6 Beginning the learning experience
Preparing for the placement
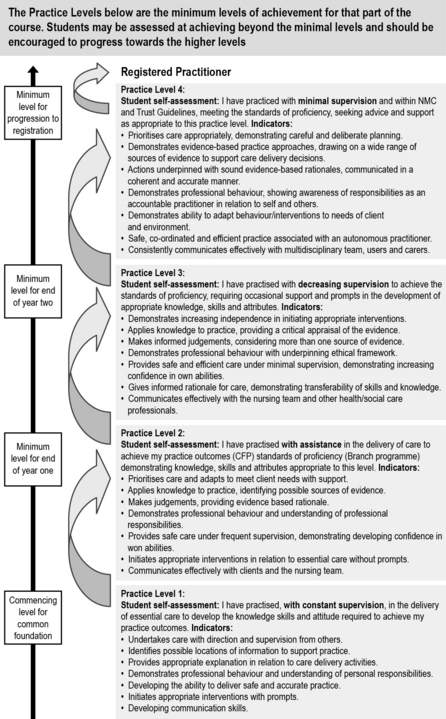
Although all student nurses are required to meet the NMC standards for pre-registration nursing education (NMC 2010) before progressing to registration, each university has a different method of assessing the level of competency. Benner’s (1984)From Novice to Expert and Bondy’s (1983) ‘skills escalator’ are examples of commonly used assessment strategies. Other universities may have an ‘achieved’ or ‘not achieved’ system. The NMC stipulated that this is not a sufficiently robust method and all pre-registration nursing providers will be expected to introduce a rigorous clinical assessment strategy, in which to measure the NMC Competencies.
Bondy (1983) (Fig. 6.1) uses four levels of achievement, and as students progress through their placements, they have minimum levels to achieve from 1–4. They can, however, meet a higher level in some outcomes or competencies if their mentor assesses they are working at that level. In each placement, they must meet the minimum level or the outcome/competency is not achieved. The levels are indicated in the ongoing achievement record on the corresponding ‘assessment results’ sheet for that semester. The level achieved for each outcome/competency should be recorded rather than merely a tick in the box.
Planning and preparation are competencies in their own rights and, as well as being essential to starting any new placement, learning these organisational and prioritising skills will be worthwhile throughout your training and in your professional role as a registered nurse. Levett-Jones and Bourgeois (2007) offer excellent advice and guidance for students prior to, during and after placements.
Roberts (2010) outlines key things you can do to prepare before starting a clinical placement. These include making sure you attend your planned clinical skills and simulated learning sessions and also, if an opportunity is planned into the timetable, undertaking some additional practice in the clinical skills classroom, either on your own or with a colleague (make sure your skills tutors are aware that you are doing so).
A good example is the online clinical skills resource written by Docherty and McCallum (2009), available at:
http://www.oup.com/uk/orc/bin/9780199534456/01student/checklists/(accessed May 2011)
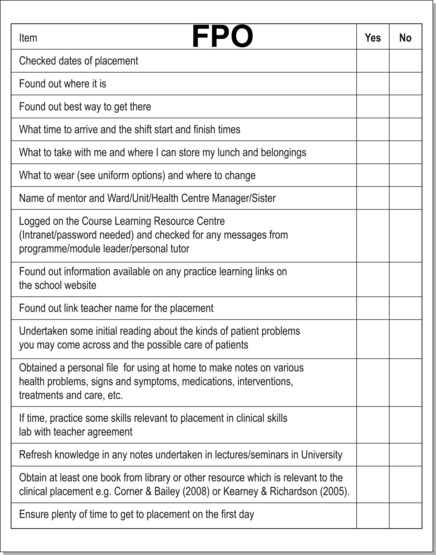
A good way to dispel your fears is to make contact with your placement area. Many universities have placement details on the internal Web pages and this can be a good starting point for finding out about the area. Phone or e-mail the placement and arrange to speak with your mentor. You may use the placement checklist in Figure 6.2 to remind you of things to find out or do before starting your placement.
An induction may include the following:
• Introduction to the placement and overview of the services offered.
• Chemotherapy and radiotherapy overview and safety features.
• Understanding spiritual distress in patients and the impact on the professional team.
• Opportunity to meet members of the wider multidisciplinary team, for example the chaplain and practice placement staff.
• Opportunity to explore areas of concern and personal feelings of anxiety.
What to expect in the first week
Within the first week
• Ward routines: visiting times; rest hour; protected meal times arrangements; meal times.
• What learning resources are available in the area: access to specialist resources; can resources be borrowed?
• Multidisciplinary team members in the clinical area: list their names and roles.
• Infection control policies: are flowers allowed in the area? What are the handwashing/rub facilities for visitors?
Mapping your own learning needs to NMC competencies
You will probably be undertaking either a programme of study where the course is clearly divided into a 1-year common foundation programme (CFP) and a 2-year branch programme, or one where there is no CFP and branch evident but still requires a programme of study which enables you to achieve outcomes (NMC 2010) which are field specific (adult, child, mental health and learning disability nursing).
Regardless of which NMC outcomes you are having to achieve on this placement, the principles remain the same. You must adhere to both the Guidance on Professional Conduct (NMC 2009) and The Code: Standards of Conduct, Performance and Ethics for Nurses and Midwives (NMC 2008). It is very important that you read these and discuss them with your personal tutor before undertaking placement learning and also your mentor when you meet for the first time.
Learning about the team
As well as being supported by a named mentor, there will be a number of other qualified nurses (now known as registrants) and other healthcare workers and professionals who will help facilitate your learning and will contribute to assessing your knowledge and skills while on placement. It is important for you to consider the specific roles and responsibilities of these individuals. This is covered in Chapter 7.
Key roles linked to student learning in practice
The mentor
Every student who is allocated by their university to gain a clinical placement learning experience has to have a named mentor who will be their main facilitator of learning, supervisor and assessor of their practice (mandatory requirement of the NMC 2008). All mentors should be experienced nurses who will have completed a course of mentorship preparation or have an equivalent qualification in their own field which is recognised as being appropriate to supervise and assess student nurses in practice (this latter individual will only be able to undertake the mentor role in specific placements and not at the major progression points within the new NMC (2010) guidance for curriculum delivery). Your mentor will be responsible for assessing your learning and competence in practice and your practice assessment document, as well as completing and signing your ongoing record of achievement (ORA) (Box 6.1), sometimes known as ongoing achievement record (OAR) (NMC 2007).
Box 6.1 Roles and expectations of you as the student and your mentor in relation to the assessment (ongoing record of achievement (ORA))*
The assessment process
Week 1
1. Student MUST negotiate with their mentor a time for their initial interview to discuss learning needs and goals and agree an action plan for achievement.
2. Student MUST share with their mentors their ORA from any previous placements and any action plans resulting from their last assessment of learning in practice.
3. Student will ensure that mentors are aware of any non-practice assessments they need to complete which may require their support for achieving, such as a client-focused assessment or evidence-based practice on a placement-specific topic.
4. Student may also have additional practice-based assessments to achieve in the placement, such as medicine management, handwashing skills or (ward/patient care) management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree