6 Caring for the patient with a disorder of the endocrine system
ANATOMY AT A GLANCE
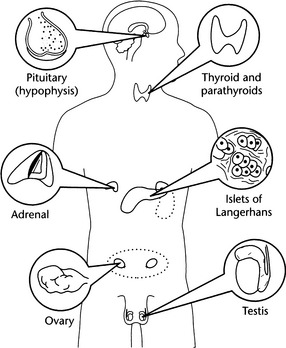
The endocrine system does not constitute a single organ. It consists of a series of glands scattered throughout the body whose function is to secrete hormones which are usually delivered by circulating blood to their target organs. Sometimes hormones act on neighbouring cells without needing to be carried in the blood stream, (paracrines) or even within the cell that secreted them (autocrines). Endocrine glands can either make up a whole organ as in the thyroid, or can be part of a larger organ such as the islets of Langerhans within the pancreas. Hormones regulate the functioning of their target organs and are therefore essential for the maintenance of a stable internal environment. Figure 6.1 shows some of the main endocrine glands in the body.
The endocrine system is closely linked to the nervous system and some chemical molecules can either act as a hormone or a neurotransmitter such as epinephrine (adrenaline). This neuro-endocrine linkage is closest in the hypothalamus gland, a small part of the brain inferior to the thalamus, which acts as the overall controller of the endocrine system. Adjacent to the hypothalamus is the pituitary gland, which is divided into an anterior and posterior lobe. Hormones released by hypothalamus generally control the hormone secretions of the anterior lobe of pituitary gland which in turn regulate many aspects of body function.
PHYSIOLOGY YOU NEED TO KNOW (P551)
A typical example of how the hypothalamus and pituitary work together is provided by the way the hypothalamus secretes thyrotrophin-releasing hormone. This stimulates the anterior pituitary to produce thyroid-stimulating hormone (TSH), which in turn stimulates the thyroid gland to secerete the thyroid hormones T3 and T4. These hormones play a large part in controlling basal metabolic rate, and are also important in growth and development. There are six other ‘releasing’ hormones produced by the hypothalalmus, which stimulate the anterior pituitary to release further hormones which act elsewhere in the body. For example, the corticotropin-releasing hormone stimulates the anterior pituitary to produce the adrenocorticotropic hormone (ACTH) which in turn stimulates the adrenal glands to produce glucocorticoids such as cortisol.
 Glucagon production increases in response to a falling blood glucose level and its main effect is on liver cells leading to a breakdown of glycogen and an increase in blood glucose levels.
Glucagon production increases in response to a falling blood glucose level and its main effect is on liver cells leading to a breakdown of glycogen and an increase in blood glucose levels. Insulin production increases as blood glucose levels rise. Its main effect is on muscle and adipose (fat) tissue where it promotes the removal of glucose from the blood and into the cells for storage as glycogen (muscle cells) and triglycerides (adipose tissue). In the liver, insulin promotes the utilization of glucose for energy production and storage as glycogen.
Insulin production increases as blood glucose levels rise. Its main effect is on muscle and adipose (fat) tissue where it promotes the removal of glucose from the blood and into the cells for storage as glycogen (muscle cells) and triglycerides (adipose tissue). In the liver, insulin promotes the utilization of glucose for energy production and storage as glycogen.DIABETES MELLITUS (P557)
PATHOLOGY: Key facts
Diabetes is a group of disorders of carbohydrate, fat and protein metabolism. The consequences of this disorder are profound, typically involving chronic elevated blood sugar levels (hyperglycaemia), degenerative vascular changes and damage to the nervous system (neuropathy). The damage that occurs both to the large blood vessels and the microcirculation has many serious debilitating effects. Few systems of the body escape the long-term effects of diabetes.
Two types of diabetes mellitus are recognized:
 Type 1 is caused by the destruction of the beta cells in the islets of Langerhans. It is thought that this is an autoimmune response associated with genetic and environmental factors. It typically develops early in life and although the onset of symptoms can be very rapid, the destructive process may have been active for several years prior to clinical signs emerging.
