Chapter 8 Cardiopulmonary resuscitation
INTRODUCTION
While few resuscitation situations involving children arise without warning, it remains imperative that children’s nurses are skilled in the area of basic life support (Simpson 1994, Carter & Dearmun 1995). Paediatric basic life support (BLS) is described as the provision of cardiopulmonary resuscitation (CPR) with no devices or with bag-valve-mask ventilation or barrier devices, until advanced life support (ALS) can be provided (International Guidelines 2000). However, ‘if basic life support is not effectively delivered to the child, attempts at advanced life support are likely to prove futile’ (Simpson 1994, p 39).
As accidents remain the commonest cause of death in children and as the life expectancy of children with a variety of chronic illnesses is increasing, the need for parents, and also other members of the general public, to learn basic paediatric life support is becoming increasingly important (Carter & Dearmun 1995, Whitton 1995).
Sudden cardiac arrest is a rare event in the paediatric population; most children will show signs of physiological deterioration, sometimes hours prior to the event (Tibballs et al 2005). As outcome from cardiac arrest is poor, it is important that deteriorating patients are recognised and appropriate interventions made. A number of early warning systems to detect clinical deterioration have been developed and are now used within adult medicine (Parr et al 2001, Hodgetts et al 2002). Early warning systems are now being developed throughout paediatric medicine (Tibballs et al 2005, Duncan et al 2006, McCabe et al 2009). Most paediatric hospitals are now using or developing early warning systems, it is important that the nurse is familiar with their format and use.
RATIONALE
Commentators on both sides of the Atlantic acknowledge the importance of resuscitation as a nursing skill (AHA 2000, Resuscitation Council (UK) 2005).
Cardiac arrest in children is often the terminal event of progressive shock or respiratory failure; early signs of shock or respiratory failure must be recognised and treated to prevent cardiac arrest (International Guidelines 2000, Resuscitation Council (UK) 2005).
Many children die or suffer permanent neurological impairment each year because of respiratory failure, sudden infant death syndrome, sepsis or trauma (CDC at: www.cdc.gov/injury/wisqars/index.html). Appropriate prompt action can help avoid many of them.
Advanced life support will be futile if basic life support is not delivered effectively.
FACTORS TO NOTE
Babies and children differ from adults in a number of ways:
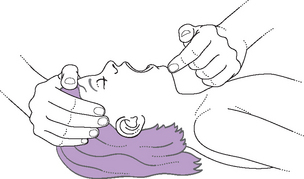
BASIC PAEDIATRIC LIFE SUPPORT
METHOD
If the lone rescuer has been taught adult basic life support then they may use the adult sequence with the addition of providing five initial breaths and performing 1 min of basic life support prior to going for help (Resuscitation Council (UK) 2005).