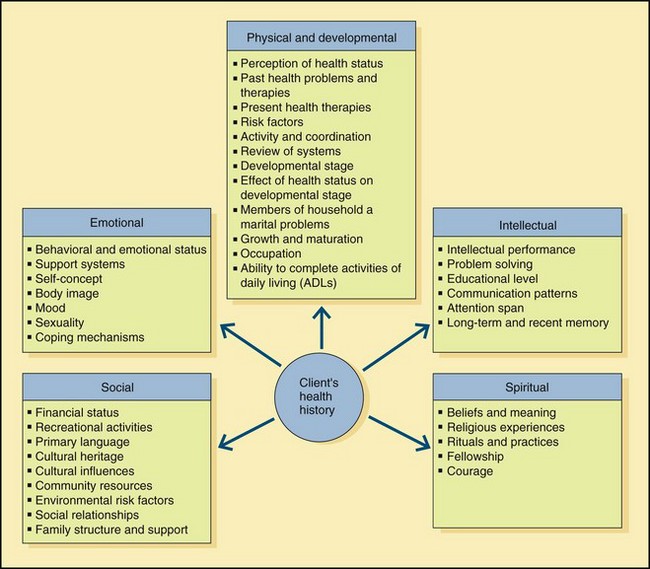
Chapter 2 1. Types of data: objective (overt, measurable, detected by physical assessment); subjective (covert, feelings, sensations, and symptoms verbalized by client) 2. Sources of data: client (primary); family/friends, health care team members, clinical record and other documents, textbooks (secondary) 3. Methods of data collection: interviewing, observation of nonverbal cues, congruency between verbal and nonverbal data, physical assessment (e.g., observation, palpation, auscultation, percussion) (Figure 2-1: Dimensions for gathering data for a health history) 4. Management of data: screening, organizing, and grouping/clustering significant defining characteristics and related information 5. Identification of client’s problem, concerns, or deficits that can be altered by nursing interventions a. Outcomes are expected changes in client’s behavior, activity, or physical state b. Outcomes must be objective, achievable, and measurable, and include a realistic period for accomplishment to determine whether outcome has been achieved 2. Collaborate with client, family/significant others, and appropriate health care team members to formulate a plan to reach identified outcomes; preparation for discharge begins at admission 3. Establish priorities of care using Maslow’s Hierarchy of Needs (see Figure 1-1) 1. TJC National Patient Safety Goals (e.g., increasing accuracy of client identification, improving effectiveness of communication among members of health team, reducing risk of health care–associated infections and falls, improving safety of medication administration) 2. TJC standardized performance measures (e.g., core measures) to determine compliance with standards of care 3. Evidence-based practice (EBP) involves using research findings, experience, or client values to guide clinical decision making a. Nurses must evaluate and participate in research that improves quality of nursing care b. Levels of evidence refer to strength of support for a particular nursing strategy; levels of support range from systematic review of all relevant randomized controlled trials (RCTs) to reports of a committee of experts 4. Identification of sentinel events A Need to communicate is universal B Through communication, humans maintain contact with reality, validate findings with others to interpret reality, and develop a concept of self in relation to others C Validation is enhanced when communication conveys an understanding of feelings D Communication is learned through the process of acculturation E Communication is the avenue used to make needs known and to satisfy needs A Requires: sender, message, receiver, and response 1. Verbal: related to anything associated with spoken word; includes speaking, writing, use of language or symbols, and arrangements of words or phrases; hearing is essential to development of effective speech because one learns to form words by hearing words of others; includes pace, intonation, simplicity, clarity, brevity, timing, relevance, adaptability, credibility, and humor 2. Nonverbal: related to messages sent and received without use of words and is expressed through appearance, body motions, use of space, nonverbal sounds, personal appearance, posture, gait, facial expression, gestures, and eye contact; more accurately conveys feelings because behavior is less consciously controlled than verbal communication 3. Confusion arises when there is a difference between verbal and nonverbal message received (lack of congruence in overt and covert messages) C Themes of communication: recurring thoughts and ideas that give insight into what client is feeling and that tie communication together 1. Content: conversation may appear superficial, but attention to underlying theme helps nurse identify problem areas while providing insight into client’s self-concept 2. Mood: emotion or affect that client communicates to nurse; includes personal appearance, facial expressions, and gestures that reflect client’s mood and feelings 3. Interaction: how client reacts or interacts with nurse; includes how client relates and what role is assumed when communicating with nurse and others D Factors affecting communication process: language, psychosociocultural influences, intellectual development, gender, values and perceptions, personal space (intimate, personal, social, and public), territoriality, roles and relationships, environment, congruence of verbal and nonverbal messages, and interpersonal attitudes 1. Variation in culture, language, and education 2. Problems in hearing, speech, or comprehension (ineffective reception or perception) 3. Refusal to listen to another point of view 4. Use of selective inattention; may cause an interruption or distortion of messages 5. Environmental considerations (e.g., noise, lack of privacy, room temperature) 6. Psychologic or physiologic discomfort (e.g., anxiety, hunger, pain) A Phases in a therapeutic relationship 1. Preinteraction: begins before nurse’s initial contact with client a. Self-exploration involves acknowledging one’s own feelings, fears, personal values, and attitudes, including identification of misconceptions and prejudices that are socially learned b. Self-awareness is necessary before establishing a relationship with others c. Tasks include gathering data about client and planning for first interaction with client 2. Orientation or introductory: the nurse, who initially is in the role of stranger, establishes a trusting relationship with the client by consistency in communication and actions; clients should never be pushed to discuss areas of concern that are upsetting to them a. Introduction of nurse, explanation of nurse’s role in multidisciplinary team, and purpose of interaction b. Contract outlining mutually agreed upon goals is set c. Confidentiality issues are discussed, and client rights are upheld d. Termination begins during orientation phase by establishing time parameters 3. Working: nurse and client discuss areas of concern, and client is helped to plan, implement, and evaluate a course of action a. Transference and countertransference may become an issue (see Chapter 16, Therapeutic Nurse-Client Relationship, Overview) b. Anxiety levels may increase; acting-out behaviors can and do occur; resistance to change need to be anticipated, identified, and addressed c. Problems need to be discussed and resolved 4. Termination: end of therapeutic relationship between nurse and client; spacing meetings further apart near end facilitates termination a. Goals and objectives achieved are summarized b. Positive adaptive behaviors are reinforced c. Feelings and experiences for both client and nurse are shared d. Rejection, anger, regression, or other negative behaviors may be expressed as a means of coping with the impending termination of the relationship B Considerations fundamental to a therapeutic relationship 1. Client is unique and worthy of respect 2. Client needs to feel accepted a. Acceptance is an active process designed to convey respect for another through empathetic understanding b. Acceptance of others implies and requires acceptance of self c. Nurse’s identification of own attitudes and feelings and their effect on perception is necessary before developing a nonjudgmental attitude d. Acceptance requires that clients be permitted and even encouraged to express feelings and attitudes even though they may be divergent from a general viewpoint; setting limits might be required for inappropriate behavior in a manner that does not reject client 3. The high stress/anxiety of most health settings is created in part by the health problem itself; treatments and procedures; nontherapeutic behavior of personnel; strange environment; inability to use usual coping skills (e.g., exercise, talking with friends); and change in lifestyle, body image, and/or self-concept 4. Previous patterns of behavior may become inadequate under stress: health problems may produce change in family or community 5. Health problems may produce change in self-perception and role identity 6. All behavior has meaning and usually results from an attempt to cope with stress or anxiety 7. Value systems influence behavior 8. Cultural differences exist among people; one’s own culture is an integral part of an individual 9. Personal meaning of experiences to clients is important 10. Clients have potential for growth a. Clients need to learn about their own behaviors b. Exchanging experiences with others provides a new learning environment and reassurance that reactions are valid and feelings are shared c. Participating in groups increases knowledge of interpersonal relationships and helps individuals to identify strengths and resources d. Identifying client’s strengths and resources emphasizes positive attributes which form a basis for future growth 11. Behavioral changes are possible only when client has other defenses to maintain equilibrium 12. Providing information may not alter client’s behavior 13. Use of defense mechanisms needs to be identified 14. Maintaining confidentiality supports a trusting relationship 15. Use of therapeutic interviewing techniques communicates acceptance and supports expression of feelings C Support of therapeutic communication 1. Maintenance of a nonjudgmental environment 2. Implementation of actions that support dignity and worth a. Maintaining eye contact when communicating b. Using names rather than labels such as room numbers or diagnoses; approach client as a person with difficulties, not as a “difficult person” d. Maintaining confidentiality e. Being courteous toward client, family, visitors, and members of the health team f. Permitting personal possessions when practical g. Providing explanations at client’s level of understanding 3. Encouragement of participation in problem solving and decision making 5. Fostering trust through honesty, consistency, reliability, and competence D Use of therapeutic techniques to facilitate communication 1. Reflection of feelings, attitudes, and words: helps client to identify feelings 2. Open-ended questions: permit client to focus on issues 3. Paraphrasing: rephrasing of feeling or thought in similar words to convey that message was understood or to provide an opportunity for clarification if necessary 4. Silence: provides nurse and client with necessary time for reflecting about what is being discussed and allows time to formulate a response 5. Touch: conveys caring, but its effectiveness can vary among individuals and cultures 6. Clarification: helps to ensure that message is understood as intended 7. Direct questions: facilitate collection of objective data but may block expression of feelings E Avoidance of nontherapeutic communication 1. Any overt/covert response conveys a judgmental (approval or disapproval) or superior attitude 2. Direct personal questions are probing or invasive 3. Ridicule conveys a hostile attitude 4. Talking about one’s own problems and not listening convey a self-serving attitude and loss of interest in the client 5. Stereotyping devalues uniqueness of the client 6. Changing the subject conveys a lack of interest in the client’s concerns 7. False reassurance eventually results in lack of trust 8. Minimizing concerns is demeaning 9. Asking for explanations using the word “why” may put client on the defensive 10. Using clichés minimizes concerns 11. Using terms of endearment such as “honey” is demeaning 12. Defensive responses shut off communication 13. Giving advice interferes with the client’s ability to problem solve 14. Challenging client to defend a position/feeling may put client on the defensive
Basics of Nursing Practice
Nursing Process
Ensuring Quality Health Care
Communication
Basic Concepts
Communication Process
The Nurse-Client Relationship
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basics of Nursing Practice
Get Clinical Tree app for offline access