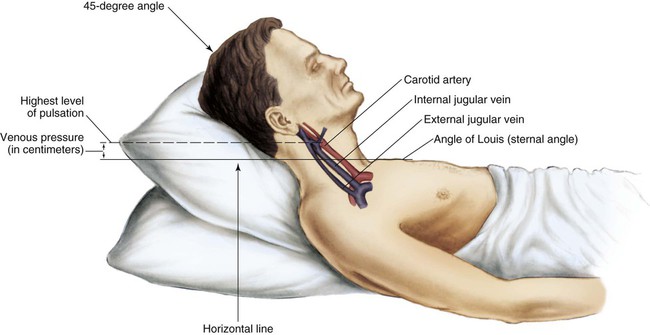
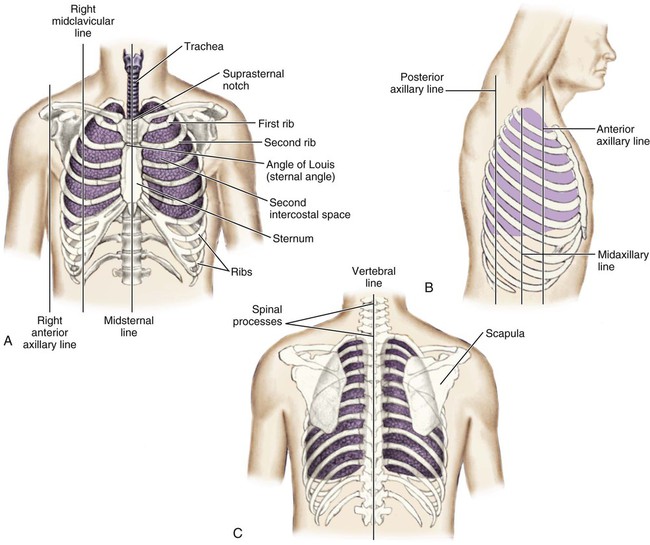
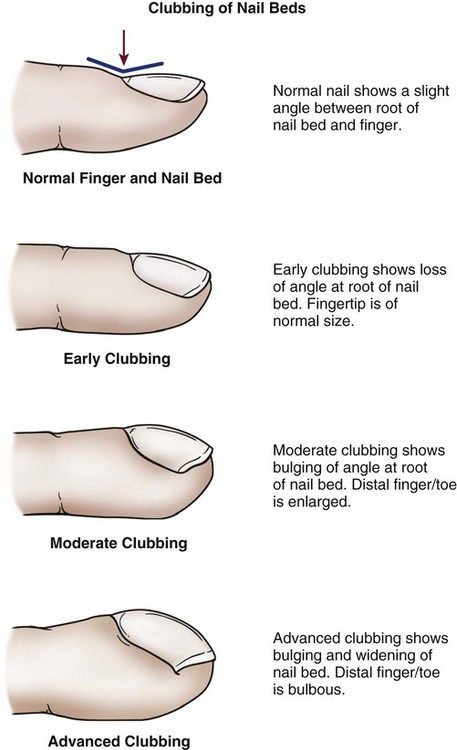
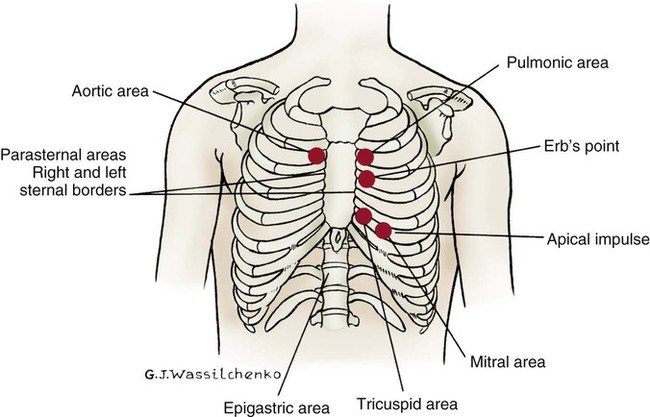
Physical assessment of the patient with cardiovascular disease is a skill that must not be overlooked in the middle of all the technology of the critical care setting.1 Data collected from a thorough, thoughtful history taking and examination contribute to both the nursing and the medical decisions about therapeutic interventions. Patient history is important because it provides data that contribute to diagnosis of cardiovascular disease and treatment plan. For a patient in acute distress, the history taking is shortened to just a few questions about the patient’s chief complaint, precipitating events, and current medications (Box 13-1). For a patient who is not in obvious distress, the history focuses on the following four areas: 1. Review of the patient’s present illness 2. Overview of the patient’s general cardiovascular status, including previous cardiac diagnostic studies, interventional procedures, cardiac surgeries, and current medications (i.e., cardiac, noncardiac, and over-the-counter medications) 3. Review of the patient’s general health status, including family history of coronary artery disease (CAD), hypertension, diabetes, peripheral arterial disease, or stroke 4. Survey of the patient’s lifestyle, including risk factors for CAD • If any evidence of CAD or risk of heart disease exists, assume that the chest pain is caused by myocardial ischemia until proven otherwise. • Questions to elicit the nature of the chest pain cover five basic areas: 1) quality, 2) location, 3) duration of pain, 4) factors that provoke the pain, and 5) factors that relieve the pain. Questions that may help elicit this information are listed in Table 13-1. TABLE 13-1 CLARIFYING CHEST PAIN SYMPTOMS BY ASKING SPECIFIC QUESTIONS • Little correlation may exist between the severity of chest discomfort and the gravity of its cause. This is a result of the subjective nature of pain and the unique presentation of ischemic disease in women, older patients, and individuals with diabetes. • Subjective descriptors vary greatly among individuals. Not all patients use the word “pain”; some may describe their problem as “pressure,” heaviness,” discomfort,” or “indigestion.” • A correlation is not always present between the location of chest discomfort and its source because of referred pain. For example, in patients with gastroesophageal reflux disease (GERD), esophageal spasm can cause visceral substernal chest pain that radiates to the left arm and jaw and may be described by patients as “heartburn.”2 • Other nonpainful symptoms that may signal cardiac dysfunction are dyspnea, palpitations, cough, fatigue, edema, ischemic leg pain, nocturia, syncope, and cyanosis. In a meta-analysis of the evaluation of stable, intermittent chest pain, a patient’s description of chest pain was found to be the most important predictor of underlying coronary disease.3 In the evaluation of acute chest pain, the 12-lead electrocardiogram (ECG) was the most useful bedside predictor for a diagnosis of ST-elevation myocardial infarction (STEMI).3 The nail beds are inspected for signs of discoloration or cyanosis.4 Clubbing in the nail bed is a sign associated with long-standing central cyanotic heart disease or pulmonary disease with hypoxemia.4,5 “Clubbing” of the nail refers to a nail that has lost the normal angle between the finger and the nail root; the nail becomes wide and convex. The terminal phalanx of the finger also becomes bulbous and swollen.6 Clubbing is rare and is a sign of severe central cyanosis (Fig. 13-1). Peripheral cyanosis, a bluish discoloration of the nail bed, is seen more commonly. Peripheral cyanosis results from a reduction in the quantity of oxygen in the peripheral extremities from arterial disease or decreased cardiac output (CO). Clubbing never occurs as a result of peripheral cyanosis. Legs are inspected for signs of peripheral arterial or venous vascular disease. The visible signs of peripheral arterial vascular disease include pale, shiny legs with sparse hair growth. Recent guidelines indicate that many individuals, especially women, can have peripheral atherosclerosis without obvious signs or symptoms.7 Venous disease causes edema of the limb, with deep red rubor, brown discoloration, and, frequently, leg ulceration. A comparison of typical assessment findings in arterial and venous diseases is presented in Table 13-2. TABLE 13-2 INSPECTION AND PALPATION OF EXTREMITIES: COMPARISON OF ARTERIAL AND VENOUS DISEASE Modified from Krenzer ME. Peripheral vascular assessment: finding your way through arteries and veins. AACN Clin Issues. 1995;6(4):631. The jugular veins of the neck are inspected for a noninvasive estimate of intravascular volume and pressure. The internal jugular veins are observed for jugular vein distention (JVD) (Fig. 13-2; Box 13-2). JVD is caused by an elevation in central venous pressure (CVP). This occurs with fluid volume overload, right ventricular dysfunction, pericardial effusion, or any condition that elevates right atrial pressure.9,10 The right internal jugular vein can be palpated for measurement of CVP in centimeters of water (Fig. 13-3; Box 13-3). Bedside ultrasound is also used to evaluate JVD and estimate CVP.11 The abdominojugular reflux sign can assist with the diagnosis of right ventricular failure. This noninvasive test is used in conjunction with measurement of JVD. The procedure for assessing abdominojugular reflux is described in Box 13-4. A positive abdominojugular reflux sign is an increase in the jugular venous pressure (CVP equivalent) of 4 cm or more sustained for at least 15 seconds.12 The thoracic cage is divided with imaginary vertical lines (sternal, midclavicular, axillary, vertebral, and scapular), and the intercostal spaces are divided by imaginary horizontal lines to serve as reference points in locating or describing cardiac findings (Fig. 13-4). The ribs are numbered from 1 (the first rib below the clavicle) to 12. The intercostal space below each rib is given the same number as the rib that lies above it. The second rib is the easiest to locate because it is attached to the sternum at the angle of Louis. This angle (also called the sternal angle) is the bony ridge on the sternum that lies approximately 2 inches below the sternal notch (see Fig. 13-4A). After the second rib has been located, it can be used as a reference point to count off the other ribs and intercostal spaces. The anterior thorax is inspected for the apical impulse, sometimes referred to as the point of maximal impulse (PMI). The apical impulse occurs as the left ventricle contracts during systole and rotates forward, causing the left ventricular apex of the heart to hit the chest wall. The apical impulse is a quick, localized, outward movement normally located just lateral to the left midclavicular line at the fifth intercostal space in the adult patient (Fig. 13-5). The apical impulse is the only normal pulsation visualized on the chest wall. In the patient without cardiac disease, PMI may not be noticeable (see Fig. 13-5). Seven pairs of bilateral arterial pulses are palpated. The examination incorporates bilateral assessment of the carotid, brachial, radial, ulnar, popliteal, dorsalis pedis, and posterior tibial arteries. The pulses are palpated separately and compared bilaterally to check for consistency.13 Pulse volume is graded on a scale of 0 to 3+ (Box 13-5). The abdominal aortic pulse can also be palpated. The brachial pulse is assessed by gently palpating the inner aspect of the slightly bent elbow with the fingers. The radial pulse is palpated in the medial area of the wrist (thumb side). The ulnar artery is palpated at the opposite side of the wrist (little finger side). The radial and ulnar arterial pulses must be assessed before an arterial line is inserted; this test, known as the Allen test, is described in Box 13-6.
Cardiovascular Clinical Assessment
History
DETERMINE
TYPICAL QUESTION
Location, radiation
Where is it?
Does it move or stay in one place?
Quality
What is it like?
Quantity
How severe is it? How frequent?
How long does it last?
Chronology
When did it begin?
How has it progressed?
What are you doing when it occurs?
What do you do to get rid of it?
Associated findings
Do you feel any other symptoms at the same time?
Treatment sought and effect
Have you seen a physician in the past for this same problem?
What was the treatment?
Personal
What do you think this is from?
Perception
Why do you think it happened now?
Physical Examination
Inspection
Face
Nail Beds and Cyanosis
Lower Extremities
CHARACTERISTIC
ARTERIAL DISEASE
VENOUS DISEASE
Hair loss
Present
Absent
Skin texture
Thin, shiny, dry
Flaking, stasis, dermatitis, mottled
Ulceration
Located at pressure points; painful, pale, dry with little drainage; well-demarcated with eschar or dried; surrounded by fibrous tissue; granulation tissue scant and pale
Usually at the ankle; painless, pink, moist with large amount of drainage; irregular, dry, and scaly; surrounded by dermatitis; granulation tissue healthy
Skin color
Elevational pallor, dependent rubor
Brown patches, rubor, mottled cyanotic color when dependent
Nails
Thick, brittle
Normal
Varicose veins
Absent
Present
Temperature
Cool
Warm
Capillary refill
Greater than 3 seconds
Less than 3 seconds
Edema
None or mild, usually unilateral
Usually present foot to calf, unilateral or bilateral
Pulses
Weak or absent (0 to 1+)
Normal, strong, and symmetric
Jugular Veins

Applying light finger pressure over the sternocleidomastoid muscle, parallel to the clavicle, helps identify the external jugular vein by occluding flow and distending it. The finger pressure is released, and the patient is observed for true distention. If the patient’s trunk is elevated to 30 degrees or more, JVD should not be present.
Abdominojugular Reflux
Thoracic Reference Points
Apical Impulse
Palpation
Arterial Pulses
Brachial, Ulnar, and Radial Pulses

Cardiovascular Clinical Assessment
Get Clinical Tree app for offline access