CHAPTER 14
Breastfeeding
1 Identify the two hormones necessary for synthesis of milk and the milk ejection reflex.
2 State two subjective findings that can contribute to a poor initial feeding.
3 Demonstrate criteria for correct positioning of the infant at the breast.
4 List three objective findings that contribute to poor latching-on.
5 List four strategies to decrease breast and nipple pain related to engorgement, plugged ducts, mastitis, or all three.
6 Identify effective swallowing of infant at the breast.
7 Describe two interventions to assist a lactating mother in each of the following special circumstances: infant of a cesarean birth; reluctant or sleepy infant; irritable or fussy infant; infant with physiologic jaundice; preterm or hospitalized infant; multiple-birth infants; or special-needs infant.
8 List three strategies to increase an inadequate milk supply.
9 State nutritional needs of the lactating woman.
10 Identify which infants might benefit from supplemental lactation aids.
11 Participate as a team member in planning care for infants and mothers with special needs in collaboration with a lactation specialist or consultant, physical therapist, occupational therapist, and other health care professionals.
12 Develop a source of referrals for families with special needs.
CLINICAL PRACTICE
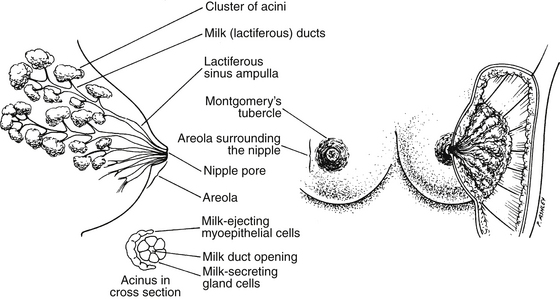
1. Hormonal influences during pregnancy begin in the first trimester related to the following (Ramsey, Kent, & Hartman, 2005):
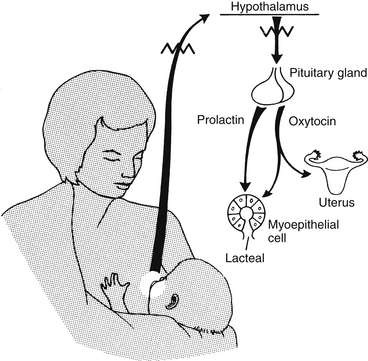
2. Initiation of milk production (Figure 14-2)
a. Prolactin level increases (at term, 200 to 400 ng/mL).
b. Estrogen and progesterone levels decrease after delivery.
c. Suckling provides continued stimulus for prolactin and oxytocin release.
d. Prolactin is released from the anterior pituitary and initiates milk production.
(1) Removal of the milk from the breast facilitates continued production of milk.
(2) Prolactin levels diminish over time in the lactating woman, but they do not return to baseline until 14 days of non-breastfeeding have occurred.
e. Oxytocin is released from the posterior pituitary and initiates milk ejection (let-down reflex); let-down reflex is triggered by the infant’s suckling at the nipple, the mother’s emotional response to the infant, or both.
(1) Colostrum is available to the infant at delivery and remains available for up to 5 days postpartum.
(3) The volume varies from 2 to 20 mL per feeding (increased volume in parous women).
(4) Higher in protein and lower in fat and sugar than mature breast milk
(1) Onset of copius milk secretion (Anderson, Moore, Hepworth, & Bergmans, 2003; Mannel, Walker, & Martens, 2008)
(2) Transitional milk: present 2 to 5 days to 2 weeks of postpartum period
(3) Mature milk: present after transitional milk; whiter and thinner than transitional milk
(a) Foremilk (a component of mature milk)
[i] Immediate milk received in feeding
[ii] Satisfies infant’s initial thirst (no normal need to supplement breastfed infant with water)
[iii] Foremilk is milk that has remained in the breast but has drawn in water and lactose and becomes more dilute.
(b) Hindmilk (a component of mature milk)
a. Previous maternal breastfeeding experience
b. Desire of mother to breastfeed and anticipated duration of breastfeeding
c. Exposure of mother to breastfeeding education
d. Cultural influences on mother
f. Previous and current maternal infections and sexually transmitted diseases
g. Any preexisting maternal health condition (such as breast surgery, thyroid dysfunction, polycystic ovary syndrome)
h. Previous and current maternal use and abuse of tobacco, alcohol, and drugs (illicit, prescription, or over-the-counter)
i. Difficult labor/delivery, cesarean section, or all
k. Preterm infant or multiple births
l. Hospitalized or special needs infant, or both
m. Infant with oral motor dysfunction
n. Infant with poor latching-on
o. Maternal complaints of pain
a. Inspect nipples for the following changes (when edge of areola is compressed at opposite sides) (Huggins, 2005):
(1) Protracted: protrude slightly at rest; when stimulated, become erect and are easy for infant to grasp
(2) Flat: may be more difficult for infant to grasp and are unchanged or retract with compression of areola
(3) Inverted: are rare; retract at rest as well as when areola is compressed
(4) Traumatized: are cracked, blistered, fissured, or bleeding; are painful when infant nurses; mother is at greater risk for breast infection (mastitis)
b. Inspect breast for the following:
(a) Augmentation: patient has the ability to breastfeed as long as milk ducts have not been severed (need to consult with surgeon about specific procedure performed; mother with poor milk production might benefit from supplemental lactation device)
(b) Reduction: variable lactation success and depends on extent of tissue removed; if nipple has been relocated, ducts usually have been severed (check with surgeon); patient might need supplemental lactation device (Marasco & West, 2005)
(c) Previous surgery for removal of cysts or lumps: incisions that could disrupt milk ducts
(d) Single mastectomy: infant can feed from remaining breast
(2) Size and condition of breast
(a) Asymmetry of breasts is not uncommon; severe difference in size might indicate reduced milk glands in smaller breast.
(b) Size of breast not related to ability to produce milk
[i] Might go into remission during lactation
[ii] Might improve with decrease in caffeine intake
[iii] Hand expression of milk might be uncomfortable in fibrocystic breasts, but mechanical pumping is effective.
[i] Breasts are tender, swollen, firm, and warm to the touch.
[ii] Mother might have fever; indicator of inadequate removal of milk from the breast
[iii] Typically occurs 2 to 4 days postpartum
[iv] Hand or mechanical expression for a few minutes prior to latch-on will soften the areola and improve latch-on
[v] Frequent breastfeeding and ice packs might alleviate condition.
[vi] Prevention is achieved with frequent, effective breastfeeding.
(e) Plugged duct: blocked milk duct; might have palpable lump and localized tenderness, swelling, and redness in area; warm compresses or shower before frequent breastfeeding might help alleviate condition
(f) Breast infection or mastitis
[i] Might be associated with milk stasis and unresolved plugged duct, cracked nipple, or both
[ii] Mother might have more severe symptoms similar to those of influenza (fever, chills, joint pain, and headache).
[iii] Stress and fatigue of the mother may increase suceptibility.
[iv] Usually only one breast with localized redness is involved.
[v] Heat to the breast before frequent feedings, pumping following feedings, and rest for the mother may alleviate condition.
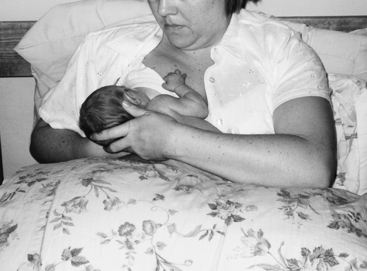
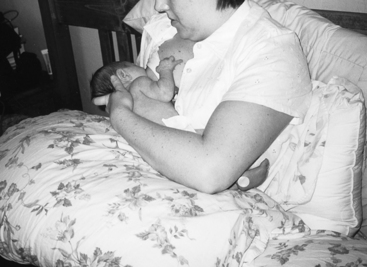
c. Observe maternal positioning of infant; four positions are possible.
a. Mother needs to be in a relaxed position as she supports her infant.
(1) Infant must grasp the breast behind the nipple and keep the nipple drawn to the back of the mouth
(2) Combination of proper positioning of infant, correct hand position on breast, and correct latching-on prevents or decreases incidence of sore nipples.
(3) When choosing a position for breastfeeding, first ensure that mother is comfortable and well supported.
(4) Pillows can be used to further suppport the mother’s arm.
(a) Cradle-hold position (Figures 14-3 and 14-4)
[i] Infant’s head is held in the crook of mother’s elbow (lower ear positioned on the bend of mother’s elbow).
[ii] Infant and mother should be tummy to tummy with infant’s bottom shoulder tucked in slightly closer to the mother’s stomach than the top shoulder.
[iii] Grasp infant’s bottom with hand, and tuck infant’s lower arm next to mother’s stomach.
[iv] Support breast with opposite hand, fingers behind areola, index finger under breast; lift up under breast until nipple is directly in front of infant’s mouth; continue to support breast during the early weeks of feeding (Figure 14-5).
[v] Bring infant to breast with pressure at the infant’s upper back; do not push breast into infant; infant’s chin should be positioned first and deepest into the breast.
(b) Cross-cradle hold offers the mother more control over the infant’s head position (Figures 14-6 and 14-7).
[i] Place infant across mother’s stomach similar to the cradle hold described previously.
[ii] Hold the infant with the opposite hand, placing mother’s hand at the infant’s upper back, supporting the back of his or her neck.
[iii] The infant’s body is held close to mother by tucking her forearm around the infant’s bottom and pulling the infant close.
[iv] The hand that is supporting the breast is positioned in a “V” shape with the thumb and index finger coming up from the bottom of the breast; the nipple should gently tip toward the infant’s mouth (Figure 14-8).
[v] Once the infant has a wide, open mouth, he or she can be brought on to the breast by pressure at the infant’s upper back. The infant’s chin should be posititioned first and deepest into the breast, resting well behind the nipple.
(c) Football-hold or clutch position offers good control of infant and may be helpful after cesarean birth or with a premature infant (Figure 14-9).
[i] Place infant on pillow at mother’s side.
[ii] Have mother support infant’s upper back with arm and support infant’s neck in hand.
[iii] Have infant’s head level with the breast.
[iv] Have mother use opposite hand to support breast, fingers off areola with index finger under breast; palm should remain facing the mother’s rib cage; nipple should gently tip down toward infant’s mouth (Figure 14-10).
(d) Side-lying position (Figure 14-11)
2. Latching-on problems due to flat or inverted nipples, nipple confusion, or both
a. Correct placement of the infant’s mouth behind the nipple ensures good stimulation for milk supply, promotes good milk transfer to the infant, and decreases or prevents sore nipples.
(1) Have mother stroke (from superior to inferior in direction) the center of the infant’s lip with nipple.
(2) Allow mouth to open wide, and center breast in mouth.
(3) Have mother pull infant in close (pull infant in with pressure on infant’s upper back or neck), place lower gum well behind nipple with lips flanged; chin is positioned deep into breast.
(4) Mother can remove infant from breast by breaking the suction: insert a clean finger gently into the corner of infant’s mouth, between infant’s gums.
(1) Infant’s mouth is opened wide; lips are not tucked or curled.
(2) Infant’s gums are placed behind nipple on areola.
(3) Tongue is positioned under breast.
(4) Infant demonstrates burst of suckling.
(5) Few or no complaints of sore nipples occur.
c. Interventions for flat or inverted nipples
(1) Have patient obtain prenatal breastfeeding education on correct latch-on techniques.
(2) Have patient place her thumbs on either side of the areola and gently stretch the areola (Hoffman’s exercise); thumbs should be rotated around edge of areola to stretch all areas; Hoffman’s exercise can be performed several times per day (Amarasena, 2006).
(3) Have mother apply ice to nipple a few minutes before feeding to increase nipple erection.
(4) Have mother use breast pump for a few minutes before latch-on to increase nipple protrusion.
(5) Silicone nipple shields can be used to assist in feeding only if all other interventions have failed and the mother has a good milk supply.
(a) The mother must be followed closely (best if by a lactation specialist) to ensure that the infant is getting adequate nutrition (Meier et al, 2000).
(b) A mother who is using a nipple shield may need to pump in addition to breastfeeding to compensate for the reduced stimulation to the breast that occurs when using a nipple shield until her milk supply is well established and infant has demonstrated the ability to transfer adequate amounts of milk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree