CHAPTER 8 Calculating in paediatrics
Key aspects
Renal impairment
Table 8.1 Development of renal function
| Age | GFR (mL/min) approx. |
|---|---|
| < 37 weeks | <25 |
| Neonate | 15–35 |
| 1–2 weeks | 35–60 |
| 2–4 months | 60–80 |
| 6–12 months | 80–110 |
| 12 months → adult | 85–150 |
Paediatric medicines
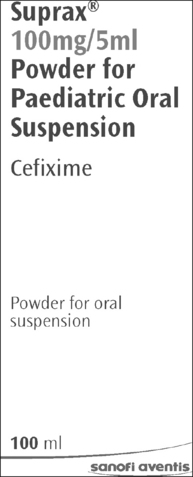
Oral route
The oral route is the most common route of administration in children and should be used where available. It is associated with less pain and anxiety, and is more cost effective than a parenteral route. It is also more convenient and less time-consuming, it requires less equipment and the need to undertake calculations may be reduced. Many children can swallow tablets and capsules but a liquid preparation may be preferred. Prescriptions for liquid preparations should include the dose in milligrams, micrograms or nanograms and not just the volume to be given. The choice between liquid and solid oral dose will depend on product availability or personal preferences. Crushing tablets or opening capsules not specifically designed for this purpose renders their use unlicensed (NMC 2008). On some occasions, it may be necessary to use a medicine in an unorthodox way, for example, administering an injectable product orally. Further advice should be sought from the pharmacy. Some products have a high osmolality and must be diluted before administration (e.g. vitamin E suspension).
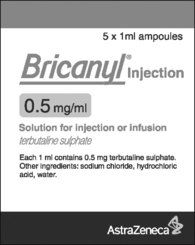
Other routes of administration
Parenteral administration is more complex and as a result presents greater risk than non-parenteral drug administration. The process involves selection of the appropriate administration device, calculating and setting the rate of infusion, and monitoring delivery. It is essential that the nurse is trained in and fully conversant with the use of the equipment.
Calculating a paediatric dose
| Normal dose | 5 mg/kg over 20 minutes |
| 5-year-old Height 108 cm | Ideal body weight 18 kg |
| 5-year-old Height 108 cm | Obese child weighs 21 kg |
| Using child’s ideal body weight | Dose 5 x 18 = 90 mg |
| Using child’s actual weight | Dose 5 x 21 = 105 mg |
Oral (enteral) syringes
A syringe exclusively for oral use is supplied when oral liquid medicines are prescribed in doses less than 5 mL (see also p. 60). Oral syringes are available in 1 mL, 3 mL and 5 mL, and supplied with a protective cap and adaptor, and a guidance leaflet. After shaking the medicine bottle, the bottle adaptor is inserted into the open neck of the bottle. The required dose is then drawn up into the oral syringe. The tip of the oral syringe is cautiously put into the child’s mouth and the plunger gently squeezed to run a small amount into the child’s mouth. The child is allowed to swallow before pushing the plunger again. The child is then given a drink to wash down the medicine and the syringe washed in warm soapy water, rinsed and dried. Alternatively, a graduated pipette may be used (see also p. 60).
Examples: Demonstration and practice
The practice examples provide the opportunity to gain competence in doing calculations and thus increase confidence. Each practice example raises a question for the reader to consider. Answers are on pp. 196–197.
Whether or not a calculation is needed, care must be taken to measure the precise dose.
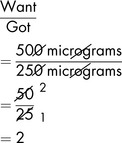
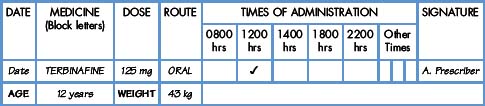
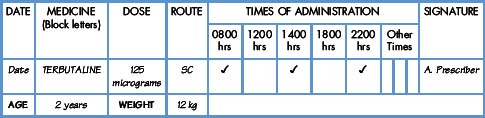
Level I Demonstration
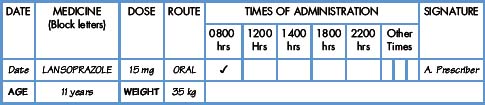
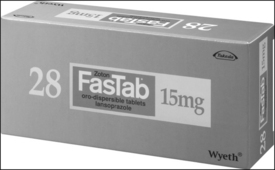
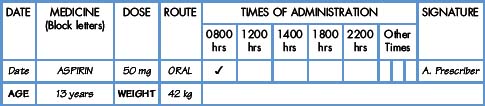
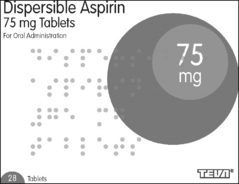
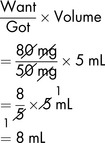
Demonstration 8.3
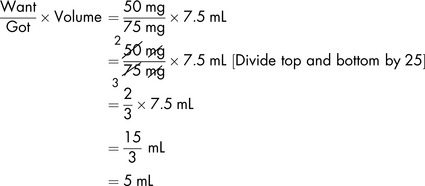
Commentary
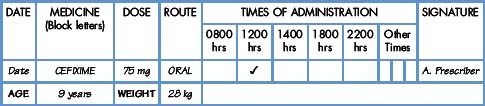
Level I Further exercises
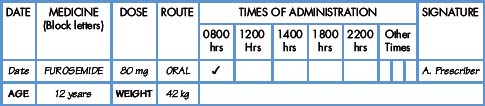
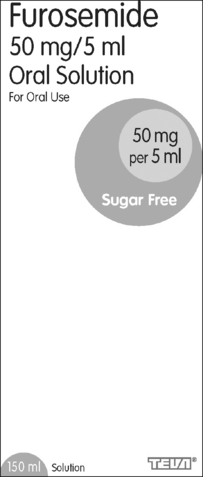
Level II Demonstration
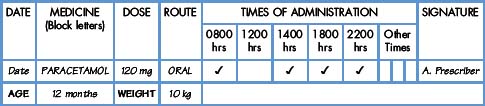
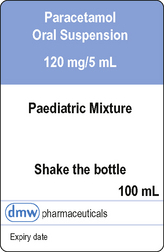
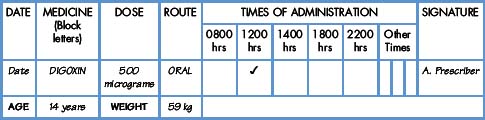
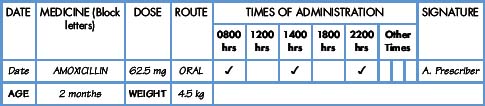
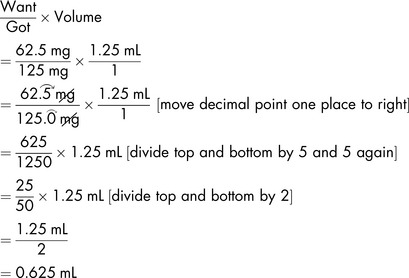
Demonstration 8.6
The medicine
Amoxicillin (Amoxil) belongs to the penicillin group. For paediatric use, it is available as a suspension (when reconstituted) containing 125 mg in 1.25 mL.
Commentary