CHAPTER 18 Chronic obstructive pulmonary disease
When you have completed this chapter you will be able to:
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is one of the most common diseases in the world, yet public awareness of the disease is much lower than for other lung diseases such as asthma or emphysema. In fact, COPD is not one single disease but an umbrella term for chronic bronchitis and emphysema, and in practice it may be difficult to differentiate between asthma, which is reversible airway obstruction, and COPD, which is irreversible airway obstruction. People with COPD experience breathlessness, coughing, wheeze, increased sputum production, sleep disturbance, fatigue and weight loss. Everyday tasks such as vacuuming, putting on shoes or even walking can become difficult due to breathlessness and the debilitating effects of the disease.
WHAT IS COPD?
The World Health Organization provided the following definition of COPD:
The most common symptoms of COPD are breathlessness, or a ‘need for air’, excessive sputum production, and a chronic cough. However, COPD is not just simply a ‘smoker’s cough’, but an under-diagnosed, life threatening lung disease that may progressively lead to death. World Health Organization, 2007 (http://www.who.int/respiratory/copd/en/)
HOW COMMON IS COPD?
All reports indicate that COPD is one of the main health issues that we should be concerned about in Australia, New Zealand and worldwide. It is estimated to be the fourth leading cause of death worldwide and is likely to rise globally to the third leading cause by 2020 (Sampsonas et al, 2006).
In a report published in 2003 (Town et al, 2003), COPD was identified as a significant New Zealand health issue affecting over 200,000 New Zealanders. Although there is an absence of reliable data on prevalence the report estimated that over $192 million was spent on COPD-related health costs and COPD affected approximately 15% of persons over the age of 45. The report highlighted the need for early detection, which is paramount, as in later stages the effects are irreversible.
According to the Australian Lung Foundation, there were estimated to be 474,000 cases of moderate-to-severe COPD in 2000 in Australia (Australian Lung Foundation, 2001). Prevalence is increasing because of the ageing of the population, and public awareness is low.
About 3.5% of Australians reported having bronchitis or emphysema in the 2001 National Health Survey, compared to 4.1% in 1995 and 3.0% in 1989. Although these estimates would contain some cases of bronchitis that were not chronic in nature, it is still likely to have underestimated the true prevalence of COPD in Australia. This is because COPD is usually not diagnosed until it begins to restrict a person’s lifestyle and is moderately advanced.
COPD is also overwhelmingly more common than asthma as a cause of death. According to a recent AIHW report, there were ten times as many deaths where COPD was mentioned on the death certificate as asthma, and six times as many hospitalisations where COPD was a diagnosis (AIHW, 2006b). According to the same report, COPD is frequently listed as a cause of death associated with other conditions, or as an additional diagnosis among people over 55 years of age.
HOW IS COPD RELATED TO ASTHMA AND OTHER LUNG FUNCTION DISEASES?
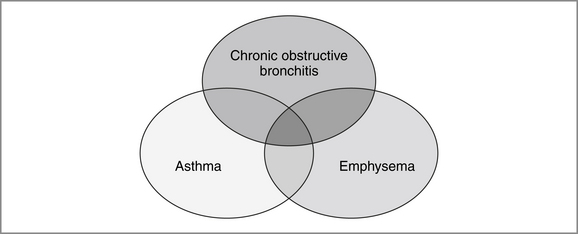
Lung function diseases are all characterised by limitations to airflow, which is measured via spirometry, a respiratory function test (RFT, also known as a lung function test). The separation of asthma and COPD aligns with the current treatment of the two lung conditions as separate although overlapping diseases. Currently accepted definitions emphasise the reversibility of asthma, which is highly responsive to treatment, while COPD is considered to be at the opposite end of the spectrum of airway disease, being poorly reversible and characterised by progressive airway narrowing (Jenkins et al, 2005). Emphysema is a pathological diagnosis, and consists of alveolar dilatation and destruction. Chronic bronchitis is defined as a daily cough with sputum production for at least three months of two or more consecutive years (McKenzie et al, 2003). (Normal lungs produce about 30 millilitres of sputum daily, so sputum production on its own is not abnormal.) In practice, there may be considerable overlap between types of lung disease (see Figure 18.1).
People with COPD commonly refer to their condition by lay terms such as ‘asthma’ or ‘emphysema’, however they usually have a combination of all three types of pathology in varying degrees.
EFFECTS ON PHYSICAL HEALTH
Significant airflow obstruction may be present before the individual is aware of any symptoms. As such, it is no surprise that people are often diagnosed with COPD quite late in the disease trajectory. COPD has a ‘relapse remitting’ course, which Lynn (2001) described as one of illness over many months or years with occasional dramatic exacerbations; each episode may cause death but the individual usually survives many such episodes before death. In the medium to latter stages of COPD, increasingly frequent hospital admissions are not uncommon, reflecting deteriorating lung function and increasing susceptibility to infection. Exacerbations tend to be more common in people with moderate to severe COPD and of greater consequence in those with advanced disease (Sherwood Burge, 2006).
PATHOPHYSIOLOGY OF BREATHLESSNESS
COPD severity is classified by the degree of obstruction during expiration on RFTs. However, evidence suggests that there is little correlation between the degree of obstruction on RFTs and the physical impairment or degree of dyspnoea endured by the individual (Wolkove et al, 1989). Dyspnoea may vary from very mild breathlessness on exertion to rendering an individual housebound. A complex relationship of neural and biochemical factors controls our respiratory rate, which is further modulated by emotional facets such as tolerance of the individual to the sensation of dyspnoea, anxiety, previous experience and expectations. Intrapulmonary pathology (e.g. airway obstruction, impaired gas exchange, hyperinflation) together with extrapulmonary factors (e.g. deconditioning and muscle wasting) govern the biochemical factors that influence the central nervous system’s control of respiration.
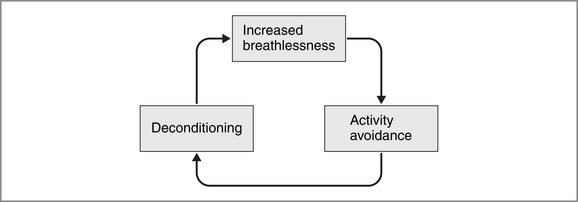
A fear of being dyspnoeic discourages people with COPD from participating in activities that result in breathlessness, which in turn causes further deconditioning and activity avoidance. This vicious cycle of deconditioning (see Figure 18.2) is a common phenomenon and may be further precipitated by musculoskeletal problems (e.g. arthritis), inconvenience (e.g. driving is quicker than walking) or lack of enjoyment of exercise (e.g. colder climates). The principal intervention for people with COPD who are deconditioned is a course of pulmonary rehabilitation, which is discussed later in this chapter.
ALTERED MOBILITY AND FATIGUE
Secondary impairment may result when a physical inability to walk, drive or catch public transport to shops leads to nutritional inadequacies. Weight loss associated with muscle wasting is common in the latter stages of COPD and further impedes exercise tolerance and respiratory function. Low body mass index (BMI) is a well-documented risk factor for poor prognosis in COPD (Schols et al, 1998) and, while the mechanisms for involuntary weight loss are not well understood (Ferreira et al, 2001), impaired swallowing function in advanced COPD is one likely contributor. Increasing dyspnoea makes the 3- to 5-second breath hold required for swallowing difficult, and may increase the risk of aspiration and chest infection. Inhaled respiratory medications often result in a dry mouth, which further hampers safe swallowing function. These factors may lead to avoidance of particular foods or of eating altogether, resulting in nutritional deprivation.
MEASUREMENT OF PHYSICAL HEALTH
Many best practice interventions for COPD, while improving dyspnoea and quality of life, do not alter physiological lung function. Hence assessment of the impact of interventions should focus on the initial goals of the intervention. That is, the use of tools that measure change in other outcomes such as BMI, dyspnoea, functional capacity, the number of exacerbations and quality of life may be more appropriate than repeating RFTs. The goal of many COPD interventions is to decrease dyspnoea; however, dyspnoea is subjective and difficult to quantify. Scales such as the Borg Scale of Dyspnoea (Mahler et al, 1987) and the Medical Research Council Scale of Dyspnoea (Bestall et al, 1999) have been validated for use in this population. The measurement of functional capacity is often achieved using the 6 Minute Walk Test (American Thoracic Society, 2002) or the Incremental Shuttle Walk Test (Singh et al, 1992). These tests may also be used to assess for exertional desaturation or oxygen requirements, and are used by physiotherapists to prescribe exercise. It is worth remembering that physiological measurements of COPD (e.g. spirometry, 6 Minute Walk Test) do not necessarily correlate with the various symptoms of COPD. As such, quality-of-life tools and measures of dyspnoea may more accurately reflect a patient’s perception of their disease severity or impairment, the impact of treatments and the fluctuations in symptoms (Yusen, 2001).
EFFECTS ON MENTAL HEALTH AND QUALITY OF LIFE
The effect of COPD on an individual’s mental health cannot be separated from the physical health, as they are not mutually exclusive. For example, physical deconditioning may lead to social isolation as friends and hobbies become inaccessible, resulting in loneliness and its associated symptom of depression (Kara & Mirici, 2004). Similarly, the anxiety that a person feels in anticipation of dyspnoea may prevent them being adequately motivated to attempt activity, resulting in further deconditioning and progressive dyspnoea.
ADJUSTMENT TO ILLNESS
Symptoms of COPD often present years after smoking has ceased, or without any known risk factor. For many people, recurrent chest infections or insidious dyspnoea leads to a diagnosis some time after initial symptoms arise. Once diagnosed, accepting a disease for which there is no cure, and for which the goals of treatment are to prevent further decline and optimise function, is understandably difficult. Physical limitations from dyspnoea often result in early retirement and a change of role in employment, social and family contexts. An individual’s loss of independence and restrictions on recreational activities may result in irritability, a sense of hopelessness (Yusen, 2001), decreased confidence and lowered self-esteem. Frustration and powerlessness are also common in response to recurrent infections and the impossibility of predicting the timing or severity of exacerbations. There is evidence to demonstrate that acute exacerbations of COPD have a negative impact on health-related quality of life and exercise capacity (Carr et al, 2007) for the duration of the exacerbation and potentially for some time after if the recovery is prolonged. People with COPD must also endure significant lifestyle changes, with the acquisition of new habits (e.g. medications, exercise, modified activities) and the suppression of old habits (e.g. smoking, poor self-care). Perhaps the most difficult adjustment people with COPD must face is the fear of breathlessness, the possibility of not ‘catching their breath’ and the fear of dying.
IMPACT ON THE PERSON AND THEIR FAMILY
Inevitably these symptoms and their impact on ADLs and life role require support and understanding from family and caregivers. It is worth remembering that COPD has a degree of stigma as a ‘self-inflicted’ illness (Sherwood Burge, 2006), which health workers should avoid reinforcing.
DEPRESSION AND ANXIETY
Significant depressive symptoms have been reported in 16–74% of people with COPD (Ng et al, 2007). This may be ‘reactive’ to their situation and considered a consequence of their physical disease, or be of more established biological cause (Gore et al, 2000). Depression in COPD has been shown to have a negative impact on health outcomes including mortality, continued smoking, length of hospital stay and physical and social functioning, even when confounders such as chronicity of COPD and socioeconomic variables are controlled for (Ng et al, 2007). This highlights the importance of monitoring patients with COPD for signs of depression and referring for assessment and treatment in a timely fashion.
Anxiety is particularly common in COPD as a result of dyspnoea (Gore et al, 2000) and may be exacerbated by the vicious cycle of deconditioning (see Figure 18.2). A fear of becoming breathless leads to activity avoidance or fear of exercise, and results in further deconditioning. Anticipatory anxiety then results when the individual next attempts an activity that they perceive may result in breathlessness. Evidence suggests that this dyspnoea anxiety is more heightened in patients with COPD, as Gore, Brophy and Greenstone (2000) found that 90% of patients with COPD suffered clinically relevant anxiety or depression compared with 52% of patients with lung cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree