13 Caring for the patient undergoing radiotherapy
Introduction
After surgery, radiotherapy is the most effective curative treatment for cancer (Burnet et al 2000). Approximately 50% of patients in the UK will receive radiotherapy. Unlike the treatments discussed in previous chapters that are given systemically, the value of radiotherapy is in the local management of cancer. The success of radiotherapy is dependent on how bulky the tumour is, how sensitive the tissues are to radiation and the location of the tumour.
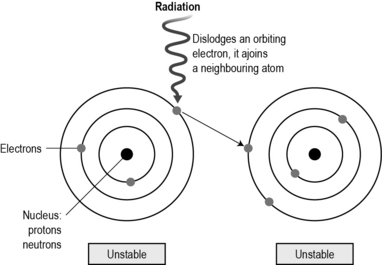
Radiation is a natural part of the electromagnetic spectrum. At one end of the electromagnetic spectrum are radio waves which have low energy and bounce around us; at the other end of the spectrum, X-rays, beta and gamma rays are highly energised and can penetrate into the body, causing ionisation. Ionisation is where the atoms within the cell are altered by the radiation. Atoms are electrical in nature. When they come into contact with radiation, the highly energised waves from the radiation cause an orbiting electron to be dislodged and join an adjacent atom which is said to be ionised (Fig. 13.1).
There are four principles (‘four Rs’) that support our understanding of how radiotherapy works:
• Repair: radiotherapy damages cells both directly and indirectly. Directly, if the damage to DNA is great, the repair genes will not be able to fix the problem and the cell will commit suicide or undergo apoptosis. Indirectly, the radiotherapy interacts with oxygen and water molecules in the cell to damage DNA as it is synthesised. Very few cells are killed straight away – it takes several cell divisions before the cell dies. Cells that die immediately are very radiosensitive, such as lymphocytes and germ cells. These are very vulnerable and responsive to radiotherapy.
• Reoxygenation: the success of radiotherapy depends on the presence of oxygen. Many cancers have a poor blood supply and are often hypoxic. This reduces the indirect action of radiotherapy which requires oxygen to damage the synthesis of DNA. To maximise the amount of oxygen, external radiotherapy is generally given in fractions. These are individual doses of radiotherapy which allow well-oxygenated cells to be killed, making way for hypoxic cells to have access to more oxygen, making them more sensitive to the next fraction of radiotherapy. Fractionisation also allows normal cells to repair and repopulate which minimises side effects.
• Redistribution: those cells in G0 will not be killed initially as they are not actively in the cell cycle, but as cells that are actively cycling die, cells in G0 are recruited into the cell cycle to replace damaged cells. Giving fractions over a period of days/weeks means that cells are more likely to be in the cell cycle and be killed. Cells are most sensitive in the M and G2 phase.
• Repopulation: cancer cells that are not actively dividing when the radiotherapy is given will start to divide after the dose, in order to replace those cells destroyed. If another dose of radiation is given, these cells will also be damaged. If the cancer repopulation happens more quickly than the radiotherapy is given, the success of the treatment will be reduced. For example, when radiotherapy is given, a number of cancer cells are killed off and other cancer cells repopulate to replace those lost. If there is a delay in the treatment schedule, these cancer cells will continue replicating, reducing the chance of success. Some radiotherapy schedules, such as accelerated hyperfractionated (CHART) radiotherapy, are give twice a day to try to deal with the problem of cancer cells repopulating more quickly than normal cells.
Read Rosenfield and Stahl (2006) (see References). Discuss the role of radiotherapy and the use of other strategies used to manage bone pain, and the nursing implications for each, with your mentor
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree