Breast Cancer
Invasive Breast Cancer
DEFINITION
Invasive breast cancer, also referred to as infiltrating breast cancer, has spread beyond the basement membrane of the duct or lobule of the breast and into the surrounding tissue. The diagnosis of invasive breast cancer is considered to be systemic, not localized, because of its ability to spread through the vascular system. The breast includes the following specific anatomical areas:
ETIOLOGY AND RISK FACTORS
SIGNS AND SYMPTOMS
• Pain is uncommon in early disease
• Changes in the size or shape of the breast
• Pink or bloody spontaneous unilateral nipple discharge may occur
• Skin changes—dimpling, edema, erythema, ulceration
• Nipple changes—inversion, scaling, ulceration
• Symptoms of metastases (i.e., shortness of breath), cough. Loss of appetite, abnormal liver function tests, headaches, and many others
DIAGNOSTIC WORKUP
Diagnostic mammogram for early detection of breast lesions:
• Workup may include ultrasonography, positron emission tomographic scan, or magnetic resonance imaging of the breast.
• Clinical breast examination to include bilateral breasts, axilla, and supraclavicular and infraclavicular areas
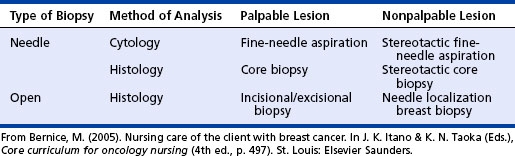
• Biopsy for a pathological diagnosis (see table on page 36)
• Imaging studies may include bone scan, computed tomographic scan of the chest and abdomen or others depending on the presenting signs and symptoms to rule out metastases
• Laboratory tests to include hematological chemistry evaluations and tests for tumor markers CA15-3 and CA27.29
HISTOLOGY
Breast cancer is a heterogeneous disease with 24 distinct histological subtypes. Some of the more common subtypes of breast cancer are the following:
• Invasive ductal carcinoma—70% to 80% of all breast cancers
• Invasive lobular carcinoma—10% to 15% of all breast cancers
• Medullary carcinomas—5% to 7% of malignant breast tumors
• Other less common subtypes include tubular, mucinous, sarcomas, and papillary carcinomas
• Axillary lymph node status—prognosis worsens with increased involvement
• Tumor size—increased risk of recurrence with increasing size
• Hormone receptor status—estrogen receptor (ER)– and progesterone receptor (PR)–negative tumors are associated with a worse prognosis
• Deoxyribonucleic acid (DNA) ploidy—aneuploid tumors, those with an abnormal amount of DNA have a poorer prognosis
• High S-phase fraction predicts poorer outcome
• Histopathological considerations take into account the nuclear pattern, morphologic features, and mitotic activity. The higher the grade the worse the prognosis
• Molecular and biological factors that may be associated with a poor prognosis include the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree