7 Caring for the patient with a disorder of the urinary system
ANATOMY AT A GLANCE
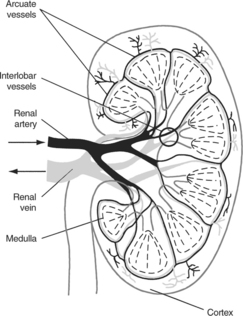
Each kidney consists of a fatty capsule containing the medulla and cortex, which collectively is known as the renal parenchyma (see Figure 7.1). The medulla is divided up into a series of subunits known as the renal pyramids (between 8 and 18 per kidney). The functional units of the kidneys are the nephrons, which are contained within the medulla and cortex, totalling approximately one million per kidney.
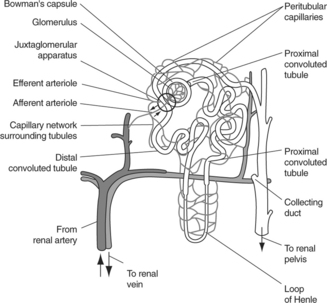
 Blood supply: as can be seen from Figure 7.2, each nephron is supplied with blood via an afferent arteriole, which divides into a tangled web of capillaries called the glomerulus before reuniting to form an efferent arteriole that is narrower than the original afferent arteriole. The efferent arteriole then subdivides into a network of peritubular capillaries, which surrounds the tubule before reuniting to form the peritubular venules which feed into the renal vein.
Blood supply: as can be seen from Figure 7.2, each nephron is supplied with blood via an afferent arteriole, which divides into a tangled web of capillaries called the glomerulus before reuniting to form an efferent arteriole that is narrower than the original afferent arteriole. The efferent arteriole then subdivides into a network of peritubular capillaries, which surrounds the tubule before reuniting to form the peritubular venules which feed into the renal vein. The nephron: the glomerulus is surrounded by a capsule which leads into the tubule itself. The tubule has four portions:
The nephron: the glomerulus is surrounded by a capsule which leads into the tubule itself. The tubule has four portions: The ureters: the urine drains via the collecting ducts eventually into the minor calyces and finally into the calyx of the kidney and on into the ureter at the pelvis of the kidney. The ureter is a 25–30 cm long tube consisting of involuntary muscle which carries the urine to the bladder. Gravity and waves of peristalsis spreading through the muscle wall of the ureter propel urine to the bladder.
The ureters: the urine drains via the collecting ducts eventually into the minor calyces and finally into the calyx of the kidney and on into the ureter at the pelvis of the kidney. The ureter is a 25–30 cm long tube consisting of involuntary muscle which carries the urine to the bladder. Gravity and waves of peristalsis spreading through the muscle wall of the ureter propel urine to the bladder. The bladder: this consists of a muscular sac with a capacity of 700–800 mL which stores urine ready for excretion. The muscle in the bladder wall is arranged in three layers, and is collectively known as the detrusor muscle. The ureters enter through the bladder wall at an oblique angle, relying on the pressure of urine in a filling bladder to compress the ureters and so close them sufficiently to prevent backflow into the kidney (there is no valve system to prevent backflow).
The bladder: this consists of a muscular sac with a capacity of 700–800 mL which stores urine ready for excretion. The muscle in the bladder wall is arranged in three layers, and is collectively known as the detrusor muscle. The ureters enter through the bladder wall at an oblique angle, relying on the pressure of urine in a filling bladder to compress the ureters and so close them sufficiently to prevent backflow into the kidney (there is no valve system to prevent backflow). The urethra: the internal sphincter of the bladder (involuntary muscle) and external sphincter (voluntary muscle) guard the entrance to the urethra. In females the urethra is very short (4 cm), but may be 15–20 cm in males. The urethra empties via the external urinary meatus.
The urethra: the internal sphincter of the bladder (involuntary muscle) and external sphincter (voluntary muscle) guard the entrance to the urethra. In females the urethra is very short (4 cm), but may be 15–20 cm in males. The urethra empties via the external urinary meatus.PHYSIOLOGY YOU NEED TO KNOW
As adults we are 55% (women) to 60% (men) water. Some 66% of that water resides within cells and is known as intracellular fluid; the rest is extracellular fluid divided between plasma and interstitial fluid in a ratio of about 1 : 4. We excrete an average of 1500 mL of urine per day, but also lose some 600 mL of water in evaporation from the skin, 300 mL in breathing out and a further 100 mL in faecal matter. Fluid intake therefore needs to be around 2500 mL per day to achieve fluid balance.
The functions of the renal system may be summarized as follows:
 To regulate fluid and electrolyte balance within the body. This ensures that
To regulate fluid and electrolyte balance within the body. This ensures that Assists in the production of vitamin D (calcitrol) which helps the body extract calcium from food in the gut.
Assists in the production of vitamin D (calcitrol) which helps the body extract calcium from food in the gut. Filtration: occurs in the glomerulus, the narrower diameter efferent arteriole helps generate filtration pressure within the glomerulus as does overall blood pressure. Filtration rate depends largely on the rate of supply of blood to the kidneys via the renal arteries. Average rate is 105–125 mL/min.
Filtration: occurs in the glomerulus, the narrower diameter efferent arteriole helps generate filtration pressure within the glomerulus as does overall blood pressure. Filtration rate depends largely on the rate of supply of blood to the kidneys via the renal arteries. Average rate is 105–125 mL/min. Reabsorption: this occurs as molecules move from the filtrate through the wall of the tubule into the interstitial fluid, and finally into the network of tubular blood vessels. The proximal convoluted tubule sees the reabsorption of large quantities of glucose, sodium, potassium, chloride and water, to name but a few substances. Lesser amounts of water, sodium, potassium and chloride are absorbed in the loop of Henle and further small amounts of water, sodium and chloride in the distal convoluted tubule.
Reabsorption: this occurs as molecules move from the filtrate through the wall of the tubule into the interstitial fluid, and finally into the network of tubular blood vessels. The proximal convoluted tubule sees the reabsorption of large quantities of glucose, sodium, potassium, chloride and water, to name but a few substances. Lesser amounts of water, sodium, potassium and chloride are absorbed in the loop of Henle and further small amounts of water, sodium and chloride in the distal convoluted tubule. Secretion: waste products such as urea, creatinine, ammonium and free hydrogen ions are secreted into the filtrate on its passage through the tubule. The body may fine-tune water and potassium reabsorption in the final part of the distal tubule and collecting duct. The hormone aldosterone acts here to secrete excess potassium into the filtrate for excretion and reabsorb sodium and water in return. Antidiuretic hormone can increase the rate of water reabsorption in this final region of the nephron, concentrating the urine further.
Secretion: waste products such as urea, creatinine, ammonium and free hydrogen ions are secreted into the filtrate on its passage through the tubule. The body may fine-tune water and potassium reabsorption in the final part of the distal tubule and collecting duct. The hormone aldosterone acts here to secrete excess potassium into the filtrate for excretion and reabsorb sodium and water in return. Antidiuretic hormone can increase the rate of water reabsorption in this final region of the nephron, concentrating the urine further. Micturition: occurs when the bladder walls become stretched as the bladder fills with 200–400 mL of urine. Nerve impulses are conducted to the micturition centre of the spinal cord (S2 and S3 segments), where a reflex arc produces reflex contraction of the detrusor muscle in the wall of the bladder. However, as adults we are able to override this reflex emptying urge through our conscious control of the voluntary, external urinary sphincter muscle. This is a skill that young children have to learn around the age of 2–3 years to achieve continence.
Micturition: occurs when the bladder walls become stretched as the bladder fills with 200–400 mL of urine. Nerve impulses are conducted to the micturition centre of the spinal cord (S2 and S3 segments), where a reflex arc produces reflex contraction of the detrusor muscle in the wall of the bladder. However, as adults we are able to override this reflex emptying urge through our conscious control of the voluntary, external urinary sphincter muscle. This is a skill that young children have to learn around the age of 2–3 years to achieve continence.URINARY TRACT INFECTION (P641)
PATHOLOGY: Key facts
Infection and inflammation of the urethra is called urethritis, and when the bladder is involved, cystitis. Approximately, 20% of women will experience at least one episode of urinary tract infection (UTI). This high incidence is thought to be due to the short female urethra (4 cm) making the entry of organisms from the rectum (e.g. Escherichia coli) and vagina much easier. Poor toilet hygiene and sexual activity increase the risk of infection, as does the presence of an indwelling urinary catheter or compression of the bladder by the uterus during pregnancy. UTI is much rarer in men, although men aged over 65 developing urinary obstructive problems due to an enlarged prostate are prone to UTI.
PRIORITIES FOR NURSING CARE
The focus is on preventing UTI:
 Patient education about personal hygiene associated with defecation (wipe from front to rear and wash hands thoroughly) and sex (both partners should wash their hands and genitals thoroughly before sex and, if problems persist, use condoms).
Patient education about personal hygiene associated with defecation (wipe from front to rear and wash hands thoroughly) and sex (both partners should wash their hands and genitals thoroughly before sex and, if problems persist, use condoms). Drinking large amounts of fluid helps dilute urine and prevent a build-up in concentration of organisms; citrus fruit juices may also assist.
Drinking large amounts of fluid helps dilute urine and prevent a build-up in concentration of organisms; citrus fruit juices may also assist.If the patient has an indwelling catheter:
There is no evidence to support the use of:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree