 0.17 to 0.68 µkat/L) in males and 7 to 35 U/L (SI, 0.12 to 0.60 µkat/L) in females.
Abnormal findings
Very high ALT levels (up to 50 times normal) suggest viral or severe druginduced hepatitis or other hepatic disease with extensive necrosis. Moderate to high levels may indicate infectious mononucleosis, chronic hepatitis, intrahepatic cholestasis or cholecystitis, early or improving acute viral hepatitis, or severe hepatic congestion as a result of heart failure.
Slight to moderate elevations of ALT may appear in any condition that produces acute hepatocellular injury, such as active cirrhosis and drug-induced or alcoholic hepatitis. Marginal elevations occasionally occur in acute myocardial infarction (MI), reflecting secondary hepatic congestion or the release of small amounts of ALT from myocardial tissue.
Aldosterone, serum
The aldosterone test measures serum aldosterone levels by quantitative analysis and radioimmunoassay. Aldosterone regulates ion transport across cell membranes to promote reabsorption of sodium and chloride in exchange for potassium and hydrogen ions. Consequently, it helps to maintain blood pressure and volume and regulate fluid and electrolyte balance.
This test identifies aldosteronism and, when supported by plasma renin levels, distinguishes between the primary and secondary forms of this disorder.
Purpose
♦ To aid in the diagnosis of primary and secondary aldosteronism, adrenal hyperplasia, hypoaldosteronism, and salt-losing syndrome
Patient preparation
♦ Explain to the patient that this test helps determine if symptoms are caused by improper hormonal secretion.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Instruct him to maintain a lowcarbohydrate, normal-sodium diet (135 mEq or 3 g/day) for at least 2 weeks or, preferably, for 30 days before the test.
♦ Withhold all drugs that alter fluid, sodium, and potassium balance—especially diuretics, antihypertensives, steroids, hormonal contraceptives, and estrogens—for at least 2 weeks or, preferably, for 30 days before the test, as ordered.
♦ Withhold all renin inhibitors for 1 week before the test, as ordered. If they must be continued, note this information on the laboratory request.
♦ Tell the patient to avoid licorice for at least 2 weeks before the test because it produces an aldosterone-like effect.
Reference values
Laboratory values vary with the time of day and with the patient’s posture— values are higher when patients are in an upright position. In upright individuals, a normal value is 7 to 30 ng/dl (SI, 0.19 to 0.83 nmol/L). In supine individuals, values are 3 to 16 ng/dl (SI, 0.08 to 0.44 nmol/L).
Abnormal findings
Excessive aldosterone secretion may indicate a primary or secondary disease. Primary aldosteronism (Conn’s syndrome) may result from adrenocortical adenoma or carcinoma or from bilateral adrenal hyperplasia. Secondary aldosteronism can result from renovascular hypertension, heart failure, cirrhosis of the liver, nephrotic syndrome, idiopathic cyclic edema, and the third trimester of pregnancy.
Low serum aldosterone levels may indicate primary hypoaldosteronism, salt-losing syndrome, eclampsia, or Addison’s disease.
Alkaline phosphatase
The alkaline phosphatase (ALP) test is used to measure serum levels of ALP, an enzyme that affects bone calcification as well as lipid and metabolite transport. ALP measurements reflect the combined activity of several ALP isoenzymes that are found in the liver, bones, kidneys, intestinal lining, and placenta. Bone and liver ALP is always present in adult serum, with liver ALP the most prominent except during the third trimester of pregnancy, when about half of all ALP originates in the placenta. The intestinal variant of ALP can be a normal component (found in less than 10% of normal patterns and almost exclusively in the sera of patients with blood groups B and O), or it can be an abnormal finding associated with hepatic disease.
Purpose
♦ To detect and identify skeletal diseases that are primarily characterized by marked osteoblastic activity
♦ To detect focal hepatic lesions that cause biliary obstruction, such as a tumor or abscess
♦ To assess the patient’s response to vitamin D in the treatment of rickets
♦ To supplement information from other liver function studies and GI enzyme tests
Patient preparation
♦ Explain to the patient that this test is used to assess liver and bone function.
♦ Instruct the patient to fast for at least 8 hours before the test because fat intake stimulates intestinal secretion of ALP.
♦ Explain that this test requires a blood sample, and tell the patient when and where it will be taken.
Reference values
Total ALP levels normally range from 25 to 100 U/L (SI, 0.43 to 1.70 mkat/L) in females older than 15 years and males older than 20 years.
Abnormal findings
Although significant elevations may occur with diseases that affect many
organs, an elevated ALP level usually indicates skeletal disease or extrahepatic or intrahepatic biliary obstruction causing cholestasis. Many acute hepatic diseases cause elevated ALP levels before they affect serum bilirubin levels.
