Central Venous Pressure Monitoring
With central venous pressure (CVP) monitoring, a catheter is inserted through a vein and advanced until its tip lies in or near the right atrium. Because no major valves lie at the junction of the vena cava and right atrium, pressure at end diastole reflects back to the catheter. When connected to a monitoring system, the catheter measures CVP—an index of right ventricular function.
CVP monitoring helps to assess cardiac function, evaluate venous return to the heart, and indirectly gauge how well the heart is pumping. The central venous (CV) catheter also provides access to a large vessel for rapid, high-volume fluid administration and allows frequent blood withdrawal for laboratory samples. CVP monitoring can be done intermittently or continuously. The catheter is inserted percutaneously or using a cutdown method. Typically, a single lumen CVP line is used for intermittent pressure readings with the use of a water manometer or a transducer and stopcock. A pulmonary artery (PA) catheter has a proximal lumen appropriate for continuous CVP monitoring.
Normal CVP ranges from 5 to 10 cm H2O or 2 to 6 mm Hg.1 Changes in preload status are reflected in CVP readings. Any condition that alters venous return, circulating blood volume, or cardiac performance may affect CVP. If circulating volume increases (such as with enhanced venous return to the heart from fluid overload, heart failure, and positive-pressure breathing), CVP rises. If circulating volume decreases (such as with reduced venous return from hypovolemia secondary to dehydration, interstitial fluid shift or hemorrhage, and negative pressure breathing), CVP drops.
Equipment
Leveling device ▪ IV pole ▪ IV solution ▪ gloves and other personal protective equipment, as needed.
For CVP Measurement with a Water Manometer
Disposable CVP manometer set ▪ additional stopcock (to attach the CVP manometer to the catheter) ▪ extension tubing, if needed ▪ IV drip chamber and tubing.
For CVP Measurement with a Transducer
Pressure-monitoring kit with disposable pressure transducer ▪ bedside pressure module ▪ pressure bag.
Implementation
Gather the necessary equipment.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.5
Explain the procedure to the patient to reduce his anxiety.
If one isn’t already in place, assist the doctor as he inserts a CV or PA catheter. (See “Central venous access catheter,” page 133.)
With the CV catheter in place, position the patient between 0 and 45 degrees with the bed in its lowest position.1
Find the right atrium by locating the fourth intercostal space at the midaxillary line. Mark the appropriate place on the patient’s chest so that all subsequent recordings will be made using the same location. When the head of the bed is elevated, the phlebostatic axis remains constant but the midaxillary line changes. Use the same degree of elevation for all subsequent measurements.
Measuring CVP with a Water Manometer
Prime the IV tubing and manometer setup. Attach the water manometer to an IV pole or place it next to the patient’s chest.
Connect the IV tubing to the CV catheter. Trace the tubing from the patient to its point of origin to make sure that it’s attached to the proper port.
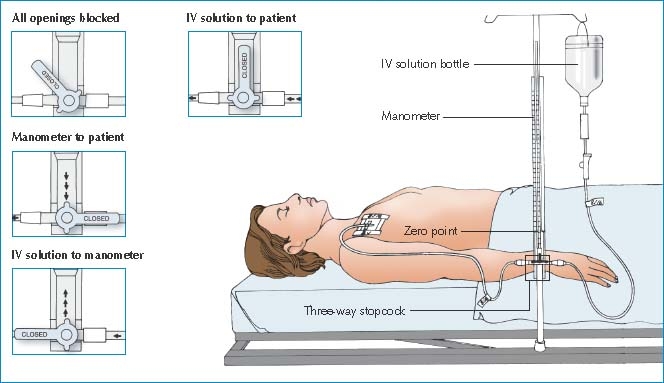
Align the base of the manometer with the zero reference point by using a leveling device and secure the manometer in place. Because CVP reflects right atrial pressure, you must align the right atrium (the zero reference point) with the zero mark on the manometer. (See Measuring CVP with a water manometer.)
Typically, markings on the manometer range from −2 to 38 cm H2O. However, manufacturer’s markings may differ, so be sure to read the directions before setting up the manometer and obtaining readings.
Turn the stopcock off to the patient and slowly fill the manometer with IV solution until the fluid level is 10 to 20 cm H2O higher than the patient’s expected CVP value. Don’t overfill the tube because fluid that spills over the top can become a source of contamination.
Measuring CVP with a Water Manometer
To ensure accurate central venous pressure (CVP) readings, make sure that the manometer base is aligned with the patient’s right atrium (the zero reference point). The manometer set usually contains a leveling rod to allow you to determine this alignment quickly.
After adjusting the manometer’s position, examine the three-way stopcock. By turning it to any position shown below, you can control the direction of fluid flow. Four-way stopcocks are also available.
 |
Intermittent CVP Readings using a Water Manometer
Turn the stopcock off to the IV solution and open to the patient. The fluid level in the manometer will drop. When the fluid level comes to rest, it will fluctuate slightly with respirations. Expect it to drop during inspiration and to rise during expiration.
Record CVP at the end of expiration, when intrathoracic pressure has a negligible effect and the fluctuation is at its highest point.1 Depending on the type of water manometer used, note the value either at the bottom of the meniscus or at the midline of the small floating ball.
After you’ve obtained the CVP value, turn the stopcock to resume the IV infusion. Adjust the IV drip rate, as required.
Place the patient in a comfortable position.
Document the procedure.6
Continuous CVP Readings using a Water Manometer
Make sure the stopcock is turned so that the IV solution port, CVP column port, and patient port are open. Be aware that with this stopcock position, infusion of the IV solution increases CVP. Therefore, expect higher readings than those taken with the stopcock turned off to the IV solution.
If the IV solution infuses at a constant rate, CVP will change as the patient’s condition changes, although the initial reading will be higher. Assess the patient closely for changes.
Record CVP values at appropriate intervals.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
