15. Care of the patient requiring thoracic surgery
Emma Gardner
CHAPTER CONTENTS
Introduction275
An overview of the respiratory system and the mechanics of breathing276
Respiratory assessment280
Common disorders requiring surgical intervention283
Specific investigations required prior to surgery286
Preoperative care289
Thoracic surgical procedures290
Postoperative care293
Specific health education/patient teaching and preparation for discharge297
Conclusion298
Introduction
Respiratory disease kills more people than coronary artery disease and accounts for over £2.5 million every year. Social inequalities cause a higher proportion of deaths in respiratory disease (44%) than any other disease. Seven per cent of the UK adult population have a long-term respiratory complaint and it is the main cause for absenteeism from work (British Thoracic Society, 2007). Thoracic surgery was initially developed in the early 20th century to aid the treatment of suppurative chest diseases – TB, bronchiectasis and emphysema. More recently there has been a resurgence in thoracic surgery for various reasons but primarily in response to the NHS cancer plan in the UK. Between 2004 and 2005, approximately 14,000 thoracic surgical procedures were performed in the UK, of which 45% were for cancer (British Cardiothoracic Society, 2008).
In the UK, there are an estimated 3 million people with chronic obstructive pulmonary disease (COPD) – an umbrella term for chronic bronchitis and emphysema – and COPD accounts for more than 10% of all acute medical admissions. Of those admitted to hospital for COPD, one in ten will die in hospital, one in three will die within 6 months and 43% will die within 12 months of hospital admission (British Lung Foundation, 2003). It is the fifth biggest killer worldwide, claiming 30,000 deaths a year in England and Wales. By 2020, COPD is predicted to be the third biggest killer in the world. In response to these statistics, a Senior Lung Policy Lead has been appointed within the Department of Health to improve the prevention, care and management of respiratory disease. A new National Service Framework for COPD is to be developed, with publication expected within 2008 and implementation aimed for 2009 (DoH, 2008).
It is essential for healthcare professionals working within the speciality of thoracic surgery to understand the anatomy and the physiology of the respiratory system, the relationships between the structures of the ribs, pleura, lungs, chest wall and diaphragm, together with the associated structures of the mediastinum. An appreciation of the mechanics and regulation of breathing is also important when considering changes in respiratory pattern.
This chapter begins with an overview of respiratory anatomy and physiology. This is followed by an examination of respiratory disorders requiring surgical intervention, the care required by patients undergoing surgical intervention and the associated nursing care.
An overview of the respiratory system and the mechanics of breathing
The primary function of the respiratory system is the efficient transfer of oxygen from the atmosphere, through the respiratory tract to the alveoli within the lungs, and the elimination of carbon dioxide in the opposite direction. This function is facilitated by the process of breathing. Breathing can be described as an automatic, rhythmic process, which is centrally regulated within the brainstem and results in contraction and relaxation of the skeletal muscles of the diaphragm, ribcage and abdomen, with the consequent movement of gas in and out of the pulmonary alveoli.
Respiration is the overall process (which includes breathing) of controlled oxidation of carbohydrates and fat, to generate energy within all cells of the body, and the production of carbon dioxide as a waste product.
This section will consider the structure and function of the respiratory system and the manner in which ventilation and gaseous diffusion takes place.
Structure and function
The thorax contains two lungs, each consisting of airways, an extensive blood supply and elastic connective tissue. The right lung consists of three lobes and the left lung has two. A division of the left upper lobe, called the lingula, arguably corresponds to the right middle lobe. The airways, which are the conducting passages for airflow into and out of the lungs, commence with the nose and mouth and include the pharynx and larynx (see Ch. 12 for details of anatomy and physiology). The trachea, the beginning of the lower respiratory tract, commences below the larynx and continues into the mediastinum, where it divides into the right and left main bronchi. The adult trachea averages 2–2.5 cm in diameter, and ranges from 10 to 12 cm in length. The trachea remains patent through the support of 16–20 C-shaped cartilaginous rings. Posteriorly, situated directly behind the trachea, a thin muscle extends between the open ends of the cartilage, which stretches to allow the passage of food down the oesophagus. A bolus of food passing down the oesophagus temporarily decreases the lumen of the trachea.
At the point of tracheal bifurcation into the right and left main bronchi, there is a sharp dividing cartilage, the carina. The carina helps to divide airflow to the right and left sides, minimizing turbulence. The right main bronchus angles off the midline at 20–30°, with the left main bronchus deflecting at a sharper angle of 45–55°. The consequence of this difference is that inhaled or aspirated objects in upright subjects tend to follow the straighter course into the right main bronchus. In supine subjects, aspirated or inhaled objects go into the dependent segments of the lung.
Functionally, the lungs can be divided into two zones: the conducting airways and the respiratory zone. The conducting airways (the volume of which is referred to as anatomical dead space) do not contain alveoli, and therefore do not participate in gaseous exchange. Gaseous exchange takes place in the alveolar-containing regions of the lung, called the respiratory zone, which accounts for most of the lung volume.
The conducting airways
The right and left main bronchi subdivide into lobar and then segmental bronchi. Terminal bronchioles, the smallest airways without alveoli, are the product of smaller subdivisions. These airways become progressively narrower, shorter and more numerous as they penetrate the lung. The terminal bronchioles subdivide further into respiratory bronchioles, which contain some alveoli within their walls, and therefore enter the respiratory zone.
By convention, the conducting airways can be broadly categorized into two distinct types: cartilaginous bronchi and membranous bronchioles. The trachea, main bronchi and subsequent divisions of the bronchi contain supporting cartilaginous plates within their walls. The cartilaginous plates maintain patency in the large airways, and enable the bronchi to dilate or constrict independently of lung volume. As the bronchi progressively subdivide, the cartilage gradually disappears. In airways of ≤1 mm, i.e. terminal bronchioles and further subdivisions, the cartilage disappears completely.
Additionally, the bronchi are characterized by a pseudostratified columnar epithelium on spiral bands of smooth muscle and ciliated, mucus-producing epithelium. The ‘mucociliary escalator’ is a significant function of the respiratory system, trapping dust and other inhaled particles in the mucus, which along with scavenging macrophages are swept up to the larynx by the cilia and coughed out, swallowed or removed by nose blowing. This mechanism may contribute to airway obstruction when patients are unable to cough adequately to clear secretions, either because of tracheal intubation, poor cough reflex, or pain following thoracic surgery.
The respiratory zone
The respiratory bronchioles contain some alveoli within their walls and subdivide finally into the alveolar ducts, which are completely lined with alveoli. These airways, lined with a simple cuboidal epithelium, contain no cartilage within their walls. An important functional difference between the bronchi and the bronchioles is that the latter are embedded directly into the connective tissue framework of the lungs, and, with no cartilage support, their diameter is dependent on lung volume.
The alveoli are thin-walled sacs, each approximately 0.3 mm in diameter and covered in a network of fine capillaries. The surface tension of the thin film of liquid within the alveoli would tend to cause inward collapse of the air space, but this is prevented by a secretion from the cells lining the alveoli. The secretion contains surfactant, which lowers the surface tension, thereby preventing alveolar collapse. Collapse of these small air spaces remains a potential problem, and frequently occurs in respiratory disease.
Pleura
The shape of the lungs conforms to that of the thoracic cavity, through a balancing of tensions within the thorax, held in balance by the pleura. The pleura is a double membrane: the visceral pleura covers the surface of the lung and doubles back as the parietal pleura, which covers the internal surface of the chest wall. The visceral pleura is devoid of a sensory nerve supply, but the parietal pleura receives innervation from the intercostal and phrenic nerves, providing pain and sensation properties.
The two pleura function as one unit because of the small volume of pleural fluid existing between the two layers. This fluid acts as a lubricant to permit the sliding of one layer across the other during respiratory movements, but does not allow the pleura to be pulled apart (rather as two plates of glass with a small drop of water between them cannot be separated except by sliding apart). The pleura, acting together, permit the transfer of movement from the respiratory muscles of the chest wall to the lungs, facilitating the variations of intrathoracic pressure, which are vital for respiratory function.
The tendency of the lungs to pull away from the chest wall and collapse is due to the natural elasticity of the pulmonary connective tissue, and the surface tension in the fluid lining the alveoli. The negative intrapleural pressure balances these tensions throughout the entire respiratory cycle. The negative intrapleural pressure is a consequence of the external forces on the pleura in the form of the inward pull of the lungs away from the chest wall, and outward movements of the chest wall.
Removal of inhaled particles
Filtration of inspired air is accomplished by large hairs within the nose and by the nasal mucosal membrane, which traps inhaled particulate matter. The direction of the inspired airstream changes abruptly at the nasopharynx, causing particulate matter to land on the back wall of the pharynx. The tonsils and adenoids located nearby provide the immunological defence against biologically active inspired material. Smaller inhaled particles may reach the lower airways, some of them lodging in the mucous epithelium, and are removed via the mucociliary escalator, or by reflex coughing or sneezing. Some small particles remain suspended as aerosols and are simply exhaled. Alveoli are not ciliated, and particles that deposit there are engulfed by macrophages, and removed from the lung via the lymphatic system or the blood flow.
Nasal breathing is the normal mechanism for air entry because of the additional pulmonary defence mechanisms it provides. Mouth breathing is necessary during colds (when the nasal passages are congested) and when large volumes of air need to be moved in and out, e.g. during exertion. Mouth breathing is a basic physiological response to dyspnoea, since the nasal turbinates create twice the resistance to airflow through the nose, compared with airflow through the mouth. Oral breathing bypasses the protective mechanisms of the nose, thereby allowing unwarmed, unfiltered, dry air to enter the tracheobronchial tree.
Inspiration and expiration
The rate and depth of respiration is a complex activity regulated by the respiratory centre in the medulla oblongata within the brainstem. Breathing is regulated to some extent through voluntary (behavioural) control, where breathing may be temporarily suspended or altered. The main regulation is through metabolic (automatic) control. Voluntary control of breathing allows ancillary actions related to breathing to occur: e.g. talking, singing, swallowing, straining, sneezing and coughing. Metabolic control serves the basic body requirements for oxygen.
The respiratory centre receives sensory input from many sources, including chemoreceptors and proprioceptors. Chemoreceptors are receptors that respond to changes in the chemical composition of blood or other fluid. Central chemoreceptors are found on the brainstem surface surrounded by brain extracellular fluid. They are sensitive to changes in hydrogen ion concentration (pH), where an increase, i.e. a fall in pH, stimulates ventilation. Carbon dioxide dissolved in cerebrospinal fluid causes a fall in pH, and is a powerful stimulus to respiration. Peripheral chemoreceptors are located in the carotid bodies at the bifurcation of the common carotid arteries, and in the aortic bodies above and below the aortic arch. The peripheral chemoreceptors respond to decreases in arterial oxygen concentrations (PaO 2) and increases in arterial carbon dioxide levels (PaCO 2). These receptors are responsible for the increase in ventilation that occurs in response to arterial hypoxaemia. A fall in oxygen concentration is a stimulus to respiration, but only a weak one. It becomes more important in chronic obstructive pulmonary disease where there is tolerance to an established rise in levels of carbon dioxide.
The rhythmicity of respiration is controlled by the pneumotaxic centre in the pons, responding to impulses from the proprioceptors, or lung stretch receptors, which are believed to lie within the smooth muscle of the bronchi and possibly the bronchioles. They respond to distension of the lung, which dilates and stretches the airways and alveoli, with the effect of inhibiting further inspiratory activity. The opposite response is also seen: i.e. deflation of the lungs tends to initiate inspiratory activity. The stretch receptors help to prevent overinflation of the lung, and, in the presence of airway narrowing or slow inspiration, their delayed activation allows inspiration to last longer until an adequate tidal volume is achieved.
Irritant receptors are thought to lie between epithelial airway cells, and are stimulated by noxious gases, cigarette smoke, inhaled dusts and cold air. They are similar to receptors found within the nose, nasopharynx, larynx and trachea. Various responses may be initiated, such as sneezing, coughing and bronchoconstriction. It is possible that these receptors play a role in the bronchoconstriction of asthma, as a result of their response to released histamine.
The mechanics of breathing
Gas flows from a region of higher pressure to one of lower pressure. When the total pressure in the alveoli is equal to atmospheric pressure, there is no airflow. For inspiration to occur, alveolar pressure must be less than atmospheric pressure, and the reverse for expiration. There are two ways of creating the pressure difference necessary for inspiration to occur: alveolar pressure can be lowered, as in natural breathing, or airway pressure can be raised, as in positive pressure ventilation by mechanical ventilators.
Inspiration is the active phase of breathing, during which time the diaphragm and external intercostal muscles contract. The contraction of the diaphragm forces the abdominal contents downwards, and the contraction of the intercostal muscles produces elevation of the ribs. This results in expansion of the thoracic cavity, and lowering of the pressure in the pleural space surrounding the lungs. As the pressure falls in the pleural space, the distensible lungs expand passively, causing the required pressure drop within the alveolar ducts and air spaces. As the pressure decreases, air flows down the airways into the alveolar spaces until the pressures are equalized, marking the end of the inspiratory phase.
During expiration, which is generally the passive phase, the diaphragm and intercostal muscles relax, allowing the elastic recoil of the lungs to occur, which increases the alveolar pressure, and gas flows out of the lungs. During exercise and voluntary hyperventilation, expiration may become active rather than passive. The significant muscles of expiration are the muscles of the abdominal wall, including the rectus abdominis, the internal and external oblique muscles and the transversus abdominis. When these muscles contract, intra-abdominal pressure is raised, and the diaphragm is pushed up.
Other muscles which may be used to assist respiration are the accessory muscles in the neck and shoulders, the scalene muscles which elevate the first two ribs, and the sternomastoid muscles which raise the sternum. There is very little or no activity in these muscles during quiet breathing, but during exercise or laboured breathing they may contract vigorously.
The exchange of carbon dioxide and oxygen between alveolar air and the pulmonary capillaries occurs by a simple process of diffusion from areas of high concentration to areas of relatively low concentration. The large surface area of the lungs provided by the alveoli is estimated to be 50–100 m 2, and with the extremely thin blood–gas barriers of the alveolar membrane and capillary membrane, create the ideal environment for gaseous diffusion to occur. Carbon dioxide is highly soluble and diffuses much more rapidly than oxygen across the membranes.
Blood gas concentration
Oxygen is carried in the blood in two forms: dissolved and in combination with haemoglobin. The amount of dissolved oxygen is proportional to the partial pressure of oxygen, but is insufficient alone to meet the demands for oxygen by the tissues. Oxygen transported in combination with haemoglobin, i.e. oxyhaemoglobin, is the significant mode of oxygen carriage, and ensures that the dissolved oxygen within the plasma can be continuously replenished, for uptake by the tissues. Oxygen forms an easily reversible combination with haemoglobin, and will combine with or separate from the haemoglobin depending on the relative partial pressures of the surrounding plasma. Differences within the amino acid chains within the haemoglobin can produce variants of haemoglobin with diminished oxygen-carrying capacity, e.g. haemoglobin S or sickle cell.
Oxygen saturation is defined as the ratio of the concentration of oxyhaemoglobin to the concentration of desaturated (or reduced) haemoglobin, and is expressed as a percentage. Normal haemoglobin levels are approximately 15 g haemoglobin/100 mL of blood and the normal oxygen saturation level of arterial blood is 97% when all the haemoglobin is carrying oxygen to full capacity. The oxygen saturation of venous blood is about 75%, reflecting the uptake of oxygen by the tissues, and a large reserve of remaining oxygen. Arterial blood gas analysis measures the PaO 2, where the normal range is 11.5–13.5 kilopascals (abbreviated to kPa).
Lung volumes
For the purposes of measurement and description, the total volume of air in the lungs is divided into volumes and capacities, where a capacity is considered to be the combination of two or more volumes (Fig. 15.1). While breathing at rest, the volume of air moved in and out, i.e. tidal volume, TV or V T, approximates to 500 mL. The volume of air remaining in the lungs at the end of tidal expiration is the functional residual capacity (FRC), which is composed of the expiratory reserve volume (ERV) and the volume of air remaining in the lungs at the end of full expiration, called the residual volume (RV). The ERV is required when increases in breathing are needed, e.g. during exercise. From knowledge of the FRC, other volumes may be assumed. The inspiratory capacity (IC) is the maximum volume that can be inspired, and consists of the tidal volume and the inspiratory reserve volume (IRV). The latter, like the ERV, is the additional volume available during exercise, or other increased levels of breathing.
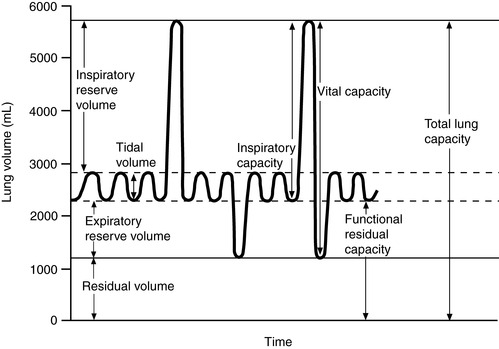 |
| Figure 15.1 Lung volumes. (From Foss, 1989.) |
At maximum inspiration, the total volume of air is the total lung capacity (TLC). The RV, the TLC and the FRC cannot be measured directly without complex equipment. However, the vital capacity can be efficiently measured, and indicates the difference in volume between the TLC and the RV. In considering these facts, it is obvious that the lungs have large reserve volumes and capacity for increased ventilation. The consequences of lung resection, therefore, may not greatly limit respiratory function if the remaining lung tissue is healthy and the reserve capacity can be utilized.
Respiratory assessment
Respiratory assessment is a vital part of the care of patients undergoing thoracic surgery. The purpose is to gain a clinical impression of the respiratory function or dysfunction and severity of symptoms, to confirm the need for medical interventions and to highlight subject areas for subsequent patient education.
Assessment of breathing
Rate, depth and quality determine the pattern of breathing. Respiratory rate is calculated by counting the number of chest movements per minute. One rise and fall of the chest is one full respiratory cycle. The normal respiratory rate at rest is 12–18 breaths per minute (in adults); it is faster in infants and children. The ratio of pulse rate to respiration is approximately 5:1. The depth of respiration is the volume of air moving in and out with each breath: i.e. the tidal volume (≅ 500 mL). The quality of breathing is compared with normal relaxed breathing, which is effortless, automatic, regular and almost silent.
Breathing patterns
Hyperpnoea
Hyperpnoea is an increased respiratory rate, being a normal physiological response, e.g. to exercise.
Tachypnoea
Tachypnoea is an increased respiratory rate, e.g. seen in fever as the body tries to rid itself of excess heat. Respirations increase by approximately seven breaths per minute for every 1°C rise in temperature. Respiratory rate also rises in pneumonia, obstructive pulmonary diseases, respiratory insufficiency, and lesions in the respiratory centre of the brainstem.
Bradypnoea
Bradypnoea is a decreased but regular respiratory rate, e.g. caused by depression of the respiratory centre in a response to opioid drugs or a brain tumour.
Dyspnoea
Dyspnoea is difficult and laboured breathing. Dilated nostrils are often apparent and the entire chest wall and shoulder girdle are raised and lowered in an exaggerated manner. Dyspnoea is a subjective complaint, being an unpleasant awareness of inappropriate effort required for breathing and can be caused by obstruction to airflow.
Hypoventilation
Hypoventilation is an alteration in the pattern of respiration, which becomes irregular or slow and shallow in depth, as a result of drugs, carbon dioxide narcosis or anaesthetic agents.
Hyperventilation
Hyperventilation is an increase in the rate and depth of respiration, e.g. in fear, anxiety, hysterical states, hepatic coma, midbrain lesions of the brainstem, and acid–base imbalance such as diabetic ketoacidosis (Kussmaul’s respiration).
Cheyne–Stokes respiration
Cheyne–Stokes respiration is a cyclical pattern in which respirations gradually increase in rate and depth and then decrease over a cycle of 30–45 seconds. Periods of apnoea (20 seconds) alternate with these cycles. This type of breathing pattern is associated with increased intracranial pressure, severe congestive heart failure, renal failure, meningitis and drug overdose. It is also commonly associated with the dying patient.
Apnoea
Apnoea is the total absence of respirations. It may be periodic or cyclical.
Respiratory noise heard without the aid of a stethoscope
Additional information about respiratory status can be determined by listening to the breathing of the patient. Descriptions of respiratory noise heard without the aid of a stethoscope are given below.
Stertorous
These noisy, snoring-type respirations, usually caused by excessive secretions in the trachea or bronchi, are commonly heard in the unconscious patient.
Stridor
Stridor is a loud, harsh, high-pitched sound on inspiration, usually caused by laryngeal obstruction. It tends to be louder and harsher than a wheeze.
Wheeze
A wheeze is a high- or low-pitched sound mainly heard on expiration. Wheezes are generated by the vibration of the walls of narrowed airways as air travels at high velocity through them. The diameter of the airway may be reduced by bronchospasm, mucosal oedema or by foreign objects. The pitch of the wheeze is unrelated to the length of the airway, but is directly related to the degree of airway compression, i.e. the tighter the airway, the higher the pitch.
Respiratory auscultation
Respiratory auscultation is heard with the aid of a stethoscope (Fig. 15.2).
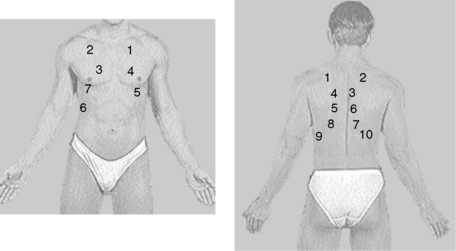 |
| Figure 15.2 Chest auscultation. The numbers represent the order in which to listen. |
Pleural rub
Pleural rub is characterized by a rough grating sound heard in both inspiration and expiration, caused by inflammation of the pleural surfaces. The pleural rub is associated with breathing but unaffected by coughing.
Additional observations
Additional observations may contribute further to the assessment of respiratory status.
Cyanosis
Cyanosis is a bluish discoloration of the skin caused by a relative decrease in oxygen saturation within the capillaries of the skin. Generally, cyanosis is said to occur when more than 5 g of deoxygenated haemoglobin is present per 100 mL of blood, i.e. when the haemoglobin level is within normal limits. Patients who are anaemic do not appear cyanotic unless they are severely hypoxaemic, and polycythaemic patients require considerably lower percentages of deoxygenated haemoglobin to display cyanosis. Cyanosis, when present in fingers, toes and ear lobes, i.e. peripheral cyanosis, is usually related to circulatory problems, such as heart failure. Central cyanosis is present when the patient’s more central regions are affected, e.g. the tongue and lips, and the trunk. This is related to a lack of oxygenation of arterial blood through the pulmonary system.
Clubbing of the digits
Clubbing of the digits is a significant manifestation within chronic cardiopulmonary disease, although the mechanism is unknown. It is identified most commonly in patients who have bronchogenic carcinoma, chronic obstructive pulmonary disease or cystic fibrosis. It is characterized by a painless enlargement of the terminal phalanges of the fingers and toes, and a widening and deepening of the nail bed.
Cough
Coughing is the most common symptom in patients with pulmonary disease, particularly within the lower respiratory tract, and can be initiated by inflammatory, mechanical or thermal stimulation of the receptors located in the pharynx, larynx, trachea, large bronchi and even the lung and visceral pleura.
The character of a cough should be evaluated using the descriptions in Table 15.1 and assessed in terms of relationship to time, patient’s position and environmental exposure. Coughs of recent onset suggest probable infection and those most noticeable on wakening suggest bronchitis or a suppurative lung disease. Nocturnal paroxysms of coughing may be indicative of asthma or left-sided heart failure. Coughs that worsen on lying down may be due to bronchiectasis or a postnasal drip from sinusitis, and those associated with food intake to aspiration of food into the trachea. A worsening cough is the most common presenting symptom of bronchial cancer. Cough also occurs for psychological reasons. Types and descriptions of coughs are shown in Table 15.2.
| Evaluation of cough | Possible causes/indications |
|---|---|
| Throat clearing | Postnasal drip |
| Dry and hacking | May be due to nervousness, viral infections, bronchogenic carcinoma or congestive cardiac failure |
| Loud and harsh | Irritation in the upper airway |
| Wheezing | Associated with bronchospasm |
| Severe, or changing in character or with position | May be bronchogenic carcinoma |
| Loose | Indicates problems in peripheral bronchi and lung parenchyma |
| Painful | May indicate pleural involvement, or chest wall disease |
| Type of cough | Description of cough |
|---|---|
| Effective | Strong enough to clear the airway |
| Inadequate | Audible but too weak to move the secretions |
| Productive | Mucus expelled as a result of the cough |
| Dry | Moisture or secretions not produced |
| Barking | Like a seal bark, indicative of a problem in the upper airways, e.g. croup, laryngotracheal bronchitis |
| Brassy/hoarse | Harsh, dry cough, associated with upper airways disorders, e.g. laryngitis, laryngotracheal bronchitis |
| Hacking | Frequent brief periods of coughing, or clearing the throat. The cough may be dry, as a result of smoking, a viral infection or postnasal drip |
Sputum
Sputum is the substance expelled from the tracheobronchial tree, pharynx, mouth, sinuses and nose. The term phlegm refers strictly to secretions from the lungs and tracheobronchial tree; phlegm may contain mucus, cellular debris, microorganisms, blood, pus and inhaled particulate matter. Normal secretions of up to 100 mL are produced daily, removed by the mucociliary escalator and swallowed unnoticed. Sputum may be described as thin, thick, viscous (i.e. gelatinous), tenacious (i.e. extremely sticky), frothy, mucoid or mucopurulent. Other observations of sputum include colour, odour and quantity (Table 15.3).
| Description of sputum | Possible causes/indications |
|---|---|
| Clear or mucoid | Viral infection, chronic bronchitis, postnasal drip |
| Yellow or green | Primary or secondary bacterial infections |
| Rusty | May indicate bacterial pneumonia |
| Malodorous | Due to lung abscess, infection from anaerobic organisms |
| Frothy and pink | Acute pulmonary oedema |
Haemoptysis
Haemoptysis is the expectoration of blood, ranging from sputum containing flecks of blood, to expectoration of large amounts of frank blood. The source of blood may be from the mouth, nose, airways or lung tissue. Careful questioning may help to differentiate haemoptysis from haematemesis. Massive bleeding can occur with pulmonary tuberculosis, lung abscesses, pulmonary embolism and pulmonary infarction, bronchiectasis and bronchogenic carcinoma. Haemoptysis can also occur following lung surgery, lung biopsy or bronchoscopy, and so the patient should be warned of these possibilities.
Chest pain
Thoracic pain is associated with a number of cardiac and pulmonary disorders. Careful assessment of precipitating factors, type and quality of pain, and the location and duration of the pain is required to distinguish between them.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