Type 1 is caused by the destruction of the beta cells in the islets of Langerhans. It is thought that this is an autoimmune response associated with genetic and environmental factors. It typically develops early in life and although the onset of symptoms can be very rapid, the destructive process may have been active for several years prior to clinical signs emerging. Type 2 develops as the islets gradually reduce their output of insulin or there is increased resistance in the peripheral tissues to the action of insulin. Onset is slow and this condition is associated with obesity and lack of exercise. Although the typical age of onset is 50–70 years, the growing problem of obesity in western society is now resulting in the development of Type 2 diabetes amongst children and young adults who are seriously overweight. There is also a strong genetic influence with Type 2 diabetes being far more common in some families and in certain ethnic groups. For example, in the UK, Pakistanis and Bangladeshis are five times more likely than the general population to develop Type 2 diabetes, whilst Indians are three times more likely.
Type 2 develops as the islets gradually reduce their output of insulin or there is increased resistance in the peripheral tissues to the action of insulin. Onset is slow and this condition is associated with obesity and lack of exercise. Although the typical age of onset is 50–70 years, the growing problem of obesity in western society is now resulting in the development of Type 2 diabetes amongst children and young adults who are seriously overweight. There is also a strong genetic influence with Type 2 diabetes being far more common in some families and in certain ethnic groups. For example, in the UK, Pakistanis and Bangladeshis are five times more likely than the general population to develop Type 2 diabetes, whilst Indians are three times more likely.Effects on the Patient
 Immediate:
Immediate: Long-term effects are many and varied. The following list notes only the more common:
Long-term effects are many and varied. The following list notes only the more common: Acute metabolic emergencies:
Acute metabolic emergencies:WHAT TO LOOK OUT FOR
Type 1 and Type 2 diabetes tend to have different presentations and these are summarized in Table 6.1.
Table 6.1 Classification of diabetes mellitus
| Type 1 | Type 2 | |
|---|---|---|
| Synonyms | Juvenile onset | Maturity onset |
| Age of onset | Usually before 30 years | Usually after 40 years |
| Type of onset | Frequently sudden | Usually gradual |
| Presentation | Polydipsia, polyuria | Often asymptomatic |
| Bodyweight | Thin | Usually (80%) obese |
| Ketoacidosis | Ketosis-prone | Ketosis-resistant |
| Control of diabetes | Difficulty; brittle | Generally easy |
| Control by diet alone | Not possible | Frequently possible |
| Control by oral agents | Not possible | Frequently possible |
| Long-term complications | Frequent | Frequent |
The diagnosis of diabetes is made from:
 Many patients with Type 2 diabetes do not present with the classic signs of Type 1, and the diagnosis may be made from a random urine test or capillary blood test carried out as part of a general health assessment.
Many patients with Type 2 diabetes do not present with the classic signs of Type 1, and the diagnosis may be made from a random urine test or capillary blood test carried out as part of a general health assessment. Type 2 diabetes may present in a middle-aged patient who is complaining of generally feeling unwell and tired all the time but with no specific symptoms.
Type 2 diabetes may present in a middle-aged patient who is complaining of generally feeling unwell and tired all the time but with no specific symptoms. Type 2 diabetes may be discovered in the patient whose presentation is due to symptoms of long-term complications such as angina, eye problems or peripheral vascular disease.
Type 2 diabetes may be discovered in the patient whose presentation is due to symptoms of long-term complications such as angina, eye problems or peripheral vascular disease. Pruritus of the vulva due to infection associated with glucose deposited from the urine. Males may complain of a swollen and inflamed glans penis (balanitis) due to the same effect.
Pruritus of the vulva due to infection associated with glucose deposited from the urine. Males may complain of a swollen and inflamed glans penis (balanitis) due to the same effect. Microalbuminuria or proteinuria may be detected upon dipstix testing of the urine. These are serious indicators of developing vascular complications of diabetes.
Microalbuminuria or proteinuria may be detected upon dipstix testing of the urine. These are serious indicators of developing vascular complications of diabetes.MEDICAL MANAGEMENT
It is now thought that the tighter the control of blood glucose levels, the lower the risk from long-term complications. Medical management therefore assesses diabetic control by measuring concentrations of a fraction of the haemoglobin molecule known as glycated haemoglobin (HbA1c). Measurements of this fraction of haemoglobin give a reliable estimate of average blood glucose levels over the preceding 6–8 weeks. This can be used to check against the self-assessed capillary blood glucose results that the patient has been recording in their diary. It is possible that patients who are not adhering to their medication and dietary regimens may falsify results leading all concerned to an inaccurate view of the extent of metabolic control. This deception can be very damaging to the patient in the long term, and needs to be (tactfully) challenged if detected. It is, however, a delicate balancing act between tight glycaemic control and avoiding the risk of hypoglycaemic episodes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree