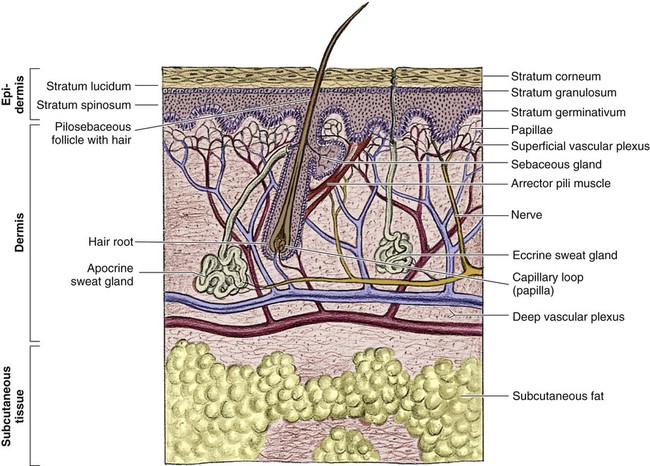
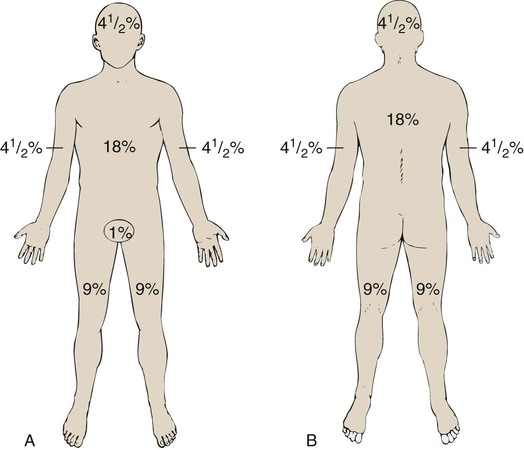
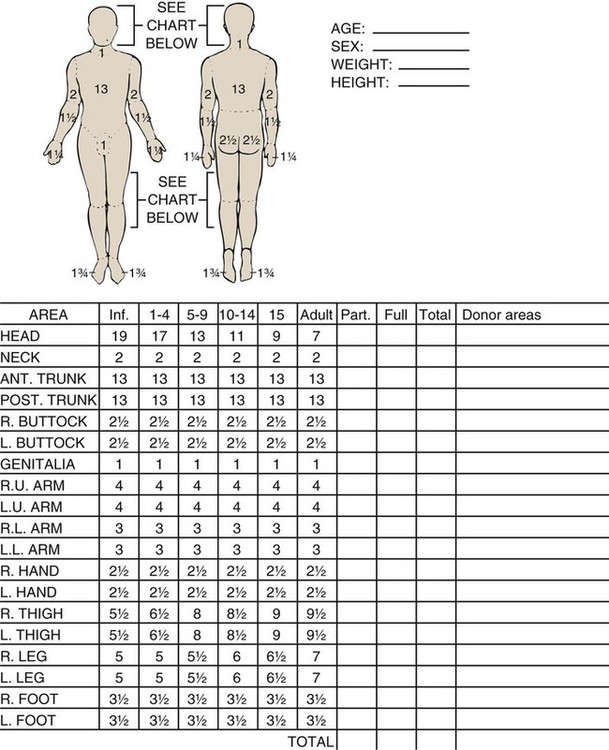
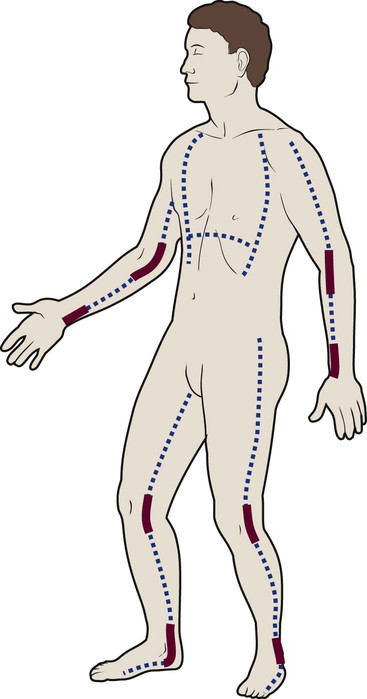
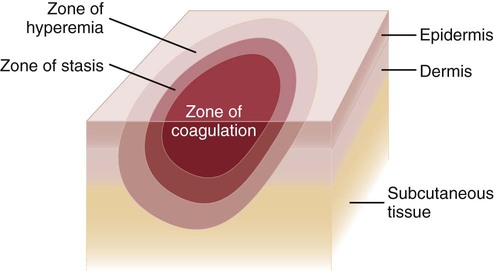
Since the late 1980s, trends of burn incidence, hospitalization, and death have all decreased.1,2 These decreases are attributed to fire and burn prevention education, management of burn patients in specialized burn centers, regulation of consumer products, and implementation of occupational safety standards. Many programs and organizations are dedicated to the prevention of burn injury. Societal changes involving decreased smoking and alcohol abuse, changes in home cooking practices, and reduced industrial employment also have contributed to the decline in burn incidence. However, in spite of a decline in overall burn incidence, because of an increase in child maltreatment (3.3 million referrals in 2010), burn injury as a result of physical abuse remains a differential diagnosis in pediatric burn patients.3 Burn injuries that require medical treatment annually number 450,000 per year.2 Burn injuries requiring hospitalization total approximately 45,000 per year, and 55% of these patients are admitted to one of the 125 specialized burn centers in the United States.2 Great advances have been made in the care of burn patients. In the mid-twentieth century, burn shock claimed many patients’ lives. If shock did not cause death, infection or respiratory insufficiency did. With improvements in fluid resuscitation, better critical care management, and the trend toward early excision and grafting, mortality rates have decreased. Focusing management on early eschar excision in patients with deeper, larger burns decreases wound sepsis, hypercatabolism, number of operations, and lengths of hospital stay.4 The skin is the largest organ of the human body, ranging from 0.2 meter squared (m2) in the newborn to more than 2 m2 in the adult. The integumentary system consists of two major layers: (1) epidermis and (2) dermis (Fig. 36-1). The outermost layer of the epidermis is 0.07 to 0.12 millimeters (mm) thick, with the deepest layer found on the soles of the feet and the palms of the hands. The epidermis is composed of dead, cornified cells that act as a tough protective barrier against the environment. It serves as a barrier to bacteria and moisture loss.5 From the surface inward, its five layers are (1) stratum corneum, (2) stratum lucidum, (3) stratum granulosum, (4) stratum spinosum, and (5) stratum germinativum. The deepest layer of the epidermis contains fibronectin, which adheres the epidermis to the basement membrane. The epidermis regenerates every 2 to 3 weeks. The second, thicker layer, the dermis, is 1 to 2 mm thick and lies below the epidermis and regenerates continuously. The dermis is composed of two layers: (1) the more superficial, papillary layer next to the stratum germinativum and (2) the deeper, reticular layer. The dermis, composed primarily of connective tissue and collagenous fiber bundles made from fibroblasts, provides nutritional support to the epidermis. The dermis contains blood vessels; sweat and sebaceous glands; hair follicles; nerves to the skin and capillaries that nourish the avascular epidermis; and sensory fibers that detect pain, touch, and temperature. Mast cells in the connective tissue perform the functions of secretion, phagocytosis, and production of fibroblasts. Beneath the dermis is the hypodermis, which contains fat, smooth muscle, and areolar tissues. The hypodermis acts as a heat insulator, shock absorber, and nutritional depot.6 A burn injury results in tissue loss or damage. Injury to tissue can be caused by exposure to thermal, electrical, chemical, or radiation sources. The temperature or causticity of the burning agent and duration of tissue contact with the source determine the extent of tissue injury. Tissue damage can occur at various temperatures, usually between 40° C (104° F) and 44° C (111.2° F). The burn wound itself is responsible for the local and systemic effects seen in the burned patient.7 Tissue damage is caused by enzyme malfunction and denaturation of proteins. Prolonged exposure or higher temperatures can lead to cell necrosis and a process known as protein coagulation. The areas extending outward from this central area of injury sustain various degrees of damage and are identified by zones of injury.8 Three concentric zones are present in burn injury: (1) zone of coagulation, (2) zone of stasis, and (3) zone of hyperemia (Fig. 36-2). The central zone, or zone of coagulation, is the site of most severe damage, and the peripheral zone is the least. The central zone is usually the site of greatest heat transfer, leading to irreversible skin death. This area is surrounded by the zone of stasis, which is characterized by impaired circulation that can lead to cessation of blood flow caused by a pronounced inflammatory reaction. This area is potentially salvageable; however, local or systemic factors can convert it into a full-thickness injury. Some of the factors that can lead to deeper wound conversion are toxic mediators of the inflammatory process, infection, inappropriate volume resuscitation, malnutrition, chronic illness, or the local wound care provided. It may take 48 to 72 hours to determine the full extent of injury in this area. The outermost area, the zone of hyperemia, has vasodilation and increased blood flow but minimal cell involvement. Early spontaneous recovery can occur in this area.7,8 Burns are classified primarily according to the size and depth of injury. However, the type and location of the burn and the patient’s age and medical history are also significant considerations. Recognition of the magnitude of burn injury, which is based on the above-mentioned factors, is of crucial importance in the overall plan of care and in decisions concerning patient management and appropriate referral to a burn center (Box 36-1).2 The patient’s age, burn size, and inhalation injury are the cardinal determinants of survival.9 A recent study of a large number of burn patients found the following factors to be the biggest predictors of patient mortality: age, percent total body surface area (TBSA), inhalation injury, coexistent trauma, pre-existing disease, and acute organ system failure.9,10 Several different methods can be used to estimate the size of the burn area. A quick and easy method is the rule of nines (or Berkow formula), which often is used in the prehospital setting for initial triage of the burn patient (Fig. 36-3). In this method, the adult body is divided into different surface areas of 9% per area. This method is modified for assessing infants and very small children and accounts for proportionate growth. For example, a 1-year-old has a head that is proportionately larger than the rest of the body, unlike in adults, so the child’s head would account for 19% of his or her TBSA, whereas the head of an adult would account for 7% of TBSA.5 Designated burn centers have access to Berkow formula charts, but local hospitals may not. Another method uses the measure of the palmar surface of the victim’s hand as a gauge for estimating burn area. The palmar surface (fingertip to wrist), which represents 1% of the TBSA, also can be useful in making burn estimates in the prehospital setting or for estimating the percentage of involvement in small and scattered areas of burn. Some studies have shown the adult hand’s TBSA is calculated to be closer to 0.8% versus 1% in a child.5 In the hospital setting, the Lund and Browder method (Fig. 36-4) is the most accurate and accepted method for determining the percentage of burn. Surface area measurements are assigned to each body part in terms of the age of the patient. This method is highly recommended for use with children younger than 10 years because it corrects for smaller surface areas of the lower extremities. It is also recommended for adult burn victims because of its accuracy. Traditionally, burn depth has been classified in degrees of injury based on the amount of injured epidermis, dermis, or both: first-degree, second-degree, third-degree, or fourth-degree burns. However, these terms are not descriptive of the burn surface. The depth of the burn is defined by how much of the skin’s two layers are destroyed by the heat source.10 Burns are classified as superficial, partial-thickness, deep partial-thickness, or full-thickness burns. These descriptions are based on the surface appearance of the wound. Superficial burns include first-degree burns. Partial-thickness wounds include various stages of second-degree burns, and full-thickness burns include third-degree burns. Four-degree burns extend through the skin to the subcutaneous fat, muscle, and even bone.10 Some authorities further separate partial-thickness burns as superficial, mid-partial, or deep-partial-thickness burns. Wound assessment involves recognition of the depth of injury and the size of burn, and it can be challenging even for experienced caregivers. Because the management of burn wounds is closely tied to the correct assessment of wound severity, some newer strategies, other than observation, are being investigated. Some of these techniques have taken into account the presence of denatured collagen, wound edema, and altered blood flow. One such technique is noncontact laser Doppler imaging, which can give a color perfusion map of the burn wound.11 Other techniques of assessing burn depth include use of vital dyes, ultrasonography, thermography, and magnetic resonance imaging.8 Research with these techniques is ongoing, but they are currently limited by their clinical usefulness at the bedside. A partial-thickness (second-degree) burn involves all of the epidermis and part of underlying dermis.5 These burns usually are caused by brief contact with flames, hot liquid, or exposure to dilute chemicals (Fig. 36-5). A light to bright red or mottled appearance characterizes superficial second-degree burns. These wounds may appear wet and weeping, may contain bullae, and are extremely painful and sensitive to air currents. These burns blanch painfully.5 The microvessels that perfuse this area are injured, and permeability is increased, resulting in leakage of large amounts of plasma into the interstitium. This fluid lifts off the thin, damaged epidermis, causing blister formation. Despite the loss of the entire basal layer of the epidermis, a burn of this depth will heal in 7 to 21 days. Minimal scarring can be expected. Mid-dermal partial-thickness wounds commonly take 4 to 6 weeks to heal. Deep-dermal partial-thickness (second-degree) burns involve the entire epidermal layer and deeper layers of the dermis.5 These burns often result from contact with hot liquids or solids or with intense radiant energy. A deep-dermal partial-thickness burn usually is not characterized by blister formation. Only a modest plasma surface leakage occurs because of severe impairment in blood supply. The wound surface usually is red with patchy white areas that blanch with pressure. The appearance of the deep-dermal wound changes over time. Dermal necrosis and surface coagulated protein turn the wound from white to yellow (Fig. 36-6). These wounds have a prolonged healing time. They can heal spontaneously as the epidermal elements germinate and migrate until the epidermal surface is restored, or they may require a skin substitute or surgical excision and grafting for wound closure. This process of healing by epithelialization can take up to 6 weeks. Left untreated, these wounds can heal primarily with unstable epithelium, late hypertrophic scarring, and marked contracture formation.5 Partial-thickness injuries can become full-thickness injuries if they become infected, if blood supply is diminished, or if further trauma occurs to the site. The treatment of choice is surgical excision and skin grafting. A full-thickness (third-degree) burn involves destruction of all the layers of the skin down to and including the subcutaneous tissue (Fig. 36-7). The subcutaneous tissue is composed of adipose tissue, includes the hair follicles and sweat glands, and is poorly vascularized. A full-thickness burn appears pale white or charred, red or brown, and leathery. The surface of the burn may be dry, and if the skin is broken, fat may be exposed. Full-thickness burns usually are painless and insensitive to palpation. Because all of the epithelial elements are destroyed, the wound will not heal by re-epithelialization. Wound closure of small full-thickness burns (<4 centimeters squared [cm2] area) can be achieved with healing by contraction. All other full-thickness wounds require skin grafting for closure. Extensive full-thickness wounds leave the patient extremely susceptible to infections, fluid and electrolyte imbalances, alterations in thermoregulation, and metabolic disturbances. The exact depth of many burn wounds cannot be clearly defined on the first inspection, and many burn wounds may contain superficial, mid-dermal, and deep-dermal wounds. A major difficulty is distinguishing deep-dermal partial-thickness from full-thickness injury. It is important to identify the depth of injury for appropriate treatment. Deep, partial-thickness wounds that will not heal within a relatively short time are treated with wound excision and grafting. Burn wounds can evolve over time, and they require frequent reassessment. Special consideration must always be given to very young and older patients because of their thin dermal layer. Older adults may also have reduced sensation and blood supply, causing them to be more susceptible to a full-thickness injury. Burn injuries in these age groups may be more severe than they initially appear.12 The most common type of burn is a thermal burn caused by steam, scalds, contact with heat, and fire injuries. About 80% of burns in children are caused by scalds (i.e., contact with hot objects or liquids).5 Toddlers are most often affected by scalding burns. Contact burns are also common. The length of time the hot object is in contact with the skin determines the depth of injury. Flame injuries are often associated with other trauma to the patient. The highest incidence of flame injuries are more common in patients older than 6 years of age.5 Experimentation with lighters, lighter fluid, fire, firecrackers, and gasoline is more common in children age 6 to 16 years.5 Contact and flame burns tend to be deep-dermal or full-thickness injuries. Electrical and lightning injuries result in 1000 deaths per year in the United States. Electrical injuries count for 4% of burn patient admissions to burn centers.2 Low-voltage (alternating) current or high-voltage (alternating or direct) current, which is greater than 1000 volts, can cause electrical burns.4 Children have the highest incidence of electrical injury. These accidents occur as a result of insertion of an object into an outlet or by biting or sucking on an electrical cord. Pediatric electrical burns occur most often in the home, whereas in adults, electrical injuries occur in the workplace.13 Common situations that may increase the risk for electrical injuries include occupational exposure and accidents involving household current. Burns associated with radiation exposure are uncommon. Radiation burns usually are localized and indicate high radiation doses to the affected area. Radiation burns may appear identical to thermal burns.14 The major difference is the time between exposure and clinical manifestation; it can be days to weeks, depending on the level of the radiation dose. Radiation injury can occur with exposure to industrial equipment such as accelerators and cyclotrons and to equipment used for medical treatment. Location of injury can be a determining factor in differentiating the level of care required. According to triage criteria from the American College of Surgeons, burns on the face, hands, feet, genitalia, major joints, and perineum are best treated in a burn center. These burns involve functional areas of the body and often require specialized intervention (Fig. 36-8). Injuries to these areas can result in significant long-term morbidity from impaired function and altered appearance. Patient age and history are significant determinants of survival. Patients considered most at risk are those younger than 2 years and those older than 60 years. History of inhalation injury and electrical burns and all burns complicated by trauma and fractures (considered major injuries) significantly increase the risk for death. Obtaining the patient’s medical history is important, particularly a history related to cardiac, pulmonary, or kidney dysfunction; diabetes; and central nervous system (CNS) disorders. In evaluating the pediatric patient, it is essential to obtain a thorough history, especially for the nonverbal patient. Attention should be paid to the description of the burn event to rule out nonaccidental trauma (Fig. 36-9). Social services such as child protective services and the police should be consulted if abuse or neglect is suspected. According to the U.S. Department of Health and Human Services Child Maltreatment 2010 report, 3.3 million referrals were made for child maltreatment, and of those, 436,321 were investigated and substantiated for abuse.15 According to this report, 1560 children died from abuse and neglect. Child abuse or maltreatment should be a differential diagnosis when caring for children with burn injury, since greater than 15% of children suffering from maltreatment suffer from physical abuse.15 Most often burns in children are accidental but are related to failure of the caregiver or parent to provide adequate supervision. However, the developmental age and size of the child are of key importance in ruling out accidental and nonaccidental burn injuries. The patterns of burns, that is, inflicted burns consistent with immersion or dunking, can be diagnostic of child abuse regardless of history.16 The goals of acute care of the patient with thermal injuries are to save life, minimize disability, and prepare the patient for definitive care. The burn injury may involve multiple organ systems, and the approach to the injured patient should be expeditious and methodical in identifying problems and establishing priorities of care.17 The first priority of emergency burn care is to secure and protect the airway. If there is any possibility of underlying cervical instability, cervical precautions must be initiated.17 In patients with facial burns, exposure to fire in an enclosed space, or both, inhalation injury should be suspected. Carbon monoxide (CO) poisoning is associated with high mortality rates. Carboxyhemoglobin (HbCO) levels are obtained, and oxygen therapy is initiated. All patients with major burns or suspected inhalation injury are initially administered 100% oxygen.17 The nurse should continue to observe the patient for clinical manifestations of impaired oxygenation such as tachypnea, agitation, anxiety, and upper airway obstruction (e.g., hoarseness, stridor, wheezing). Early intubation may save the life of the patient who has an inhalation injury because it may be impossible to perform this procedure later, when edema has obstructed the larynx. The need for frequent blood sampling and the benefit of continuous blood pressure monitoring may necessitate placement of an arterial line. The extent and depth of the burn are assessed. The extent of TBSA of the burn is calculated for estimation of fluid resuscitation requirements (Table 36-1); the Parkland formula is the most widely used method of calculation (see Box 36-5, Case Study: Patient with Burns at the end of the chapter). Burn shock is caused by the loss of fluid from the vascular compartment into the area of injury resulting in hypovolemia. The larger the percentage of burn area, the greater is the potential for development of shock. Lactated Ringer solution is infused through a large-bore cannula in a peripheral vein. Lactated Ringer solution, an isotonic crystalloid, is the resuscitation fluid used most often. Given in large amounts, it can restore cardiac output to normal in most patients. It is preferred over normal saline because it most closely matches extracellular fluid. Because isotonic salt solutions generate no difference in osmotic pressure between plasma and the interstitial space, the entire extracellular space must be expanded to replace intravascular losses. Diuretics should not be given during the resuscitative phase of burn care. TABLE 36-1 FORMULAS FOR FLUID REPLACEMENT OR RESUCITATION IN FIRST 24 HOURS *Adjust these rates to maintain a urine output >30 mL/hr in adults or 1 mL/kg/hr in children. According to the Parkland formula (see Table 36-1), half of the calculated amount of fluid is administered to the patient in the first 8 hours after injury; 25% is given in the second 8 hours, and 25% is given in the third 8 hours. It is important to remember that calculated fluid requirements are guidelines. Fluid resuscitation is a dynamic process. The rate of fluid administration is adjusted according to the individual’s response, which is determined by monitoring urine output, heart rate, blood pressure, and level of consciousness. Meticulous attention to the patient’s intake and output is imperative to ensure that he or she is appropriately resuscitated. Under-resuscitation may result in inadequate cardiac output, leading to inadequate organ perfusion and the potential for wound conversion from a partial-thickness to full-thickness injury. Over-resuscitation may lead to moderate to severe pulmonary edema, to excessive wound edema causing a decrease in perfusion of unburned tissue in the distal portions of the extremities, or to edema inhibiting perfusion of the zone of stasis, resulting in wound conversion.11 Fluid requirements may be much higher than estimated by using the Parkland formula. The recommendations for these situations are included later in this chapter. For pediatric burn patients, add dextrose containing intravenous fluid at a maintenance rate along with Parkland resuscitation fluid. Pediatric patients need continuous dextrose infusions for vital organs. Burn injuries greater than 20% of TBSA can result in burn shock.4 Shock is defined as inadequate cellular perfusion. Significant burn injury results in hypovolemic shock and tissue trauma. Both cause the production and release of several local and systemic mediators. Burn shock can occur even when hypovolemia is corrected. Burn edema has been attributed to several factors. Barrier property changes of the capillary wall occur by direct injury and indirect mediator-modulated changes. Increases in permeability of protein and water occur, resulting in edema. In most forms of shock, capillary pressure decreases as a result of arteriolar vasoconstriction. However, after burn injury, an increase in capillary pressure has been found in burned tissue in the first minutes to hours after injury, causing capillary leak for first 24 hours.4 Coupled with this increase in capillary pressure is a negative interstitial hydrostatic pressure that occurs in the dermis layer of burned skin after thermal injury. This negative interstitial hydrostatic pressure represents an edema-generating mechanism that occurs for approximately 2 hours after injury. Plasma colloid osmotic pressure is decreased as a result of protein leakage into the extravascular space. Plasma is then further diluted with fluid resuscitation. The osmotic pressure is decreased, and further fluid extravasation can occur. In addition to leaking capillaries, local and systemic mediators cause edema and the cardiovascular problems seen in burn patients. These mediators include histamine, prostaglandins, kinins, and oxygen radicals, they increase arteriolar vasodilation.4 Manipulation of these mediators to stop the cascade of burn edema and burn shock is being researched. If fluid resuscitation is inadequate, acute kidney injury (AKI) may occur. An indwelling urinary catheter should be placed for burns greater than 15% to 20% of TBSA in the emergency department to monitor urine output and the effectiveness of fluid resuscitation. A catheter may be necessary if the burn extends into the perineal area because of the presence or development of edema. Urinary catheters with temperature probes should be used whenever possible. The nurse measures urine output hourly. Adequate urine output for adults is 0.5 to 1 milliliter per kilogram per hour (mL/kg/hr), or 30 to 50 mL/hr; in children, it is 1 mL/kg/hr.4 Patients with burns of more than 20% of TBSA are prone to gastric dilation as a result of paralytic ileus. Nasogastric or orogastric tubes are placed in these patients to prevent abdominal distention, emesis, and potential aspiration. This decrease in gastrointestinal (GI) function is caused by the effects of hypovolemia and the neurologic and endocrine response to injury. GI activity usually returns in 24 to 48 hours. Gastric prophylaxis with histamine blockers or sucralfate is initiated because burn patients are prone to Curling stress ulcers. These acute ulcerations of the duodenum are caused by sloughing of the gastric mucosa resulting from loss of plasma volume after severe burns. Enteral nutrition has been shown to be protective of gastric mucosal integrity and to improve intestinal flow, gastric motility, and intestinal blood flow in burned patients.18 Enteral nutrition should be started as soon as possible. Severely burned patients can be safely fed within 6 hours of burn injury in the duodenum or jejunum.18 Care should be taken to start enteral feeds for burn patients via nasoduodenal or nasojejunal tube promptly. Edema formation may cause neurovascular compromise to the extremities; frequent assessments are necessary to evaluate pulses, skin color, capillary refill, and sensation. Arterial circulation is at greatest risk with circumferential burns. If not corrected, reduced arterial flow causes ischemia and necrosis. The Doppler flow probe is one of the best ways to evaluate arterial pulses. An escharotomy may be required to restore arterial circulation and to allow for further swelling. The escharotomy can be performed at the bedside with a sterile field and scalpel. Care must be taken to avoid major nerves, vessels, and tendons. The incision extends through the length of the eschar, over joints, and down to the subcutaneous fat. The incision is placed laterally or medially on the extremity. If a single incision does not restore circulation, bilateral incisions are required (see Fig. 36-8). If escharotomy is required before the patient is transferred to a burn center, consultation with the receiving physician is advised. After the wounds have been assessed, topical antimicrobial therapy is not a priority during emergency care. However, the wounds must be covered with clean, dry dressings or sheets. Every attempt must be made to keep the patient warm because of the high risk of hypothermia. The administration of tetanus prophylaxis is recommended for all burns covering more than 10% of the TBSA and for patients with a questionable immunization history.10 After initial treatment and stabilization at an emergency department, referral to a burn center is considered (see Box 36-1). A burn center must be able to deliver all therapy required, including rehabilitation, and must perform personnel training and burn research.17 Patients meeting the criteria for referral need the expertise of a multidisciplinary team. Referring hospitals must always contact the burn center in their region.2 Providers in the field should cover the burns with clean, dry cloth until arrival at the burn center. Early communication between the initial provider and the burn center is encouraged by the American Burn Association (ABA).19 Inhalation injury can occur in the presence or absence of cutaneous injury. Inhalation injuries are strongly associated with burns sustained in a closed space, and they constitute the leading cause of fire-related deaths.20 Inhalation injury appears in three basic forms, alone or in combination: CO poisoning, direct heat injury, and chemical damage. The three types of inhalation injury are CO poisoning, upper airway injury, and lower airway injury. Immediate measures to save the life of the burn patient include management of the airway. The burn patient may exhibit few or no signs of airway distress; however, thermal injury to the airway must be anticipated if facial burns, singed eyebrows and nasal hair, carbon deposits in the oropharynx, and carbonaceous sputum are present or if the history suggests confinement in a burning environment. Any of these findings indicates acute inhalation injury and requires immediate and definitive care. To prevent the necessity of tracheostomy or cricothyrotomy, the use of early intubation and respiratory support must be considered before tracheal edema occurs. Inhalation injury predisposes the patient to the development of pneumonia and acute respiratory distress syndrome (ARDS).20 Management of ARDS necessitates mechanical ventilatory support and, in extreme cases, high-frequency oscillatory ventilation or extracorporeal membrane oxygenation. The occurrence of inhalation injury with cutaneous burns increases the fluid requirements during resuscitation to a higher level than would be predicted by the cutaneous burn alone. Persons found dead at the scene of a fire, who may have few or no cutaneous thermal injuries, would have died of CO poisoning. CO is a colorless, odorless, and tasteless gas. Inhalation of CO, a byproduct of the incomplete combustion of carbon, results in its bonding to available hemoglobin, producing HbCO, which effectively decreases oxygen saturation of hemoglobin. The affinity of hemoglobin molecules for CO is approximately 200 to 250 times greater than that for oxygen.9 HbCO binds poorly with oxygen, reducing the oxygen-carrying capacity of blood and causing hypoxemia. The shortage of oxygen at the tissue level is worsened by a shift to the left of the oxyhemoglobin dissociation curve, reflecting the fact that the oxygen in the hemoglobin is not readily given up to the cells. Arterial oxygen saturation measurement is of limited value because oxygen saturation may be quite high despite dangerously low levels of oxygen content. Because the pulse oximeter cannot distinguish between oxyhemoglobin and HbCO, it is an unreliable predictor of tissue oxygenation during the initial stages of CO poisoning.9 Arterial blood gas determinations and oxygen saturation are used to accurately assess the hemoglobin oxygen saturation level. A serum HbCO level is obtained the diagnosis. Normal HbCO levels are less than 2%. HbCO levels of 40% to 60% often produce unresponsiveness or obtundation; levels of 15% to 40% may result in various degrees of CNS dysfunction. Levels of 10% to 15%, which can be found in cigarette smokers, rarely produce serious symptoms but may cause a headache. The major clinical manifestations of severe CO poisoning are related to the CNS and the heart. Symptoms associated with CO poisoning include headache, dizziness, nausea, vomiting, dyspnea, and confusion.9 In severe cases, CO poisoning may lead to myocardial ischemia and CNS complications caused by lowered oxygen delivery and the already compromised circulatory system. Early signs of CO poisoning may include tachycardia, tachypnea, confusion, and lightheadedness. As the CO level rises, patients exhibit a decreased level of responsiveness, which may progress to unresponsiveness and respiratory failure. The treatment of choice for CO poisoning is high-flow oxygen administered at 100% through a tight-fitting nonrebreathing mask or endotracheal intubation. The half-life of CO in the body is 4 hours at room air (21% oxygen), 2 hours at 40% oxygen, and 40 to 60 minutes at 100% oxygen.9 The half-life of CO is 30 minutes in a hyperbaric oxygen chamber at three times atmospheric pressure. The use of hyperbaric oxygen is controversial in the care of the burn patient. Because of the rapid removal of CO with the administration of 100% oxygen, the time required to transport a patient who has received oxygen in the field should always be considered to avoid possible underestimation of inhalation injury. Heat damage may be severe enough to cause upper airway obstruction at any time, beginning from moment of injury through the resuscitation period. Caution is taken for patients with severe hypovolemia because supraglottic edema may be delayed until fluid resuscitation is under way and third spacing occurs. Patients must be monitored for hoarseness, stridor, audible airflow turbulence, and the production of carbonaceous sputum. Maximal edema occurs 24 hours after injury with upper airway injuries, and these patients should be observed in the critical care unit for a minimum of 24 hours.10
Burns
Anatomy and Functions of the Skin
Pathophysiology and Etiology of Burn Injury
Zones of Injury
Classification of Burn Injury
Size of Injury
Depth of Burn Injury



Types of Injury
Thermal Burns
Electrical Burns
Radiation Burns
Location of Injury

Patient Age and History
Child Abuse
Initial Emergency Burn Management
Airway Management
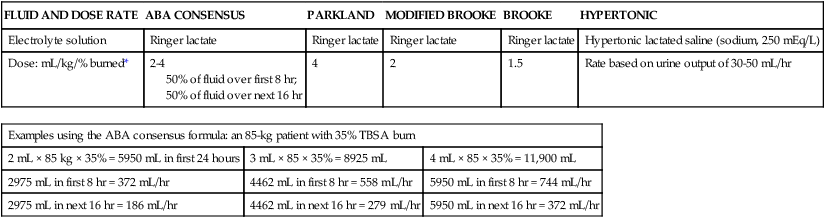
Circulatory Management
FLUID AND DOSE RATE
ABA CONSENSUS
PARKLAND
MODIFIED BROOKE
BROOKE
HYPERTONIC
Electrolyte solution
Ringer lactate
Ringer lactate
Ringer lactate
Ringer lactate
Hypertonic lactated saline (sodium, 250 mEq/L)
Dose: mL/kg/% burned*
2-4
50% of fluid over first 8 hr;
50% of fluid over next 16 hr
4
2
1.5
Rate based on urine output of 30-50 mL/hr
Examples using the ABA consensus formula: an 85-kg patient with 35% TBSA burn
2 mL × 85 kg × 35% = 5950 mL in first 24 hours
3 mL × 85 × 35% = 8925 mL
4 mL × 85 × 35% = 11,900 mL
2975 mL in first 8 hr = 372 mL/hr
4462 mL in first 8 hr = 558 mL/hr
5950 mL in first 8 hr = 744 mL/hr
2975 mL in next 16 hr = 186 mL/hr
4462 mL in next 16 hr = 279 mL/hr
5950 mL in next 16 hr = 372 mL/hr
Pathophysiology of Burn Shock
Kidney Management
Gastrointestinal System Management
Extremity Pulse Assessment
Wound Care
Burn Center Referral
Special Management Considerations
Inhalation Injury
Carbon Monoxide Poisoning
Upper Airway Injury
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access