Chapter 19 Cast care
INTRODUCTION
Casts are used to obtain immobilisation, protection and correction of bone, tissue damage, deformity and pain relief. Correct care is essential to prevent complications arising. Stone (2000) acknowledges that casting which includes the application, adaptation and the removal of casts, requires skill, knowledge and judgement to care for patients safely.
RATIONALE
Newman & Fawcett (1995) and Smith (2004), endorse the importance of effective communication and information to allow children and carers to be adequately prepared and understand the necessity for the application of the cast, its subsequent care and the recognition of possible complications. It is therefore necessary that the nurse has the required skills of cast application and knowledge of the principles involved, including possible complications which may arise (BOA 1998, RCN 1999).
FACTORS TO NOTE
Casting materials
Plaster of Paris, fibreglass, flexible polyester based and semi-rigid materials are the most commonly used materials today. Each has its own advantages and disadvantages for use (Miles et al 2000).
Plaster of Paris
This is a high-quality gypsum impregnated onto an open weave fabric material. It has been the most common choice for immobilisation for many years. It is relatively inexpensive, pliable and easy to mould, smoothing to conform almost exactly to the extremity (Cutler 2007).
However, despite starting to set in 5–7 min, it may take up to 48 h for the plaster cast to dry completely (Prior & Miles 1999a, Altizer 2004). During this time, the wet cast should be supported by a pillow and handled with the palms of the hands to prevent denting the cast (Pifer 2000, Altizer 2004). Walking on a cast before it is fully set will cause the same problem.
Fibreglass
It comes in a variety of colours, is radiolucent, lightweight and is stronger than Plaster of Paris (McRae & Esser 2002). However, it requires five to eight layers for weight-bearing casts (Cutler 2007) and, although more resistant to damage, it can be brittle and crack from repetitive use and can leave a sharp edge, potentially causing excoriation of the skin (Cutler 2005).
It takes approximately 30 min to dry completely, making weight-bearing and use of the casted limb possible much sooner (Prior & Miles 1999a). Fibreglass casting materials have water-resistant properties. However, the underlying padding if not waterproof can pose a problem if exposed to water and may result in excoriation of the skin or formation of a pressure sore.
The resilience of the material makes it more difficult to conform well to the extremity and, unlike Plaster of Paris, it does not mould specifically. The extremity must be in the correct position before application; if not, wrinkles may develop which cannot be smoothed out and can result in pressure sores (Miles et al 2000).
The resin becomes tacky when in contact with water and may make the material resist coming off the roll. If pulled too hard on application, it may compromise the circulation. It is essential that healthcare professionals applying casts are familiar with the products they are using and read the manufacturers’ advice and instructions for use (Miles et al 2000, Cutler 2007).
Fibreglass is more expensive than Plaster of Paris, and for this reason is often not the initial cast of choice following trauma or surgery, when removal may be necessary because of swelling or wound inspection. Fibreglass casts can leave sharp edges and, as noted by Prior and Miles (1999a), may cause breakdown of the skin.
Polyurethane-based materials
Polyurethane-based materials that incorporate a flexible polyester were introduced early in the 1990s and are used in some areas. It is radiolucent, lightweight, durable, flexible and conforms to the limb shape very easily and it can be removed with a serrated scissor edge or with the oscillating saw. Fewer layers are required for weight-bearing purposes. This type of casting material lends itself well to focused rigidity casting (FRC). The main concept of FRC is the stabilisation of a fracture with maximum support at the fracture site but less support targeted above and below the fracture site. This allows a degree of functional movement and micro-motion that encourages the stimulation of blood flow and therefore promotes the healing process. FRC is achieved by using four layers of material at the fracture site and two layers elsewhere. The application is very specific and moulding of the material is paramount to its success. A single cast can be used throughout a treatment episode because it can be adjusted to accommodate swelling or muscle atrophy. This method of casting was developed in Germany and evaluated in the UK by Petty and Wardman in 1998. Their study looked at the safety and effectiveness of this new technique, the effect on patients living with a cast, patient satisfaction and cost-effectiveness of the materials, and concluded that FRC application is beneficial to the patient allowing early mobilisation and better function with less impact on daily living and although the initial cost of the material is more expensive, it is more cost-effective because less material is required. Munshi et al (2000) used FRC for treatment of a stable forearm greenstick fracture in children and highlighted similar results.
Semi-rigid materials
At first glance, this material looks like fibreglass. However, the composition is slightly different and combines flexibility with resilience after the final curing stage. A semi-rigid cast is more commonly used in conjunction with a fibreglass membrane (combination casting) to add strength and stability to the finished product. It is versatile, lightweight, radiolucent, flexible, mouldable and leaves a soft edge. The application of this material is again quite specific. It can be removed using a serrated edge scissor or by unwrapping it like a bandage, therefore making it beneficial to children by reducing the trauma of removal especially in the pre-verbal child or a child with learning difficulties. Schuren 1998 provides a full guide to this material, its application and how to use it.
All materials generate heat initially; therefore it is advisable to use cool or tepid water for dipping the tape, otherwise the patient may sustain a plaster burn (Prior & Miles 1999b).
Allergic skin reactions can sometimes be caused by certain paddings and casting materials. Parents and children should be advised on what to look for (Miles et al 2000).
Effects of application on the patient and family
Very often, carers are not prepared for the frustrations, fears and difficulties associated with the child’s cast confinement (Prior & Miles 1999b). Preparation of the family for the reality of home care could help to make what may be a difficult recovery period more acceptable to all concerned. Problems may not be eliminated fully but prior warning enables the carers and child to deal with them in whatever way is convenient to their circumstances (Miles et al 2000). What makes these problems overwhelming is learning about them after discharge when lack of knowledge, equipment and support becomes apparent. Smith (2004) concurred that families with children in hospital require information about their illness, treatment and subsequent care and that families caring for children living with casts on may require the information to be more specifically related and to be supported with information in a written format and upon discharge telephone contact details for help if needed.
A simple explanation of what is normal and what is not can be very helpful, for example the psychological aspects of cast confinement may mean that a once independent child may now be totally dependent, causing insecurity, frustration, tantrums and demanding behaviour, as highlighted by Clarke and Dowling (2003). Educating the family will help to eliminate this.
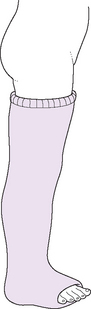
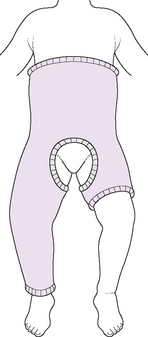
Types of cast
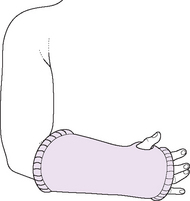
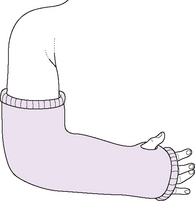
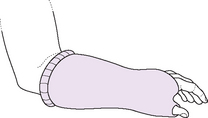
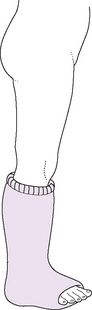
The most common casts used for children are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree