Chapter 21. CNS 4. Antidepressants and dementias
Depression279
Psychosocial causes of clinical depression 280
Brain neuro transmitters and depression 280
Tricyclic antidepressants 280
Tricyclic anxiolytics 281
Selective serotonin (5-HT) reuptake inhibitors – SSRIs 282
Monoamine oxidase inhibitors (MAOIs) 282
Other antidepressants 283
Lithium 283
The management of depression (see also Culpepper 2002) 284
Electroconvulsive therapy 285
Summary287
At the end of this chapter, the reader should be able to:
• list the different types of depression and discuss brain neurotransmitters in depression
• give an account of the different groups of drugs used to treat depression and examples of such
• describe the adverse effects of tricyclic antidepressants and appreciate the dangers associated with MAOI drugs, particularly interactions with food and other drugs
• describe what SSRI drugs are and know examples
• provide the names of the other antidepressants mentioned
• explain what ECT is
• explain what lithium is, the preparations and when it is prescribed, and describe the dangers associated with using lithium, and the importance of monitoring blood levels of the drug
• give an account of the management of dementias and the drugs used to treat Alzheimer’s disease
Depression
Depression is a common and normal emotion and people naturally become depressed as a result of unfortunate domestic and social conditions. Sometimes, however, the depression is disproportionate to the precipitating factors or there may be no obvious cause at all. This is an illness called endogenous or psychotic depression and is commoner in older people. Some psychiatrists recognize a further type of depressive illness, in which environmental factors play a more prominent part, and this is sometimes called reactive depression or depressive neurosis. Sometimes, depression may alternate with attacks of mania. This is known as bipolar depression or manic-depressive psychosis.
In depression the mood is at its lowest in the morning and improves throughout the day. The patient is disinterested and may be irritable and anxious. The appetite is poor, and vague symptoms, including headache and odd pains, are common. Suicide is a special risk in depressed patients.
Psychosocial causes of clinical depression
Clinical depression may possibly be an eventual result in some individuals who experience, for example:
• prolonged periods of daylight shortening (seasonal affective disorder, possibly caused by increased brain melatonin)
• chronic illness
• bereavement or other forms of family crisis
• chronic unemployment.
Brain neurotransmitters and depression
The aetiology of depression is not known but there is evidence that a major factor is a reduction in the amount of neurotransmitter amines such as 5-HT (5-hydroxytryptamine; serotonin) or noradrenaline at the junctions between neurones in the brain. Many of the drugs used to treat depression increase the amount of these substances in the brain, thus providing some evidence that amines are connected with changes of mood.
The following groups of drugs are used to relieve depression:
• tricyclic antidepressants
• tricyclic anxiolytics
• selective serotonin reuptake inhibitors (SSRIs)
• monoamine oxidase inhibitors (MAOIs)
• lithium
• other antidepressants.
Tricyclic antidepressants
Tricyclic antidepressants comprise:
• amytriptyline
• clomipramine
• desipramine
• imipramine
• lofepramine
• nortriptyline
• protriptyline.
Clearly there are several tricyclic antidepressants in use and there is not a great deal of difference between them. Therefore a few representative drugs will be considered here. They are well absorbed after oral administration and undergo considerable breakdown in the liver; some of these metabolic products are therapeutically active. It is believed that they produce their therapeutic effect by preventing the reuptake of amines at nerve endings in the brain, which thus increases the concentration of these substances available for receptor uptake (Fig. 21.1).
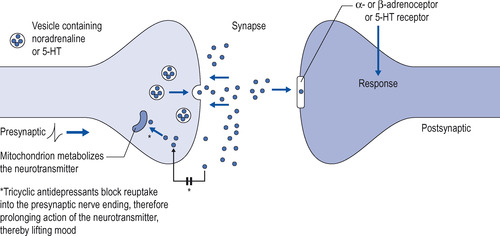 |
| Figure 21.1 Mechanism of action of the tricyclic antidepressants. |
Some members of the group (i.e. nortriptyline and desipramine) have a greater effect on noradrenaline concentration, and others (e.g. imipramine and amitriptyline) on 5-HT concentration.
Imipramine and amytriptyline
Imipramine was the first of these drugs to be used. Amitriptyline is very similar to imipramine but is rather more sedating. Both these drugs have a long action and need only be given once a day. If amitriptyline is given in the evening, its sedative action will help sleep, which is often disturbed in depression. Imipramine is actually a prodrug and is metabolized to the active drug, namely, desipramine (see above).
Therapeutic use
After starting treatment, the sleep disorders associated with depression usually respond fairly quickly, but it is important to remember that it may take several weeks before thedepression itself is relieved. Treatment should therefore be continued for 6 weeks before deciding that treatment has failed. About 80% of depressed patients will ultimately respond. Tricyclic antidepressants are also used in the treatment of pain of obscure origin, such as atypical facial pain.
Bedwetting
Plasma concentrations
Owing to the considerable interpersonal variation in the breakdown of these drugs, plasma levels may vary widely. Extensive investigation has been carried out on the measurement of plasma levels to control treatment but it is doubtful whether this is helpful in controlling dosage.
Adverse effects of tricyclic antidepressants
• Anticholinergic effects: dry mouth can be troublesome and may be mitigated by lemon juice. Elderly male patients may experience difficulty with micturition, and constipation can be a problem, particularly in depressed patients already preoccupied with their bowels. Owing to a dilating effect on the pupil of the eye, they should not be given to patients with glaucoma.
• Postural hypotension: this is a fall in blood pressure with occasional faintness, especially in elderly patients.
• Increased appetite and weight gain.
• In epilepsy: in patients with epilepsy, the tendency to seizures is increased and the dose of antiepileptic drugs may require alteration if tricyclic antidepressants are used.
• Heart: tricyclic antidepressants depress conduction in the heart, and a number of sudden deaths have been reported in patients with heart disease taking these drugs. They are therefore best avoided in this group of patients.
• Overdose: tricyclic antidepressants are dangerous in overdose, producing cardiovascular disturbance, seizures and coma.
• Withdrawal symptoms develop if the drug is stopped suddenly (see below).
Drug interactions
Interactions with other drugs occur, including antiepileptics, sympathomimetic drugs (but not local anaesthetics) and with other antidepressants and MAOIs. They may reverse the effect of some hypotensive agents and their action is enhanced by alcohol, so care should be taken when combining tricyclics with other drugs.
Tricyclic anxiolytics
Doxepin and dosulepin are similar to the tricyclic antidepressants, but have a weaker antidepressant action and are particularly useful when anxiety complicates mild depression. They are also more rapidly effective than the standard tricyclics. Adverse effects are similar to those of the tricyclics but generally less marked. They are still dangerous in overdose.
Maprotiline is not a tricyclic drug, but is an amine reuptake inhibitor. Its action and adverse effects profile is very similar to that of the tricyclics. It is also cardiotoxic.
• Patients must understand that the response to treatment may be delayed by up to 6 weeks with tricyclics.
• They may be told of the possible adverse effects and how to make the best of them.
• They must be informed of the important interactions and how to avoid them.
• They must realize that most of the drugs are dangerous in overdose.
Selective serotonin (5-HT) Reuptake inhibitors – SSRIs
5-HT is concerned with mood and behaviour and a deficiency of 5-HT in the brain is believed to be a factor in depression. Several drugs have been introduced which specifically inhibit 5-HT reuptake at nerve junctions and thus raise its concentration in the brain. Those available at present are:
• citalopram
• escitalopram
• fluoxetine
• fluvoxamine
• paroxetine
• sertraline.
In relieving depression these drugs are about as effective as the tricyclics and they have also been used in anxiety states. Their advantage lies in the lack of many of the adverse effects of the older tricyclics:




• they are generally not cardiotoxic and therefore are less dangerous in overdose
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
