Chapter 13 Central lines
INTRODUCTION
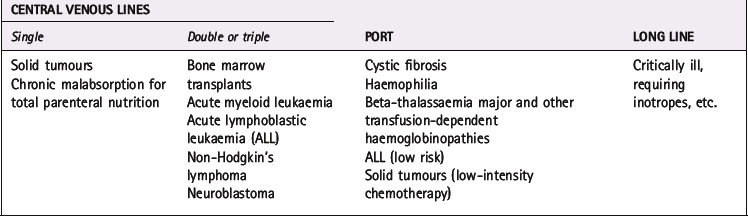
A central line is inserted when a child requires frequent and/or long-term venous access. Reasons for insertion may include the administration of total parenteral nutrition, cytotoxic drugs or frequent intravenous antibiotics. These lines are usually inserted under general anaesthetic in theatre by experienced paediatric surgeons or by experienced anaesthetists. The use of ultrasound imaging is recommended to locate and assist in central venous access device insertion (NICE 2002).
RATIONALE
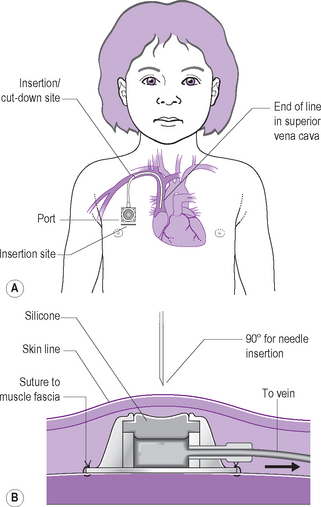
Central venous lines play a crucial role in the administration of treatment to many children with acute and chronic potentially life-threatening illnesses (see Table 13.1 for examples). They reduce the need for frequent venepuncture, which is extremely distressing for all children, particularly the very young.
Nurses have a key role in the care of these lines. In addition to performing the practical procedures, they are responsible for the education of the child, family and those in the community who are unfamiliar with central lines (McInally 2005). A sound policy for line care, adhered to by all involved, will help to ensure that a line can safely remain in use for as long as required.
FACTORS TO NOTE
There are three types of central line used for children.
Tunnelled central venous line
Also known as a Broviac, or Hickman line, or often by the child as a ‘wiggly’. These are skin-tunnelled silastic catheters which are inserted, under general anaesthetic, into the subclavian or internal jugular vein (Fig. 13.1). These lines can be single, double or triple lumen with each lumen having an external clamp. The type inserted depends upon the clinical requirements of the patient.
Note: 10 mL or larger syringes are recommended, particularly when confirming patency.
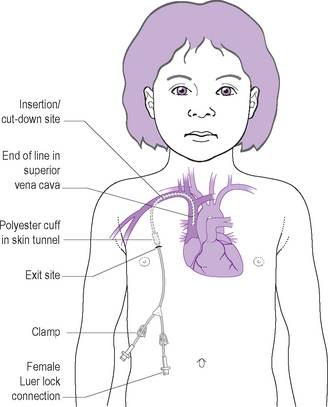
Implanted port
Also known as a Port-a-Cath, Vascuport or TIVAD (totally implantable venous access device). This is a silastic catheter, inserted into the subclavian or internal jugular vein, which is attached to a metal or plastic chamber sealed at the top with a septum of self-sealing silicone. The port (chamber) is positioned under the skin on the chest wall. Access to this system is via straight or angled Huber non-coring needles through the septum of the port (Fig. 13.2).
Note: Always use 10 mL or larger syringes with the ports as recommended by the manufacturers.
Non-tunnelled long line
Note: 10 mL or larger syringes are recommended with PICC lines.
The type of line used for a particular child will depend upon various factors:
This is usually decided by the medical consultants in charge of the individual child’s care and is often also dependent upon the treatment protocol. Full details of the line inserted, i.e. make, model and size, should be documented in the child’s medical notes. This assists staff to obtain the correct repair kit in the event of a line break. Table 13.1 gives examples of conditions and the type of line used for each condition.
Preparation of the child and family for the insertion of any central line is essential (McInally 2005). This includes information from medical and nursing staff, plus preparatory work by the hospital play specialist if available. After discussion with the child and family, it may be useful to introduce them to another child with the same type of line.
Central venous lines can be in situ for months or even years, often in children who are immunocompromised (Cesaro et al 2004, Ewenstein et al 2004, McIntosh 2003, McInally 2005, Valentino et al 2004). As they provide direct access to the child’s central venous system, the major risk is of infection either to the exit site or the line itself with the potential for septicaemia. For this reason alone, strict aseptic non-touch procedures need to be maintained when accessing all types of central line (NICE 2003, Pratt et al 2007).
Many children will go home with these lines in situ so they and their families need to follow the same procedures and be knowledgeable about potential problems and how to deal with them (McInally 2005, Pratt et al 2007). Community nursing staff may also be involved in their care.
GENERAL GUIDELINES
Central venous lines require heparinising weekly when not in use, and daily if being used intermittently for drug administration. Heparinisation has been shown to significantly reduce bacterial colonisation of central venous lines (Pratt et al 2007). It has also been shown to have a strong non-significant trend towards a reduction in line-related bacteraemia. Some lines with very small lumens will require heparinisation more frequently. There is considerable variation in the frequency of heparinising lines, so local hospital policy must be adhered to.