Moderate increases in ALP levels may reflect acute biliary obstruction as a result of hepatocellular inflammation in active cirrhosis, mononucleosis, and viral hepatitis. Moderate increases also occur in osteomalacia and deficiencyinduced rickets.
Sharp elevations in ALP levels may indicate complete biliary obstruction by malignant or infectious infiltrations or fibrosis. These are most common in Paget’s disease and occasionally occur in biliary obstruction, extensive bone metastasis, and hyperparathyroidism. Metastatic bone tumors caused by pancreatic cancer increase ALP levels without a concomitant rise in serum ALT levels.
Isoenzyme fractionation and additional enzyme tests (gamma glutamyl transferase, lactate dehydrogenase [LD], 5-nucleotidase, and leucine aminopeptidase) are sometimes performed when the cause of ALP elevation is in doubt. Rarely, low levels of serum ALP are associated with hypophosphatasia and protein or magnesium deficiency.
Amylase, serum
An enzyme that’s synthesized primarily in the pancreas and salivary glands, amylase (alpha-amylase, or AML) helps to digest starch and glycogen in the mouth, stomach, and intestine. In cases of suspected acute pancreatic disease, measurement of serum or urinary AML is the most important laboratory test.
Purpose
♦ To diagnose acute pancreatitis
♦ To distinguish between acute pancreatitis and other causes of abdominal pain that require immediate surgery
♦ To evaluate possible pancreatic injury caused by abdominal trauma or surgery
Patient preparation
♦ Explain to the patient that this test is used to assess pancreatic function.
♦ Inform the patient that he need not fast before the test but must abstain from alcohol.
♦ Explain that this test requires a blood sample, and tell the patient when and where it will be taken.
Reference values
Normal serum AML levels range from 25 to 125 U/L (SI, 0.4 to 2.1 µkat/L) for adults age 18 and older.
Abnormal findings
After the onset of acute pancreatitis, AML levels begin to rise within 2 hours, peak within 12 to 48 hours, and return to normal within 3 to 4 days. Urine levels of AML should be measured after normal serum AML results are obtained to rule out pancreatitis. Moderate serum elevations may accompany obstruction of the common bile duct, pancreatic duct, or ampulla of Vater; pancreatic injury from a perforated peptic ulcer; pancreatic cancer; and acute salivary gland disease. Impaired kidney function may increase serum levels.
Levels may be slightly elevated in a patient who is asymptomatic or responds unusually to therapy.
Decreased levels can occur in chronic pancreatitis, pancreatic cancer, cirrhosis, hepatitis, and toxemia of pregnancy.
Antinuclear antibodies
In conditions such as systemic lupus erythematosus (SLE), scleroderma, and certain infections, the body’s immune system may perceive parts of its own cell nuclei as foreign and may produce antinuclear antibodies (ANAs). Specific ANAs include antibodies to deoxyribonucleic acid (DNA), nucleoprotein, histones, nuclear ribonucleoprotein, and other nuclear constituents.
Because they don’t penetrate living cells, ANAs are harmless, but they sometimes form antigen-antibody complexes that cause tissue damage (as in SLE). Because several organs may be involved, test results aren’t diagnostic and can only partially confirm clinical evidence.
Purpose
♦ To screen for SLE (The absence of ANAs essentially rules out active SLE.)
♦ To monitor the effectiveness of immunosuppressive therapy for SLE
Patient preparation
♦ Explain to the patient that this test evaluates the immune system and that further testing is usually required for diagnosis.
♦ Inform the patient that the test will be repeated to monitor his response to therapy, if appropriate.
♦ Inform the patient that he need not restrict food or fluids.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Check the patient’s history for drugs that may affect test results, such as isoniazid and procainamide. Note the findings on the laboratory request.
Reference values
Test results are reported as positive (with pattern and serum titer noted) or negative.
Abnormal findings
Although this test is a sensitive indicator of ANAs, it isn’t specific for SLE. Low titers may occur in patients with viral diseases, chronic hepatic disease, collagen vascular disease, and autoimmune diseases, and in some healthy adults; the incidence increases with age. The higher the titer, the more specific the test is for SLE. The titer commonly exceeds 1:256.
The pattern of nuclear fluorescence helps identify the type of immune disease present. A peripheral pattern is almost exclusively associated with SLE because it indicates anti-DNA antibodies; sometimes anti-DNA antibodies are measured by radioimmunoassay if ANA titers are high or if a peripheral pattern is observed. A homogeneous, or diffuse, pattern is also associated with SLE and related connective tissue disorders. A nucleolar pattern is associated with scleroderma, and a speckled, irregular pattern is associated with infectious mononucleosis and mixed connective tissue disorders (for example, SLE).
A single serum sample, especially one collected from a patient with collagen vascular disease, may contain antibodies to several parts of the nucleus of the cell. In addition, as serum dilution increases, the fluorescent pattern may change because different antibodies are reactive at different titers.
Arterial blood gas analysis
Arterial blood gas (ABG) analysis is used to measure the partial pressure of
arterial oxygen (PaO
2), the partial pressure of arterial carbon dioxide (PaCO
2), and the pH of an arterial sample. It also measures the oxygen content (O
2CT), arterial oxygen saturation (SaO
2), and bicarbonate (HCO
3 -) level. A blood sample for ABG analysis may be drawn by percutaneous arterial puncture or with an arterial line.
Purpose
♦ To evaluate the efficiency of pulmonary gas exchange
♦ To assess the integrity of the ventilatory control system
♦ To determine the acid-base level of the blood
♦ To monitor respiratory therapy
Patient preparation
♦ Explain to the patient that this test is used to evaluate how well the lungs are delivering oxygen to the blood and eliminating carbon dioxide.
♦ Tell the patient that the test requires a blood sample. Explain when and where the test will be performed and tell the patient which site—radial, brachial, or femoral artery—has been selected for the venipuncture.
♦ Inform the patient that he need not restrict food or fluids.
♦ Instruct the patient to breathe normally during the test, and warn him that he may have brief cramping or throbbing pain at the puncture site.
Reference values
Normal ABG values fall within the following ranges:
♦ PaO2: 80 to 100 mm Hg (SI, 10.6 to 13.3 kPa)
♦ PaCO2: 35 to 45 mm Hg (SI, 4.7 to 5.9 kPa)
♦ pH: 7.35 to 7.45 (SI, 7.35 to 7.45)
♦ O2CT: 15% to 23% (SI, 0.15 to 0.23)
♦ SaO2: 95% to 100% (SI, 0.95 to 1.00)
♦ HCO3 -: 22 to 26 mEq/L (SI, 22 to 26 mmol/L)
Abnormal findings
Low PaO2, O2CT, and SaO2 levels and a high PaCO2 may result from conditions that impair respiratory function, such as respiratory muscle weakness or paralysis, respiratory center inhibition (from head injury, brain tumor, or drug abuse), and airway obstruction (possibly from mucus plugs or a tumor). Similarly, low readings may result from obstruction of the bronchioles as a result of asthma or emphysema, from an abnormal ventilation-perfusion ratio caused by partially blocked alveoli or pulmonary capillaries, or from alveoli that are damaged or filled with fluid because of disease, hemorrhage, or near-drowning.
When inspired air contains insufficient oxygen, PaO2, O2CT, and SaO2 decrease, but PaCO2 may be normal. Such findings are common in pneumothorax, in patients with impaired diffusion between the alveoli and blood (as a result of interstitial fibrosis, for example), and in patients who have an arteriovenous shunt that permits blood to bypass the lungs.
Low O2CT—with normal PaO2, SaO2 and, possibly, PaCO2 values—may result from severe anemia, decreased blood volume, and reduced capacity to carry hemoglobin oxygen.
Aspartate aminotransferase
Aspartate aminotransferase (AST) is one of two enzymes that catalyze the conversion of the nitrogenous portion of an amino acid to an amino acid residue. It’s essential to energy production in the Krebs cycle. AST is found in the cytoplasm and mitochondria of many cells, primarily in the liver, heart, skeletal muscles, kidneys, pancreas, and red blood cells (RBCs). It’s released into serum in proportion to cellular damage.
Purpose
♦ To aid in the detection and differential diagnosis of acute hepatic disease
♦ To monitor the progress and prognosis of patients with cardiac and hepatic diseases
♦ To aid in the diagnosis of MI in correlation with creatine kinase (CK) and LD levels
Patient preparation
♦ Explain to the patient that this test is used to assess heart and liver function.
♦ Inform the patient that the test usually requires three venipunctures (one on admission and one each day for the next 2 days).
♦ Tell the patient that he need not restrict food or fluids.
Reference values
AST levels range from 14 to 20 U/L (SI, 0.23 to 0.33 µkat/L) in males and from 10 to 36 U/L (SI, 0.17 to 0.60 µkat/L) in females. In newborns, levels are 47 to 150 U/L (SI, 0.78 to 2.5 µkat/L). In children, they are 9 to 80 U/L (SI, 0.15 to 1.3 µkat/L).
Abnormal findings
AST levels fluctuate in response to the extent of cellular necrosis. They are transiently and minimally increased early in the disease process and extremely increased during the most acute phase. Depending on when the initial sample is drawn, AST levels may increase, indicating increasing severity of disease and tissue damage, or they may decrease, indicating resolution of disease and tissue repair.
Maximum elevations (more than 20 times normal) may indicate acute viral hepatitis, severe skeletal muscle trauma, extensive surgery, drug-induced hepatic injury, or severe passive liver congestion.
High levels (10 to 20 times normal) may indicate severe MI, severe infectious mononucleosis, or alcoholic cirrhosis. High levels may also occur during the prodromal and resolving stages of conditions that cause maximum elevations.
Moderate to high levels (5 to 10 times normal) may indicate dermatomyositis, Duchenne muscular dystrophy, or chronic hepatitis. Moderate to high levels also occur during the prodromal and resolving stages of diseases that cause high elevations.
Low to moderate levels (two to five times normal) occur at some time during the course of the conditions or diseases discussed earlier or may indicate hemolytic anemia, metastatic hepatic tumors, acute pancreatitis, pulmonary emboli, delirium tremens, or fatty liver. AST levels increase slightly after the first few days of biliary duct obstruction.
Bilirubin, serum
The bilirubin test is used to measure serum levels of bilirubin, the predominant pigment in bile. Bilirubin is the major product of Hb catabolism. Serum bilirubin measurements are especially significant in neonates because elevated unconjugated bilirubin can accumulate in the brain, causing irreparable damage.
Purpose
♦ To evaluate liver function
♦ To aid in the differential diagnosis of jaundice and monitor its progress
♦ To aid in the diagnosis of biliary obstruction and hemolytic anemia
♦ To determine whether a neonate requires an exchange transfusion or phototherapy because of dangerously high levels of unconjugated bilirubin
Patient preparation
♦ Explain to the patient that this test is used to evaluate liver function and the condition of RBCs.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Inform the adult patient that he need not restrict fluids but should fast for at least 4 hours before the test. (Fasting isn’t necessary for neonates.)
♦ If the patient is an infant, tell the parents that a small amount of blood will be drawn from his heel. Tell them who will be performing the heelstick and when it will be performed.
Reference values
In adults, the normal indirect serum bilirubin level is 1 mg/dl (SI, 17 µmol/L) and the direct serum bilirubin level is less than 0.5 mg/dl (SI, < 6.8 µmol/L). In neonates, the total serum bilirubin level is 2 to 12 mg/dl (SI, 34 to 205 µmol/L).
Abnormal findings
Elevated indirect serum bilirubin levels usually indicate hepatic damage. High levels of indirect bilirubin are also likely in severe hemolytic anemia. If hemolysis continues, levels of both direct and indirect bilirubin may rise. Other causes of elevated indirect bilirubin levels include congenital enzyme deficiencies such as Gilbert’s disease.
Elevated direct serum bilirubin levels usually indicate biliary obstruction. If the obstruction continues, both direct and indirect bilirubin levels may rise. In severe chronic hepatic damage, direct bilirubin concentrations may return to normal or near-normal levels, but indirect bilirubin levels remain elevated.
In neonates, total bilirubin levels of 15 mg/dl (SI, 257 µmol/L) or more indicate the need for an exchange transfusion.
Blood urea nitrogen
The blood urea nitrogen (BUN) test is used to measure the nitrogen fraction of urea, the chief end product of protein metabolism. Formed in the liver from ammonia and excreted by the kidneys, urea constitutes 40% to 50% of the nonprotein nitrogen in the blood. The BUN level reflects protein intake and renal excretory capacity but is a less reliable indicator of uremia than the serum creatinine level.
Purpose
♦ To evaluate kidney function and aid in the diagnosis of renal disease
♦ To aid in the assessment of hydration
Patient preparation
♦ Tell the patient that this test is used to evaluate kidney function.
♦ Inform the patient that he need not restrict food or fluids but should avoid a diet high in meat.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
Reference values
BUN values normally range from 8 to 20 mg/dl (SI, 2.9 to 7.5 mmol/L), with slightly higher values in elderly patients.
Abnormal findings
Elevated BUN levels occur in renal disease, reduced renal blood flow (as a result of dehydration, for example), urinary tract obstruction, and increased protein catabolism (such as burn injuries).
Low BUN levels occur in severe hepatic damage, malnutrition, and overhydration.
Calcium, serum
About 99% of the calcium in the body is found in the teeth. Approximately 1% of total calcium in the body circulates in the blood. Of this, about 50%
is bound to plasma proteins and 40% is ionized, or free. Evaluation of serum calcium levels measures the total amount of calcium in the blood, and ionized calcium measures the fraction of serum calcium that’s in the ionized form.
Purpose
♦ To evaluate endocrine function, calcium metabolism, and acid-base balance
♦ To guide therapy in patients with renal failure, renal transplant, endocrine disorders, malignancies, cardiac disease, and skeletal disorders
Patient preparation
♦ Explain to the patient that this test is used to determine blood calcium levels.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Inform the patient that he need not restrict food or fluids.
Reference values
Normally, total calcium levels range from 8.8 to 10.4 mg/dl (SI, 2.2 to 2.6 mmol/L) in adults and from 8.8 to 10.7 mg/dl (SI, 2.20 to 2.67 mmol/L) in children. Ionized calcium levels are 4.65 to 5.28 mg/dl (SI, 1.16 to 1.32 mmol/L).
Abnormal findings
Abnormally high serum calcium levels (hypercalcemia) may occur in hyperparathyroidism and parathyroid tumors, Paget’s disease of the bone, multiple myeloma, metastatic carcinoma, multiple fractures, and prolonged immobilization. Elevated levels may also result from inadequate excretion of calcium, such as in adrenal insufficiency and renal disease; from excessive ingestion of calcium; and from overuse of antacids such as calcium carbonate.
Low calcium levels (hypocalcemia) may result from hypoparathyroidism, total parathyroidectomy, and malabsorption. Decreased serum calcium levels may also occur with Cushing’s syndrome, renal failure, acute pancreatitis, peritonitis, malnutrition with hypoalbuminemia, renal failure, and blood transfusions (as a result of citrate).
In the patient with hypocalcemia, be alert for circumoral and peripheral numbness and tingling, muscle twitching, Chvostek’s sign (facial muscle spasm), tetany, muscle cramping, Trousseau’s sign (carpopedal spasm), seizures, arrhythmias, laryngeal spasm, decreased cardiac output, prolonged bleeding time, fractures, and prolonged Q interval.
Carcinoembryonic antigen
Carcinoembryonic antigen (CEA) is a protein that’s normally found in embryonic entodermal epithelium and fetal GI tissue. Production of CEA stops before birth, but it may begin again later if a neoplasm develops. Because biliary obstruction, alcoholic hepatitis, chronic heavy smoking, and other conditions also increase CEA levels, this test can’t be used as a general indicator of cancer. The measurement of enzyme CEA levels by immunoassay is useful for staging and monitoring the treatment of certain cancers.
Purpose
♦ To monitor the effectiveness of cancer therapy
♦ To assist in the preoperative staging of colorectal cancers, assess the adequacy of surgical resection, and test for recurrence of colorectal cancers
Patient preparation
♦ Explain to the patient that this test detects and measures a special protein that isn’t normally present in adults.
♦ Inform the patient that the test will be repeated to monitor the effectiveness of therapy, if appropriate.
♦ Inform the patient that he need not restrict food, fluids, or medications.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
Reference values
Normal serum CEA values are less than 5 ng/ml (SI, < 5 mg/L).
Abnormal findings
Persistent elevation of CEA levels suggests residual or recurrent tumor. If levels exceed normal before surgical resection, chemotherapy, or radiation therapy, a return to normal within 6 weeks suggests successful treatment.
High CEA levels are characteristic of various malignant conditions, particularly entodermally derived neoplasms of the GI organs and lungs, and of certain nonmalignant conditions, such as benign hepatic disease, hepatic cirrhosis, alcoholic pancreatitis, and inflammatory bowel disease.
Elevated CEA concentrations may occur in nonendodermal carcinomas, such as breast and ovarian cancers.
Cerebrospinal fluid analysis
For qualitative analysis, cerebrospinal fluid (CSF) is most commonly obtained by lumbar puncture (usually between the third and fourth lumbar vertebrae) and, rarely, by cisternal or ventricular puncture. A CSF specimen may also be obtained during other neurologic tests such as myelography.
Purpose
♦ To measure CSF pressure as an aid in detecting obstruction of CSF circulation
♦ To aid in the diagnosis of viral or bacterial meningitis, subarachnoid or intracranial hemorrhage, tumors, and brain abscesses
♦ To aid in the diagnosis of neurosyphilis and chronic central nervous system infections
♦ To aid in the diagnosis of dementia
Patient preparation
♦ Describe the procedure to the patient, and explain that this test analyzes the fluid around the spinal cord.
♦ Inform him that he need not restrict food or fluids.
♦ Tell him who will perform the procedure and where it will be performed.
♦ Advise the patient that a headache is the most common adverse effect of a lumbar puncture, but reassure him that his cooperation during the test helps to minimize this effect.
♦ Make sure that the patient or his legal guardian has signed the appropriate consent form.
♦ If the patient is unusually anxious, assess him and report his vital signs.
Normal findings
For a summary of normal and abnormal findings, see Findings in cerebrospinal fluid analysis.
Normally, CSF pressure is recorded and the appearance of the specimen is checked. Three tubes of CSF are collected routinely and are sent to the laboratory for analysis of protein, sugar, and cells as well as for serologic testing, such as the Venereal Disease Research Laboratory test for neurosyphilis. A separate specimen is sent to the laboratory for culture and sensitivity testing. Electrolyte analysis and Gram stain may be ordered as supplementary tests. CSF electrolyte levels are of special interest in patients with abnormal serum electrolyte levels or CSF infection and in those receiving hyperosmolar agents.
Chloride, serum
The chloride test is used to measure serum levels of chloride, the major extracellular fluid anion. Chloride helps maintain the osmotic pressure of blood and, therefore, helps regulate blood volume and arterial pressure. Chloride levels also affect the acid-base balance. Chloride is absorbed from the intestines and excreted primarily by the kidneys.
Purpose
♦ To detect an acid-base imbalance (acidosis or alkalosis) and to aid in the evaluation of fluid status and extracellular cation-anion balance
Patient preparation
♦ Explain to the patient that this test is used to evaluate the chloride content of blood.
♦ Explain that the test requires a blood sample, and tell the patient when it will be taken.
♦ Inform the patient that he need not restrict food or fluids.
Reference values
Normally, serum chloride levels range from 98 to 108 mEq/L (SI, 98 to 108 mmol/L) in adults.
Abnormal findings
Chloride levels are inversely related to bicarbonate levels, reflecting the acidbase balance. Excessive loss of gastric juices or other secretions that contain chloride may cause hypochloremic metabolic alkalosis; excessive retention or ingestion of chloride may lead to hyperchloremic metabolic acidosis.
Increased blood chloride levels occur in patients with severe dehydration, complete renal shutdown, head injury (producing neurogenic hyperventilation), and primary aldosteronism.
Decreased blood chloride levels occur in patients with low sodium and potassium levels as a result of
prolonged vomiting, gastric suctioning, intestinal fistula, chronic renal failure, and Addison’s disease. Heart failure or edema resulting in excess extracellular fluid can cause dilutional hypochloremia.
Cholesterol, total
The total cholesterol test, the quantitative analysis of serum cholesterol, is used to measure the circulating levels of free cholesterol and cholesterol esters. It reflects the level of the two forms in which this biochemical compound appears in the body. High serum cholesterol levels may be associated with an increased risk of coronary artery disease (CAD).
Purpose
♦ To assess the risk of CAD
♦ To evaluate fat metabolism
♦ To aid in the diagnosis of nephrotic syndrome, pancreatitis, hepatic disease, hypothyroidism, and hyperthyroidism
♦ To assess the efficacy of lipid-lowering drug therapy
Patient preparation
♦ Explain to the patient that this test is used to assess the body’s fat metabolism.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Instruct the patient not to eat or drink for 12 hours before the test, but inform him that he may have water.
Reference values
Total cholesterol concentrations vary with age and sex. Total cholesterol values are:
♦ adults: desirable, less than 200 mg/dl (SI, < 5.18 mmol/L)
♦ children ages 12 to 18: desirable, less than 170 mg/dl (SI, < 4.40 mmol/L).
Abnormal findings
Elevated serum cholesterol levels (hypercholesterolemia) may indicate a risk of CAD as well as incipient hepatitis, lipid disorders, bile duct blockage, nephrotic syndrome, obstructive jaundice, pancreatitis, and hypothyroidism.
Low serum cholesterol levels (hypocholesterolemia) are commonly associated with malnutrition, cellular necrosis of the liver, and hyperthyroidism. Patients who have abnormal cholesterol levels typically must undergo further testing to pinpoint the cause.
Creatine kinase
CK is an enzyme that catalyzes the creatine-creatinine metabolic pathway in muscle cells and brain tissue. Because of its intimate role in energy production, CK reflects normal tissue catabolism. Increased serum levels indicate trauma to cells.
Fractionation and measurement of three distinct CK isoenzymes—CK-BB (CK1), CK-MB (CK2), and CK-MM (CK3)—have replaced the use of total CK levels to localize the site of increased tissue destruction. CK-BB is most commonly found in brain tissue. CK-MM and CK-MB are found primarily in skeletal and heart muscle. In addition, subunits of CK-MB and CK-MM, called isoforms or isoenzymes, can be assayed to increase the sensitivity of the test.
Purpose
♦ To detect and diagnose acute MI and reinfarction (CK-MB is primarily used.)
♦ To evaluate possible causes of chest pain and to monitor the severity of myocardial ischemia after cardiac surgery, cardiac catheterization, and cardioversion (CK-MB is primarily used.)
♦ To detect early dermatomyositis and musculoskeletal disorders that aren’t neurogenic in origin such as Duchenne muscular dystrophy (Total CK is primarily used.)
Patient preparation
♦ Explain to the patient that this test is used to assess myocardial and musculoskeletal function and that multiple blood samples are required to detect fluctuations in serum levels.
♦ Tell the patient when and where the blood samples will be taken.
♦ If the patient is being evaluated for musculoskeletal disorders, advise him to avoid exercising for 24 hours before the test.
Reference values
Total CK values determined by ultraviolet or kinetic measurement range from 38 to 174 U/L (SI, 0.63 to 2.90 µkat/L) for men and from 26 to 140 U/L (SI, 0.46 to 2.38 µkat/L) for women. CK levels may be significantly higher in muscular people. Infants up to age 1 have levels two to four times higher than adult levels, possibly reflecting birth trauma and striated muscle development. Normal ranges for isoenzyme levels are as follows: CK-BB, undetectable; CK-MB, less than 6% (SI, < 0.06); CK-MM, 90% to 100% (SI, 0.90 to 1.00).
Abnormal findings
CK-MM makes up 99% of the total CK that’s normally present in serum. Detectable CK-BB isoenzyme may indicate, but doesn’t confirm, a diagnosis of brain tissue injury, widespread malignant tumors, severe shock, or renal failure.
CK-MB levels greater than 6% of the total CK level indicate MI, especially if the LD isoenzyme ratio is greater than 1 (flipped LD). In acute MI and after cardiac surgery, CK-MB begins to increase within 2 to 4 hours, peaks within 12 to 24 hours, and usually returns to normal within 24 to 48 hours. Persistent elevations and increasing levels indicate ongoing myocardial damage. The total CK level follows roughly the same pattern but increases slightly later. CK-MB levels may not increase in heart failure or during angina pectoris that’s not accompanied by myocardial cell necrosis. Serious skeletal muscle injury that occurs in certain muscular dystrophies, polymyositis, and severe myoglobinuria may cause a mild increase in CK-MB because a small amount of this isoenzyme is present in some skeletal muscles.
CK-MM values increase after skeletal muscle damage as a result of trauma, such as surgery and I.M. injections, and from diseases, such as dermatomyositis and muscular dystrophy (values may be 50 to 100 times normal). CK-MM levels increase moderately in patients with hypothyroidism; sharp increases occur with muscle activity caused by agitation, such as during an acute psychotic episode.
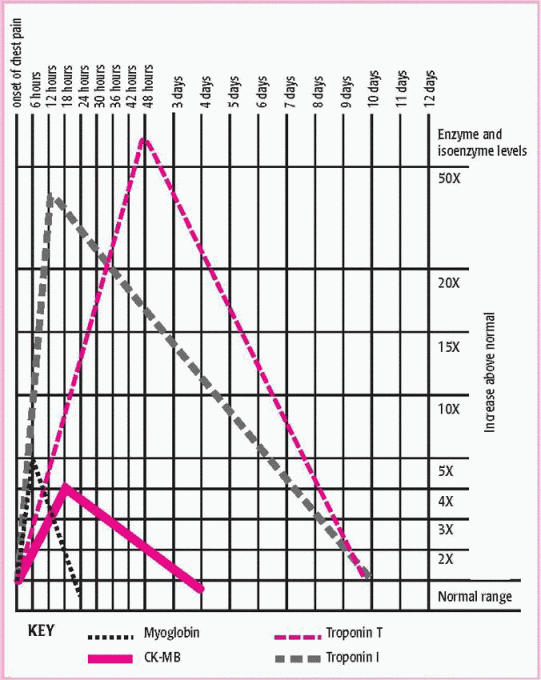
Total CK levels may be increased in patients with severe hypokalemia, carbon monoxide poisoning, malignant hyperthermia, and alcoholic cardiomyopathy. They may also be increased after seizures and, occasionally, in patients who have had pulmonary or cerebral infarctions. Troponin I and cardiac troponin C are present in the contractile cells of cardiac myocardial tissue and are released when myocardial tissue is injured. Troponin levels increase within 1 hour of infarction and may remain elevated for as long as 14 days. (See Serum protein and isoenzyme levels after MI.)
Creatinine, serum
Analysis of serum creatinine levels provides a more sensitive measure of renal damage than BUN levels. Creatinine is a nonprotein end product of creatine metabolism that appears in serum in amounts proportional to muscle mass.
Purpose
♦ To assess glomerular filtration
♦ To screen for renal damage
Patient preparation
♦ Explain to the patient that this test is used to evaluate kidney function.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Instruct the patient that he need not restrict food or fluids.
Reference values
Creatinine concentrations normally range from (0.9 to 1.3 mg/dl (SI, 80 to 115 µmol/L) in men and 0.6 to 1.1 mg/dl (SI, 53 to 97 µmol/L) in women.
Abnormal findings
Elevated serum creatinine levels usually indicate renal disease that has seriously damaged 50% or more of the nephrons. Elevated levels may also be associated with gigantism and acromegaly.
Creatinine clearance
An anhydride of creatine, creatinine is formed and excreted in constant amounts by an irreversible reaction. It functions solely as the main end product of creatine. Creatinine production is proportional to total muscle mass and is relatively unaffected by urine volume, normal physical activity, or diet.
Creatinine clearance is an excellent diagnostic indicator of renal function. The test determines how efficiently the kidneys are clearing creatinine from the blood. The rate of clearance is expressed in terms of the volume of blood (in milliliters) that can be cleared of creatinine in 1 minute. Creatinine levels become abnormal when more than 50% of the nephrons have been damaged.
Purpose
♦ To assess renal function (primarily glomerular filtration)
♦ To monitor the progression of renal insufficiency
Patient preparation
♦ Explain to the patient that this test assesses kidney function.
♦ Inform the patient that he may need to avoid meat, poultry, fish, tea, or coffee for 6 hours before the test.
♦ Advise the patient to avoid strenuous physical exercise during the collection period.
♦ Tell the patient that the test requires a timed urine specimen and at least one blood sample.
♦ Tell the patient how the urine specimen will be collected, and inform him when and where the blood sample will be taken.
Reference values
Normal creatinine clearance varies with age; in men, it ranges from 94 to 140 ml/min/1.73 m2 (SI, 0.91 to 1.35 ml/s/m2); in women, 72 to 110 ml/min/1.73 m2 (SI, 0.69 to 1.06 ml/s/m2).
Abnormal findings
Low creatinine clearance may result from reduced renal blood flow (associated with shock or renal artery obstruction), acute tubular necrosis, acute or chronic glomerulonephritis, advanced bilateral chronic pyelonephritis,
advanced bilateral renal lesions (which may occur in polycystic kidney disease, renal tuberculosis, and cancer), nephrosclerosis, heart failure, or severe dehydration.
High creatinine clearance can suggest poor hydration.
Erythrocyte sedimentation rate
The erythrocyte sedimentation rate (ESR) measures the degree of erythrocyte settling that occurs in a blood sample during a specified amount of time. The ESR is a sensitive but nonspecific test that’s commonly the earliest indicator of disease when other chemical or physical signs are normal. The ESR usually increases significantly in widespread inflammatory disorders; elevations may be prolonged in localized inflammation and malignant disease.
Purpose
♦ To monitor inflammatory or malignant disease
♦ To aid in the detection and diagnosis of occult disease, such as tuberculosis, tissue necrosis, or connective tissue disease
Patient preparation
♦ Explain to the patient that this test is used to evaluate the condition of RBCs.
♦ Explain that a blood sample will be needed, and tell the patient when and where it will be taken.
♦ Inform the patient that he need not restrict food or fluids.
Reference values
The ESR normally ranges from 0 to 15 mm/hour (SI, 0 to 15 mm/hour) in men and 0 to 20 mm/hour (SI, 0 to 20 mm/hour) in women. Rates gradually increase with age.
Abnormal findings
The ESR increases in pregnancy, anemia, acute or chronic inflammation, tuberculosis, paraproteinemias (especially multiple myeloma and Waldenström’s macroglobulinemia), rheumatic fever, rheumatoid arthritis, and some cancers.
Polycythemia, sickle cell anemia, hyperviscosity, and low plasma fibrinogen or globulin levels tend to depress the ESR.
Estrogens
Estrogens (and progesterone) are secreted by the ovaries. These hormones are responsible for the development of secondary female sexual characteristics and for normal menstruation. Levels are usually undetectable in children. These hormones are secreted by the ovarian follicular cells during the first half of the menstrual cycle and by the corpus luteum during the luteal phase and during pregnancy. In menopause, estrogen secretion drops to a constant, low level.
This radioimmunoassay measures serum levels of estradiol, estrone, and estriol (the only estrogens that appear in serum in measurable amounts) and has diagnostic significance in evaluating female gonadal dysfunction. (See
Predicting premature labor, page 164.) Tests of hypothalamic-pituitary function may be required to confirm the diagnosis.
Purpose
♦ To determine sexual maturation and fertility
♦ To aid in the diagnosis of gonadal dysfunction, such as precocious or delayed puberty, menstrual disorders (especially amenorrhea), and infertility
♦ To determine fetal well-being
♦ To aid in the diagnosis of tumors that are known to secrete estrogen
Patient preparation
♦ Tell the patient that this test helps determine if the secretion of female hormones is normal, and explain that the test may be repeated during the various phases of the menstrual cycle.
♦ Tell the patient that she need not restrict food or fluids.
♦ Explain that the test requires a blood sample, and tell the patient when and where it will be taken.
♦ Withhold all steroid and pituitarybased hormones, as ordered. If they must be continued, note this on the laboratory request.
Reference values
Normal serum estrogen levels for premenopausal women vary widely during the menstrual cycle, ranging from 26 to 149 pg/ml (SI, 90 to 550 pmol/L). The range for postmenopausal women is 0 to 34 pg/ml (SI, 0 to 125 pmol/L).
Serum estrogen levels in men range from 12 to 34 pg/ml (SI, 40 to 125 pmol/L). In children younger than age 6, the normal level of serum estrogen is 3 to 10 pg/ml (SI, 10 to 36 pmol/L).
During pregnancy, the placenta secretes large amounts of estriol. Levels range from 2 ng/ml (SI, 7 nmol/L) by week 30 to 30 ng/ml (SI, 105 nmol/L) by week 40.