CHAPTER 21 Chronic kidney disease
INTRODUCTION
Chronic kidney disease (CKD) is a serious health problem and, in its later stages, requires people to invest considerable time to manage their health, including modifying their diet, managing numerous medications, undergoing kidney replacement therapy (KRT) (if required) and attending medical and hospital appointments. CKD, its treatment and concomitant complications have a significant impact on a person’s lifestyle, family responsibilities, ability to work and financial status (Tallis, 2005).
CASE STUDY 21.1 Part 1
His record showed the following:
| 2005 | 2007 | |
| Weight | 90 kg | 96 kg |
| Height | 170 cm | 170 cm |
| BMI | 31.1 kg/m2 | 33.2 kg/m2 |
| Blood pressure | 140/90 | 160/100 |
| Urinalysis | No abnormalities | Protein ++ |
| Urine albumin/creatinine ratio (RR < 1.0) | 150 mg/g | 194 mg/g |
| 24-hour urine collection (RR < 100 mg) | Not done | 2 g protein |
| HbA1c (target < 7%) | 8.7% | 11% |
| Smoking status | Not current smoker | 1 pack per day |
| Haemoglobin (RR 135–180) | 136 g/L | 101 g/L |
| Serum creatinine (RR 70-120) | 145 umol/L | 285 umol/L |
| eGFR (RR > 60) | 47 mL/min | 21.5 mL/min |
Arthur has stage 4 CKD and is at high risk of progressing to stage 5 CKD.
UNDERSTANDING CHRONIC KIDNEY DISEASE
The kidneys have remarkable functional reserve. Up to 80% of the glomerular filtration rate (reflected in creatinine clearance measurements) may be lost with few obvious changes in the functioning of the body. A person is born with about 2 million nephrons and can survive without dialysis until almost 90% of the nephrons are lost. In the majority of cases the individual passes through the early stages of CKD without recognising the disease state because the remaining nephrons hypertrophy to compensate. CKD is defined as either kidney damage or a glomerular filtration rate (GFR) ≤ 60 mL/min/1.73m2 for more than three months. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies (Vassalotti et al, 2007).
In Australia and New Zealand, the number of people with or at risk of CKD is not clear but Kidney Health Australia estimates that one in seven people over the age of 25 years have at least one clinical sign of CKD. The major causes of ESKD, however, are well known, and these are diabetes mellitus (32% Australia, 41% NZ), glomerulonephritis (24% Australia, 22% NZ) and hypertension (14% Australia, 11% NZ) (McDonald et al, 2006). Other significant causes include polycystic kidney disease, analgesic nephropathy and reflux nephropathy. Over the last 25 years, while Australia’s population has grown by 40%, the number of people with CKD and ESKD has increased by 400% (Cass et al, 2006). Aboriginal and Torres Strait Islander peoples in Australia (Australian Institute of Health and Welfare (AIHW), 2005) and New Zealand Māoris are disproportionately affected by ESKD—up to 30 times the national average (Cass et al, 2006). There is some evidence that the high incidence of hypertension and CKD in indigenous people is related to low birth weight (Hoy 2005). CKD also affects children and adolescents, with approximately 4 new cases per million population per year (Darbyshire et al, 2006).
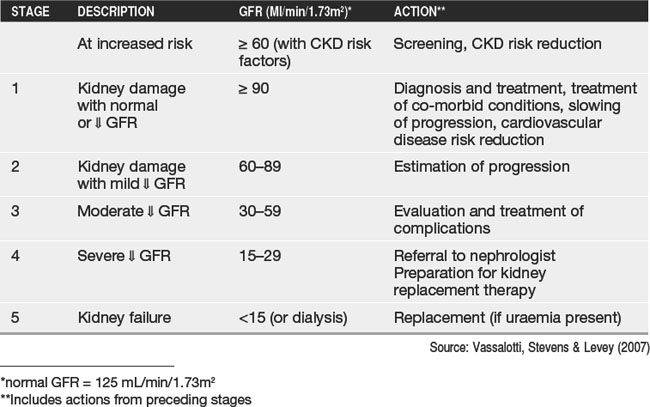
CKD is characterised by a progressive loss of kidney function over time, and the development and progression of cardiovascular disease (Levey et al, 2005; AIHW, 2007). It results from a number of conditions that cause permanent loss of nephron function, and a decrease in GFR. A five-stage classification system for describing the severity of CKD has been developed. This uses GFR to describe the phases of CKD and guides clinical interventions (Table 21.1).
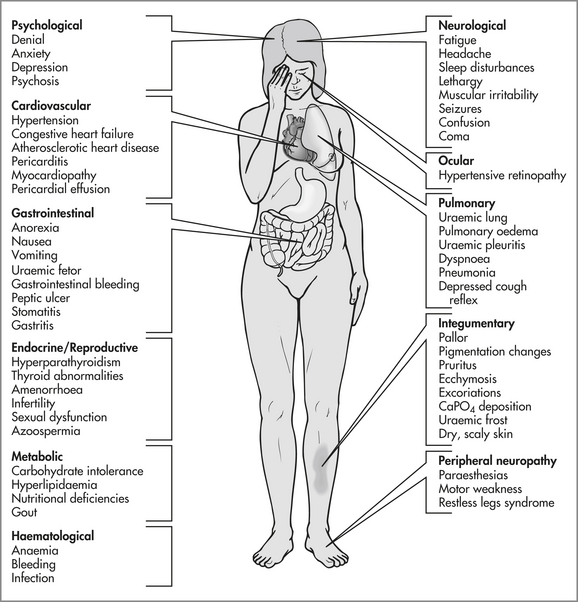
In the early stages of CKD, polyuria results from the decreased ability of the kidneys to concentrate urine. This is most noticeable at night, and the patient must arise several times to urinate (nocturia). During stage 3, when about 50% of nephron function has been destroyed, hypertension, elevated urea and creatinine levels, and anaemia develop (Kilstoff & Bonner, 2006). These effects are summarised in Figure 21.1. Haemodialysis, peritoneal dialysis or kidney transplantation, collectively known as kidney replacement therapy (KRT), are required when the clinical manifestations become life-threatening (usually in stage 5).
SCREENING FOR CKD
An annual kidney health check is recommended for those at risk of CKD (see Table 21.2). In its simplest form a kidney health check will have three components:
Table 21.2 CKD risk factors and screening recommendations.
| WHO IS AT RISK OF CKD? | WHAT SHOULD BE DONE? | HOW OFTEN? |
|---|---|---|
| Increased risk | Every 12 months | |
| High risk Over 50 yrs + one of the following: | Every 12 months | |
| Very high risk | Every 12 months |
Source: Royal Australian College of General Practitioners (2005)
Further screening is required if the patient also has diabetes (or is suspected to have diabetes). Microalbuminuria is a precursor to diabetic kidney disease (Thomas, 2004) and if two of the three screening tests are abnormal, the serum creatinine needs to be measured. The standard multiple urinalysis dipstick is not specific for albumin and will only show positive protein when there is a large amount of albuminuria. In people with diabetes a test for microalbuminuria should always be performed if the urine dipstick for protein is negative.
DELAYING PROGRESSION
The single most important intervention to delay progression of CKD is to achieve good blood pressure control. The target BP is <125/75 for people with proteinuria >1g/24h, <130/80 if proteinuria is 0.25–1g/24h and <130/85 if proteinuria is <0.25g/24h (Gillan, 2005).
Although medication may be introduced early, therapeutic lifestyle change is an important element of delaying progression and preventing complications (Johnson, 2004). Lifestyle changes include cessation of smoking, increased exercise, weight loss and reduced dietary sodium intake. The nurse should encourage the patient to set realistic goals, plan strategies and give positive reinforcement for achievements.
Patients with CKD and albuminuria or proteinuria (see Case study 21.1) may be prescribed an angiotensin-converting enzyme inhibitor (ACEI) or an angiotensin receptor blocker (ARB) even if their blood pressure is normal. These classes of drugs have been shown to protect the kidneys by reducing albumin loss as well as through the blood pressure lowering effect (Lewis et al, 2001).
PREVENTING COMPLICATIONS
People with CKD are susceptible to deterioration in remaining kidney function due to dehydration and nephrotoxic substances. It is important for nurses to be aware that the kidneys are less able to regulate urinary concentration and are more sensitive to dehydration. Intravenous fluids may be needed for diagnostic and/or therapeutic interventions that require fasting. In addition, radio-opaque contrast used in coronary angiography (and similar procedures) is nephrotoxic, and decisions to use contrast will be weighed up in view of the risks and benefits to the individual patient. Many medications (e.g. gentamicin, vancomycin) will require dose adjustment and monitoring to ensure patient safety. Others such as metformin must be used with caution in earlier stages of CKD and discontinued in patients with a creatinine clearance of less than 30 mL/min (Faull & Lee, 2007).
TREATING COMPLICATIONS
As CKD progresses, the complications of CKD manifest, usually around late stage 3 and stage 4. These complications are as a result of anaemia, and abnormal bone and mineral metabolism. Management involves medication (iron supplements, and erythropoietin-stimulating agents for anaemia; calcitriol and phosphate binders for bone and mineral metabolism) (McCarley & Salai, 2005). Some patients will need sodium bicarbonate to correct acidosis or Resonium A for hyperkalaemia.
THE PATIENT WITH END-STAGE KIDNEY DISEASE
When renal function deteriorates to the point of ESKD (stage 5), KRT is required. These treatments include haemodialysis, peritoneal dialysis and renal transplantation. Briefly, haemodialysis (HD) involves access to the vascular system (usually an arteriovenous fistula is formed and cannulated), an extracorporeal circuit, dialyser and technological equipment. Typically, a patient will receive a minimum of four hours of treatment on three occasions each week either in a hospital, satellite dialysis centre or at home (Cass et al, 2006). In Australia nocturnal home haemodialysis is increasing in acceptance: patients do their haemodialysis overnight—sometimes six nights per week.
Peritoneal dialysis (PD) is performed by introducing 2–3 litres of a sterile dextrose-containing solution (dialysate) into the peritoneal cavity. Although there are several different techniques for PD, the most common is continuous ambulatory peritoneal dialysis (CAPD). CAPD requires the individual to manually change the dialysate in the peritoneal cavity four or five times each day, every day of the year.
ALTERED MOBILITY AND FATIGUE
There is considerable literature reporting a wide range of symptoms experienced with CKD that cause people distress and/or disruption to normal daily living (Thomas-Hawkins, 2000). These symptoms include reduced levels of fitness and a reduced capacity to engage in regular activity (Tawney et al, 2003) with a consequent effect on people’s ability to perform routine living chores, their quality of life, their survival, and their need for nursing support (for example assistance with dialysis, arranging community support services).
Levels of activity in CKD are affected by anaemia, lengthy treatment commitments and debilitating co-morbid conditions (Leikis et al, 2006). The promotion of activity is increasingly recognised as integral in rehabilitation with some reports of improved levels of activity in CKD patients’ levels of activity (Tawney et al, 2003), but there has been limited evidence of the adoption of activity-promoting interventions in routine nursing care (White & Grenyer, 2006).
Fatigue is a complex, subjective experience, which is familiar and understood by many, but is difficult to objectively measure (McCann & Boore, 2000). Despite advances in renal healthcare, fatigue remains one the most troublesome symptoms for people with CKD; physical fatigue is frequently experienced, with more than 90% of patients reporting a lack of energy and feeling tired (Thomas-Hawkins, 2000). Factors associated with the fatigue experienced in CKD include prescribed medications and their side-effects; nutritional deficiencies; physiological alterations, such as obstructive sleep apnoea (KHA, 2007); abnormal urea and haemoglobin levels; and psychological factors such as depression, sleep dysfunction and those associated with haemodialysis treatment (Welch, 2006). In one study in Australia, 92 people with CKD or ESKD living in Far North Queensland were found to be more fatigued than the general population (Bonner et al, in press). Of importance for nurses providing healthcare to people with CKD, patients with diabetic nephropathy and those who were pre-dialysis were more fatigued than those receiving KRT.
BODY IMAGE
CKD can result in both physical and psychological changes in body image. There is limited research, however, exploring the patient’s perception of body image in CKD. Physical changes are common and are not restricted to those directly affecting the renal system, as other body systems are also involved (see also Figure 21.1). Alterations in body image are often due to external changes in skin, body weight, mobility, side-effects of medications and the presence of KRT devices. In children, growth retardation occurs due to the effects of uraemia on growth hormone production (Miller et al, 2004). Internal or psychological alterations such as fatigue, depression and altered feelings of wellbeing also occur. Both external and internal alterations in body image may contribute to a decreased quality of life and compliance with treatment.
When CKD progresses to stage 5 and KRT is commenced, other physical alterations to a person’s body image occur due to the presence of dialysis access devices and a number of surgical procedures. These access devices could be either (or in some situations both) a peritoneal dialysis (PD) catheter, an arteriovenous fistula (AVF) or an external vascular catheter. A PD catheter and extension set protrudes from the body by approximately 15–30 cm and often requires adjustments to the type of clothing worn to accommodate its presence (e.g. underpants, location of belts or waist bands). An AVF is an internal surgical anastomosis of an artery and a vein (commonly radial artery and cephalic vein), and results in arterial blood flowing straight into the vein. The AVF causes the vein to dilate, and when repeatedly cannulated for haemodialysis, can result in tortuous and/or aneurysmal dilatations (Brieterman White, 2006) and changes in body image. Vascular catheters can be temporary or permanent, and are often visible. Lastly, scars as a result of previous, and often numerous, surgery for access devices and/or kidney transplantation can also affect an individual’s body image.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree