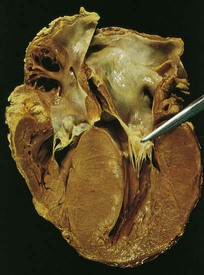
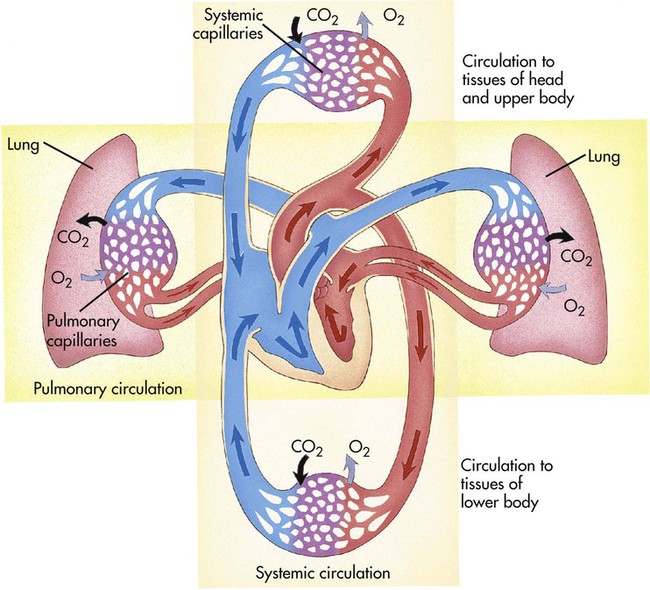
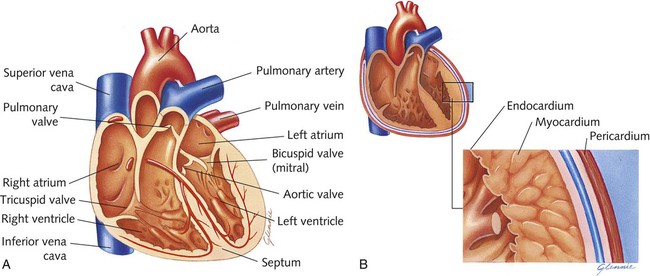
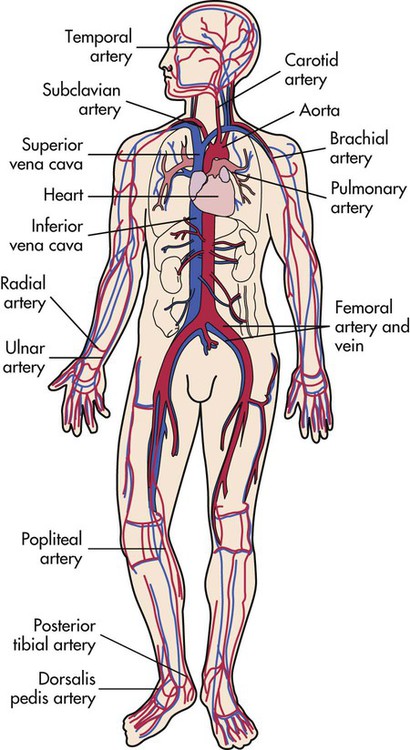
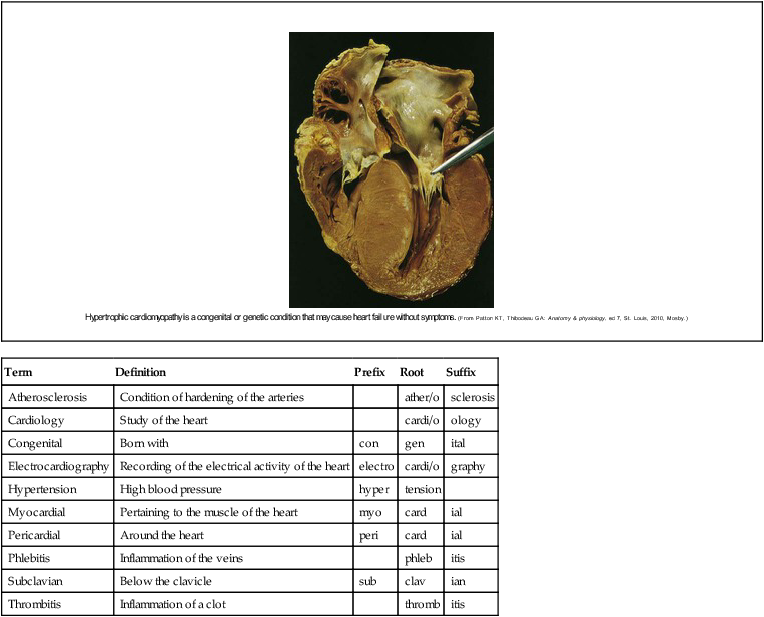
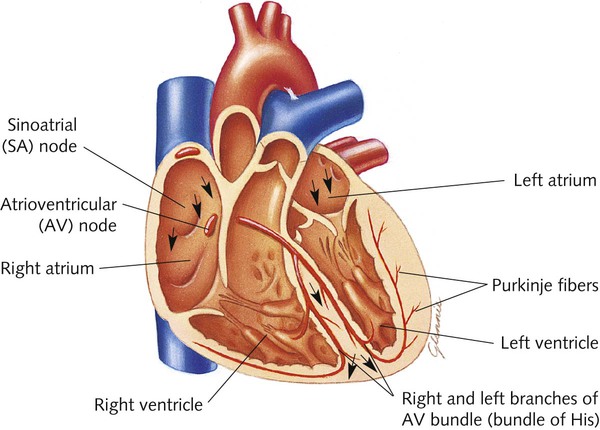
Chapter 11 Cardiovascular System Terminology* *A transition syllable or vowel may be added to or deleted from the word parts to make the combining form. The right side of the heart pumps oxygen-poor (deoxygenated) blood to the lungs, where carbon dioxide is exchanged for oxygen. This is referred to as pulmonary circulation. The left side pumps the oxygen-rich (oxygenated) blood to the rest of the body. This is referred to as systemic circulation. The blood returns to the right side of the heart from the body to complete the cycle (Fig. 11-1). The heart has four chambers (Fig. 11-2). The top chambers are called atria. The lower chambers are called ventricles. The blood enters the heart through the atria and leaves the heart from the ventricles. The septum divides the right and left sides of the heart. Four valves prevent the blood from flowing backward through the system. Two of these valves are called atrioventricular (AV) valves. They separate the atria and ventricles on each side of the heart. The semilunar valves separate the ventricles from the outgoing vessels (pulmonary artery and aorta). The valves are named according to their structure (semilunar) and location (pulmonary or aortic). The activity of the heart muscle is controlled largely by the nervous system but is affected also by the action of hormones and other mechanisms such as fluid balance. Additionally, the heart contains the only muscle tissue that can stimulate its own contractions. Specialized sinoatrial (SA) cells in the right atrium (SA node) act as a pacemaker to start a heart contraction (Fig. 11-3). The change in the electrical potential of these cells stimulates another group of cells, called the atrioventricular node (AV node), to send the impulse into the lower portions of the heart. The impulse of the AV node stimulates specialized bundles of muscle called the AV bundle or bundle of His. These fibers then stimulate the Purkinje fibers, which surround the lower portions of the ventricles. The Purkinje fibers cause the ventricles to contract. Another unique property of the heart is the ability to adjust the strength of the contractions on the basis of the amount of blood in its chambers. Without the influence of the nervous system and other controls, the heart would contract only 40 times each minute instead of the normal 60 to 90 times. The adult heart beats 10,000 times a day. The body has three main types of blood vessels (Fig. 11-4): Blood is pumped from the heart to the body by the largest artery in the body, the aorta. Fig. 11-5 shows the principal arteries of the body. The aorta branches into other arteries, which in turn branch into smaller vessels called arterioles. The blood moves from arterioles to microscopic capillaries. Gases, nutrients, and wastes are exchanged through the thin walls of the capillaries. The blood, which has now given up its oxygen, flows from the capillaries into tiny veins called venules. Venules branch together to form larger veins (Fig. 11-5). The blood is returned to the heart in the body’s largest veins, the superior vena cava and inferior vena cava. With the exception of the pulmonary artery, blood in the arteries is oxygenated. Except for the pulmonary vein, blood in veins is deoxygenated. Tracing the path of a blood cell through the heart is one way to learn the heart’s structures and understand its functions (Table 11-1). Although the heart is considered a two-sided pump to differentiate the systemic and pulmonary circulation, the two atria contract at the same time, then the ventricles contract. Deoxygenated blood enters the right atrium of the heart from the body through the inferior and superior vena cavae. Additionally, blood from the heart muscle itself returns through a structure called the coronary sinus. The blood then passes through the tricuspid valve into the right ventricle. This valve closes as the pulmonary valve opens, allowing the passage of blood from the right ventricle to the pulmonary arteries. The pulmonary valve closes as the blood enters the lungs for the diffusion of oxygen and carbon dioxide. The oxygenated blood then travels through the pulmonary veins to the left atrium. From the left atrium the blood travels through the bicuspid or mitral valve to the left ventricle. The mitral valve closes as the blood leaves the left ventricle through the aortic valve. The blood then travels through the aorta to the rest of the body. As the ascending aorta leaves the heart, it branches in three directions to supply blood to the head and upper limbs. Two coronary arteries, which supply blood to the heart, branch off of the ascending aorta. The descending portion of the aorta supplies blood to the abdominal area and lower extremities. Deoxygenated blood is returned to the heart through the inferior and superior vena cavae from the body to complete the path. TABLE 11-1 Path of the Blood through the Heart
Cardiovascular System
 Define at least 10 terms relating to the cardiovascular system.
Define at least 10 terms relating to the cardiovascular system.
 Describe the function of the cardiovascular system.
Describe the function of the cardiovascular system.
 Identify at least 10 cardiovascular system structures and the function of each.
Identify at least 10 cardiovascular system structures and the function of each.
 Identify at least three methods of assessment used to evaluate the cardiovascular system.
Identify at least three methods of assessment used to evaluate the cardiovascular system.
 Describe at least five disorders of the cardiovascular system.
Describe at least five disorders of the cardiovascular system.
Term
Definition
Prefix
Root
Suffix
Atherosclerosis
Condition of hardening of the arteries
ather/o
sclerosis
Cardiology
Study of the heart
cardi/o
ology
Congenital
Born with
con
gen
ital
Electrocardiography
Recording of the electrical activity of the heart
electro
cardi/o
graphy
Hypertension
High blood pressure
hyper
tension
Myocardial
Pertaining to the muscle of the heart
myo
card
ial
Pericardial
Around the heart
peri
card
ial
Phlebitis
Inflammation of the veins
phleb
itis
Subclavian
Below the clavicle
sub
clav
ian
Thrombitis
Inflammation of a clot
thromb
itis
Structure and Function of the Cardiovascular System
 Transport nutrients and oxygen to the body
Transport nutrients and oxygen to the body
 Transport waste products from the cells to the kidneys for excretion
Transport waste products from the cells to the kidneys for excretion
 Distribute hormones and antibodies throughout the body
Distribute hormones and antibodies throughout the body
 Help control body temperature and maintain electrolyte balance (homeostasis)
Help control body temperature and maintain electrolyte balance (homeostasis)
Heart
Blood Vessels
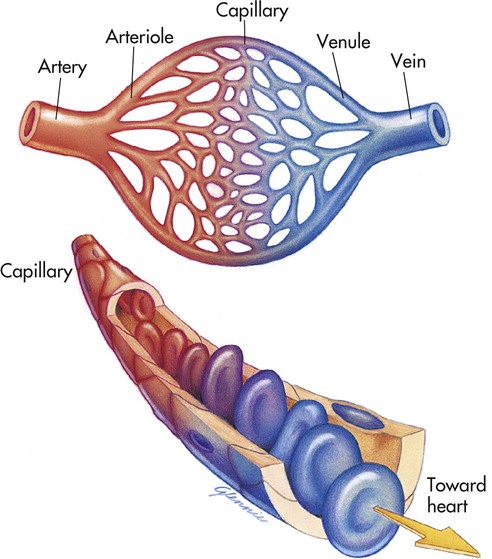
 Arteries carry blood away from the heart.
Arteries carry blood away from the heart.
 Veins carry blood back to the heart.
Veins carry blood back to the heart.
 Capillaries are microscopic vessels that carry blood between the arterial and venous vessels.
Capillaries are microscopic vessels that carry blood between the arterial and venous vessels.
Path of the Blood Through the Heart
Structure
Oxygen Content
Body
Exchange of carbon dioxide and oxygen
Superior and inferior vena cavae
Deoxygenated
Right atrium
Deoxygenated
Tricuspid valve
Deoxygenated
Right ventricle
Deoxygenated
Pulmonary valve
Deoxygenated
Pulmonary artery
Deoxygenated
Lungs
Exchange of carbon dioxide and oxygen
Pulmonary vein
Oxygenated
Left atrium
Oxygenated
Mitral valve
Oxygenated
Left ventricle
Oxygenated
Aortic valve
Oxygenated
Aorta
Oxygenated
Body
Exchange of carbon dioxide and oxygen ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cardiovascular System
Get Clinical Tree app for offline access