Chapter 7 Change and Adaptation in Pregnancy
Physiological changes in the reproductive system
The body of the uterus
Decidua
 The decidua is believed to maintain functional quiescence of the uterus during pregnancy; spontaneous labour is thought to result from the activation of the decidua with resultant prostaglandin release following withdrawal of placental hormones.
The decidua is believed to maintain functional quiescence of the uterus during pregnancy; spontaneous labour is thought to result from the activation of the decidua with resultant prostaglandin release following withdrawal of placental hormones.
 The decidua and trophoblast also produce relaxin, which appears to promote myometrial relaxation, and may have a role to play in cervical ripening and rupture of fetal membranes.
The decidua and trophoblast also produce relaxin, which appears to promote myometrial relaxation, and may have a role to play in cervical ripening and rupture of fetal membranes.
Myometrium
Uterine growth is due to hyperplasia (increase in number due to division) and hypertrophy (increase in size) of myometrial cells under the influence of oestrogen (Table 7.1). The dimensions of the uterus vary considerably, however, depending on the age and parity of the woman.
Table 7.1 Uterine growth during pregnancy
| Prior to pregnancy | At term | |
|---|---|---|
| Weight of uterus | 60–80 g | 1000 g |
| Size of uterus | 7.5 × 5 × 2.5 cm | 30 × 22.5 × 20 cm |
The three layers of the myometrium become more clearly defined during pregnancy.
Muscle layers
 The outer longitudinal layer of muscle fibres is thin. It consists of a network of bundles of smooth muscles. These pass longitudinally from the front of the isthmus anteriorly over the fundus and into the vault of the vagina posteriorly, and extend into the round and transverse ligaments.
The outer longitudinal layer of muscle fibres is thin. It consists of a network of bundles of smooth muscles. These pass longitudinally from the front of the isthmus anteriorly over the fundus and into the vault of the vagina posteriorly, and extend into the round and transverse ligaments.
 The thicker middle layer comprises interlocked spiral myometrial fibres that are perforated in all directions by blood vessels. Each cell in this layer has a double curve so that the interlacing of any two gives the approximate form of a figure of eight. Due to this arrangement, contraction of these cells after birth causes constriction of the blood vessels, providing ‘living ligatures’.
The thicker middle layer comprises interlocked spiral myometrial fibres that are perforated in all directions by blood vessels. Each cell in this layer has a double curve so that the interlacing of any two gives the approximate form of a figure of eight. Due to this arrangement, contraction of these cells after birth causes constriction of the blood vessels, providing ‘living ligatures’.
 The inner circular layer is arranged concentrically around the longitudinal axis of the uterus and bundle formation is diffuse. It forms sphincters around the openings of the uterine tubes and around the internal cervical os.
The inner circular layer is arranged concentrically around the longitudinal axis of the uterus and bundle formation is diffuse. It forms sphincters around the openings of the uterine tubes and around the internal cervical os.
Uterine activity in pregnancy
 The contractile ability of the myometrium is dependent on the interaction between two contractile proteins, actin and myosin.
The contractile ability of the myometrium is dependent on the interaction between two contractile proteins, actin and myosin.
 The interaction of actin and myosin brings about contraction, whereas their separation brings about relaxation under the influence of intracellular free calcium.
The interaction of actin and myosin brings about contraction, whereas their separation brings about relaxation under the influence of intracellular free calcium.
 The coordination of synchronous contractions across the whole organ is due to the presence of gap junctions that connect myometrial cells and provide connections for electrical activity. Gap junctions are absent for most of the pregnancy but appear in significant numbers near term, manifesting themselves as Braxton Hicks contractions.
The coordination of synchronous contractions across the whole organ is due to the presence of gap junctions that connect myometrial cells and provide connections for electrical activity. Gap junctions are absent for most of the pregnancy but appear in significant numbers near term, manifesting themselves as Braxton Hicks contractions.
 The formation of gap junctions is promoted by oestrogens and prostaglandins.
The formation of gap junctions is promoted by oestrogens and prostaglandins.
 Progesterone, prostacyclin and relaxin, however, are all involved in inhibiting the formation of gap junctions by reducing cell excitability and cell connections and so limiting myometrial activity to small clumps of cells, thus maintaining uterine quiescence during pregnancy.
Progesterone, prostacyclin and relaxin, however, are all involved in inhibiting the formation of gap junctions by reducing cell excitability and cell connections and so limiting myometrial activity to small clumps of cells, thus maintaining uterine quiescence during pregnancy.
In the last few weeks of pregnancy, prelabour occurs:
 Further increases in myometrial contractions cause the muscle fibres of the fundus to be drawn up.
Further increases in myometrial contractions cause the muscle fibres of the fundus to be drawn up.
 The actively contracting upper uterine segment becomes thicker and shorter in length and exerts a slow, steady pull on the relatively fixed cervix.
The actively contracting upper uterine segment becomes thicker and shorter in length and exerts a slow, steady pull on the relatively fixed cervix.
 This causes the beginning of cervical stretching and ripening known as effacement, and thinning and stretching of the passive lower uterine segment.
This causes the beginning of cervical stretching and ripening known as effacement, and thinning and stretching of the passive lower uterine segment.
Perimetrium
 The double folds of perimetrium (broad ligaments), hanging from the uterine tubes and extending to the lateral walls of the pelvis, become longer and wider with increasing tension exerted on them as the uterus enlarges and rises out of the pelvis.
The double folds of perimetrium (broad ligaments), hanging from the uterine tubes and extending to the lateral walls of the pelvis, become longer and wider with increasing tension exerted on them as the uterus enlarges and rises out of the pelvis.
 The anterior and posterior folds open out so that they are no longer in apposition and can therefore accommodate the greatly enlarged uterine and ovarian arteries and veins.
The anterior and posterior folds open out so that they are no longer in apposition and can therefore accommodate the greatly enlarged uterine and ovarian arteries and veins.
 The round ligaments (contained within the hanging folds of perimetrium) provide some anterior support for the enlarging uterus and undergo considerable hypertrophy and stretching during pregnancy, which may cause discomfort.
The round ligaments (contained within the hanging folds of perimetrium) provide some anterior support for the enlarging uterus and undergo considerable hypertrophy and stretching during pregnancy, which may cause discomfort.
Changes in uterine shape and size
For the first few weeks the uterus maintains its original pear shape, but as pregnancy advances the corpus and fundus assume a more globular form (Box 7.1).
Box 7.1 Changes in the pregnant uterus
12 weeks
• The uterus is about the size of a grapefruit
• It is no longer anteverted and anteflexed and has risen out of the pelvis and become upright
• The fundus may be palpated abdominally above the symphysis pubis
• The globular upper segment is sitting on an elongated stalk formed from the isthmus, which softens and which will treble in length from 7 to 25 mm between the 12th and 36th weeks
38 weeks
• The uterus reaches the level of the xiphisternum
• As the upper segment muscle contractions increase in frequency and strength, the lower uterine segment develops more rapidly and is stretched radially; along with cervical effacement and softening of the tissues of the pelvic floor, this permits the fetal presentation to begin its descent into the upper pelvis
• This leads to a reduction in fundal height known as lightening, relieving pressure on the upper part of the abdomen but increasing pressure in the pelvis. In the majority of multiparous women, however, engagement rarely occurs prior to labour
The cervix
 The connective tissue of the long firm cervix is progressively softened by prostaglandins and shortened from the top downwards.
The connective tissue of the long firm cervix is progressively softened by prostaglandins and shortened from the top downwards.
 The softened muscular fibres at the level of the internal cervical os are pulled upwards or ‘taken up’ into the lower uterine segment and around the fetal presenting part and the forewaters.
The softened muscular fibres at the level of the internal cervical os are pulled upwards or ‘taken up’ into the lower uterine segment and around the fetal presenting part and the forewaters.
 The canal that was about 2.5 cm long becomes a mere circular orifice with paper-thin edges.
The canal that was about 2.5 cm long becomes a mere circular orifice with paper-thin edges.
Changes in the cardiovascular system
The heart
 The heart enlarges by about 12% between early and late pregnancy.
The heart enlarges by about 12% between early and late pregnancy.
 The growing uterus elevates the diaphragm, the great vessels are unfolded and the heart is correspondingly displaced upwards, with the apex moved laterally to the left by about 15°.
The growing uterus elevates the diaphragm, the great vessels are unfolded and the heart is correspondingly displaced upwards, with the apex moved laterally to the left by about 15°.
 By mid-pregnancy more than 90% of women develop an ejection systolic murmur, which lasts until the first week postpartum. If unaccompanied by any other abnormalities, it reflects the increased stroke output.
