One of the primary discoveries we made was that clinics already had many of these functions, and that IT use could be successfully enhanced through addition of a small set of functions. These functions can be separated into two categories: quality and care coordination. The amount of information related to measures of disease management, assessed in decision making, and discussed and reviewed with patients was extensive. The patient summary sheet, a succinct report that includes decision support information, facilitated discussion of disease management measures, preventive needs, and care planning, and as well as helping plan and direct the visit, could be given to the patient to take from the appointment. Voluntary use of this summary sheet improved process and outcomes measures for quality by 17% to 30% (Wilcox et al. 2005).
Additionally, software was created for the care manager that tracks self-management goals and care plans, provides reminders about best practices, and facilitates many elements of provider and patient communication. Detailed information about the tools is available at the CMP website (www.caremanagementplus.org). Use of the tracking system was a crucial component to the positive outcomes described above, as it allowed the care managers to facilitate multiple different population management and care planning components simultaneously. The system was created separately from the internally developed EHR at Intermountain Healthcare because the population management and care management tasks required a different information model and functions.
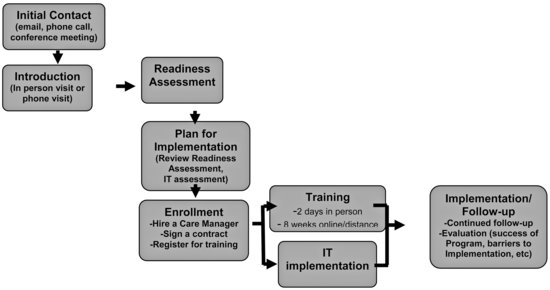
Due to the successful CMP outcomes and the overwhelming need for redesign of chronic care services, the Hartford Foundation has supported program dissemination during the past four years. An implementation process was developed for interested health care organizations (Figure 11.2) and the original care manager training curriculum was augmented and updated, still keeping the key elements of case-based learning, emphasis on geriatrics training, and identification and utilization of community resources. In addition to educating health care leaders, physicians, clinic managers, and care managers, foundation support allowed providing assessment of existing EHR functions and adoption of IT. To date, over 150 clinical teams in 15 states have implemented CMP.
With additional support from the Agency for Healthcare Research and Quality we developed the Integrated Care Coordination Information System (ICCIS) which has enhanced CMP-proven HIT functions that can interface with a health care organization’s current computer systems (including EHRs, standards, and workflow). The ICCIS is a web-based application that meets Healthcare Information Technology Standards Panel (HITSP) and Health Insurance Portability and Accountability Act (HIPAA) privacy and security requirements. The ICCIS also includes additional caregiver information, designated patient goals, improved tracking of workflow, and a dashboard of specific quality measures.
To implement provisions of the American Recovery and Reinvestment Act of 2009, the Centers for Medicare & Medicaid Services announced rulemaking provisions to include incentive payments to providers for the “meaningful use” of EHR functions for improving quality and safety, providing care coordination, examining population management, and engaging patients and their families (DesRoches & Rosenbaum 2010). CMP has identified best practices in the coordination of care and care management techniques and incorporated them into HIT. Many of these components are similar to those suggested for medical home accreditation (such as through the National Committee for Quality Assurance 2008). The medical home accreditation, however, does not include identification of patients with complex illnesses. For care coordination, the first step is to refer a patient for ongoing care management.
Table 11.1 Example Patterns and Elements of Coordinated Care Found Through CMP (N = 4,735)
The analysis of CMP also included optimal “dosage” which identified a number of care coordination patterns that worked well for patients with complex illness (Dorr et al. 2007a). In all, 22,899 services were completed for 4,735 patients. Care managers spent an average of 230.5 (± 268.2) minutes working with patients and their families per year, seeing them, on average, 4.8 times and providing 2.6 different types of services. Patterns of care management that emerged included active coordination, active disease management, or brief, intense interactions (Table 11.1). These patterns contributed to a 10% to 25% absolute increase in the accomplishment of process measures of care. The active disease management and brief intense patterns also improved the odds of achieving positive outcomes in patients with diabetes and cardiovascular disease by reducing HbA1c and LDL levels.
Curriculum
Education and acquiring skills are important to implementing new models of care. As part of implementing CMP, following the clinic or health care system’s readiness assessment and enrollment (see Figure 11.2), care managers, health care leaders, physicians, and clinic managers attend in-person training sessions (Widmier et al. 2010). CMP care managers also complete online training. After successful completion, care managers receive 30 hours of American Nurses Credentialing Center credits. Their learning starts with eight to twelve hours of in-person training for an intensive jumpstart in gaining skills in assessment of patients and families, functional, cognitive, and depression screening, and motivational interviewing (Larsen 2009). These skills are reinforced and complemented by a series of online learning modules that cover the fundamentals of care management, special issues in geriatric syndromes and concepts, chronic disease management with related assignments, case-based learning, discussions, and expert calls, and they rely heavily on resources such as the John A. Hartford Geriatric Nursing Initiative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree