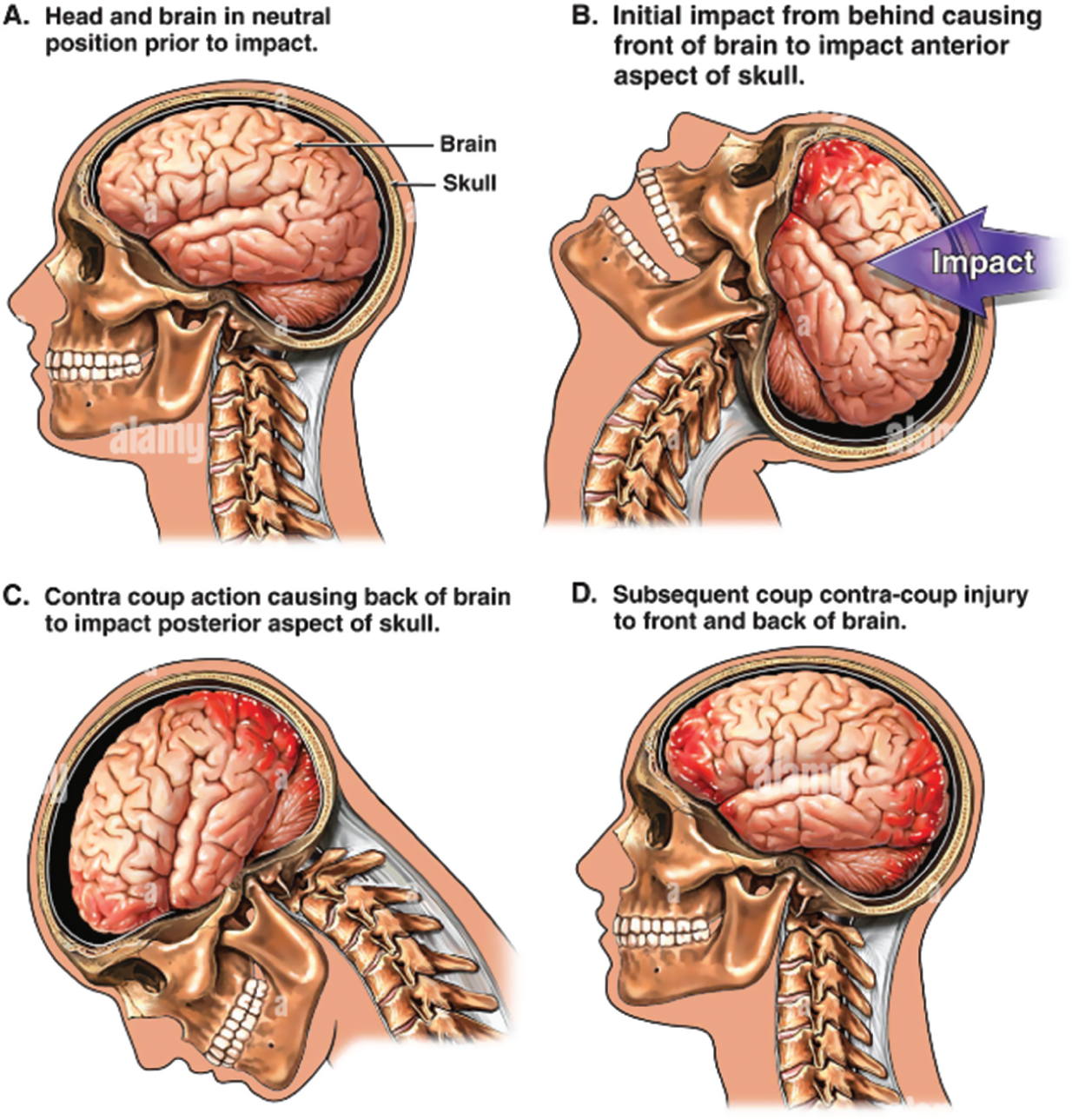
Carol McCormick (acknowledging Katie Dowdie) A closed head injury (CHI) is defined as non-penetrating injury to the brain and occurs when the head accelerates and then rapidly collides with another object (Steffen’ Albert 2010). Trauma causes injury to the brain as a result of a blow to the head, or sudden, violent motion that causes the brain to impact against the skull. No object penetrates through the skull to the brain tissue itself. Brain injury is classified into phases: primary injury and secondary injury. The primary injury is the initial brain insult as a result of traumatic impact. According to Moppett (2007), oedema, capillary leakage, and systemic inflammatory response is associated with secondary injury. Furthermore, secondary injury is worsened by hypoxia and hypotension (Pigula et al. 1993). Coup is injury on site of impact and contre-coup is injury on opposite side of impact. This is shown in Figure 17.1. FIGURE 17.1 Coup and contre-coup injury (collection of L. Henry). Reproduced from Best Practice (https://bestpractice.bmj.com/search?q=Coup+and+contre-coup+injury+ – practice/monograph/967/resources/images.html) with kind permission. Please refer to Table 17.1. Table 17.1 Mead model. Please see Chapter 1 for further reading. Adapted from: McClune and Franklin (1987). Respiratory and cardiovascular needs should be looked at (McClune & Franklin 1987). Any child presenting with a Glasgow Coma Scale (GCS) <8 is classified as a severe head injury (Moppett 2007; Weinstein 2006). The most important initial interventions are: Physical needs Respiratory Assess: continue to assess Leah’s level of consciousness and ability to maintain her: Airway, Breathing, and Circulation (ABC). Cardiovascular Assess: this assessment has some overlap with the respiratory assessment: It is important to know the cardiovascular stability of the child prior to intubation as the choice of drugs used for induction and intubation can have adverse effects. These assessments are carried out very quickly and the child is then prepared for intubation and ventilation. Plan: preparation for child Table 17.2 Emergency/airway trolley for intubation. Table 17.3 Common drugs used for intubation (see BNFc 2023). Implement: NB The combination of drugs used will be decided by the anaesthetist, based on the clinical condition of the child.
CHAPTER 17
Closed Head Injury
ANSWERS TO QUESTIONS
Question 1. What is a closed head injury?
A Respiratory
B Cardiovascular
C Pain/sedation
D Neurology
E Nutrition/hydration
F Elimination
G (i) Skin/wound care
G (ii) Mobility
G (iii) Hygiene
H (i) Psychological and social/culture
H (ii) Circumstantial
Question 2. When using the Mead model, how would the children’s nurse safely maintain the airway of a child with a Glasgow Coma Scale below 8?
At the bedside:
Intravenous anaesthetic used for induction of anaesthesia.
Side effects: apnoea, hypotension, arrhythmias, laryngeal spasm. In excessive doses, hypothermia and reduction in cerebral function.
Ketamine
Induction and maintenance of anaesthesia for short procedures.
Neuromuscular blocking drug, also known as muscle relaxant.
Side effects – skin flushing, hypotension, tachycardia.
Depolarising neuromuscular blocking drug. Used if fast action and brief duration of action is required.
Intravenous anaesthetic used for induction of anaesthesia.
Side effects: hypotension, tachycardia, less common – thrombosis, pulmonary oedema, hyperkalaemia, cardiac failure.
Antimuscarinic drug used in the treatment of bradycardia.
Side effects: tachycardia, dilatation of the pupils, dry mouth, nausea, and vomiting, confusion.
Direct acting sympathomimetic agent. Used in CPR, acute anaphylaxis, low cardiac output. Side effects: nausea, vomiting, tachycardia, arrhythmias, hypertension, cold peripheries.
Opioid analgesia used to relieve moderate to severe pain.
Side effects: nausea, vomiting, constipation, hypotension, respiratory depression.
Benzodiazepine used for sedation.
Side effects: gastro-intestinal disturbances, hypotension, heart rate changes, laryngospasm, respiratory depression.
Used for drug/line flush.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