By mid-pregnancy more than 90% of women develop an ejection systolic murmur, which lasts until the first week postpartum. If unaccompanied by any other abnormalities, it reflects the increased stroke output.
 Twenty per cent develop a transient diastolic murmur and 10% develop continuous murmurs, heard over the base of the heart, owing to increased mammary blood flow.
Twenty per cent develop a transient diastolic murmur and 10% develop continuous murmurs, heard over the base of the heart, owing to increased mammary blood flow.
 Rotational and axis changes during pregnancy cause an inverted T wave to be apparent on the electrocardiogram (ECG) – essential to note if resuscitation is required.
Rotational and axis changes during pregnancy cause an inverted T wave to be apparent on the electrocardiogram (ECG) – essential to note if resuscitation is required.
Cardiac output
 The increase in cardiac output ranges from 35 to 50% in pregnancy, from an average of 5 L/min before pregnancy to approximately 7 L/min by the 20th week; thereafter the changes are less dramatic.
The increase in cardiac output ranges from 35 to 50% in pregnancy, from an average of 5 L/min before pregnancy to approximately 7 L/min by the 20th week; thereafter the changes are less dramatic.
 The increased cardiac output is due to rises in both stroke volume and heart rate.
The increased cardiac output is due to rises in both stroke volume and heart rate.
 The increase in heart rate begins in the 7th week and by the third trimester it has increased by 10–20%.
The increase in heart rate begins in the 7th week and by the third trimester it has increased by 10–20%.
 Heart rates are typically 10–15 beats per minute faster than those of the non-pregnant woman.
Heart rates are typically 10–15 beats per minute faster than those of the non-pregnant woman.
 The stroke volume increases by 10% during the first half of pregnancy, and reaches a peak at 20 weeks’ gestation that is maintained until term.
The stroke volume increases by 10% during the first half of pregnancy, and reaches a peak at 20 weeks’ gestation that is maintained until term.
Blood
Blood pressure
 Early pregnancy is associated with a marked decrease in diastolic blood pressure but little change in systolic pressure. With reduced peripheral vascular resistance the systolic blood pressure falls an average of 5–10 mmHg below baseline levels and the diastolic pressure falls 10–15 mmHg by 24 weeks’ gestation.
Early pregnancy is associated with a marked decrease in diastolic blood pressure but little change in systolic pressure. With reduced peripheral vascular resistance the systolic blood pressure falls an average of 5–10 mmHg below baseline levels and the diastolic pressure falls 10–15 mmHg by 24 weeks’ gestation.
 Thereafter blood pressure gradually rises, returning to prepregnant levels at term. Posture can have a major effect on blood pressure. The supine position can decrease cardiac output by as much as 25%.
Thereafter blood pressure gradually rises, returning to prepregnant levels at term. Posture can have a major effect on blood pressure. The supine position can decrease cardiac output by as much as 25%.
 Compression of the inferior vena cava by the enlarging uterus during the late second and third trimesters results in reduced venous return, which in turn decreases stroke volume and cardiac output.
Compression of the inferior vena cava by the enlarging uterus during the late second and third trimesters results in reduced venous return, which in turn decreases stroke volume and cardiac output.
Blood volume
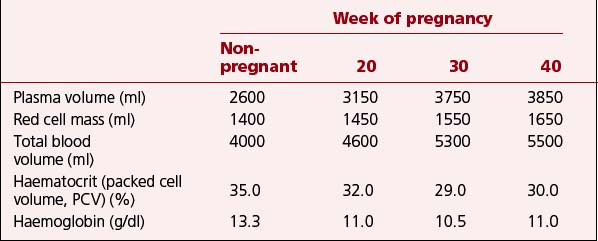
The total maternal blood volume increases 30–50% in singleton pregnancies.
Red cell mass increases during pregnancy in response to the extra oxygen requirements of maternal and placental tissue. Approximately 10–15% of women will have an increase in and reactivation of maternal fetal haemoglobin. The increase in red cell mass appears to be constant throughout pregnancy but it is most marked from about 20 weeks. In spite of the increased production of red blood cells, the marked increase in plasma volume causes dilution of many circulating factors. As a result, the red cell count, haematocrit and haemoglobin concentration all decrease (Table 7.2).
Table 7.2 Falling haemoglobin and haematocrit in pregnancy despite rising blood volume and red cell mass
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



