3. Basics of musculoskeletal injury and examination
Contents
Terminology23
The musculoskeletal system and healing27
Treatment of acute injury29
Bone35
Soft connective tissues41
Basic principles of examination54
The purpose of this book is to equip you with the tools which you will need to make a safe, competent diagnosis of an injured patient. It can be difficult to assess patients with closed limb injuries, the largest part of minor injury work, or with musculoskeletal pain and no history of injury. There is no direct access to the injured part, and the patient’s description of the problem may not tell you which tissue is causing the difficulty.
Musculoskeletal problems show themselves by two signs, pain and a loss of normal function in the affected part. There are not usually, with exceptions of which infection is the most common, any systemic signs of illness and the patient will describe his or her symptoms to you in a similar way regardless of which tissues are damaged. Compare that to the clinical situation when a patient presents with a heart attack. There may be a complaint of pain radiating into the left arm, but you are not likely to linger long with the idea that your patient has a bit of a sprain. A common reason for an injured person coming to hospital is that he or she thinks that the injury is a fracture, and we often find that this is not the case. However, we will frequently have requested an X-ray to decide the matter because the history and the examination did not.
It often does not matter which of the musculoskeletal tissues are injured, and it is common to see the non-specific diagnosis ‘soft tissue injury’ in the notes. If an injury is not severe and the management is the same regardless of which tissue is damaged, then there is no reason to pursue the matter. There are also cases where it is clear which tissue is damaged, and little examination is required to reach a diagnosis. This often happens with more severe injuries such as displaced fractures and large dislocations. There remain, however, patients who present with problems which require a much closer assessment and where an exact diagnosis has a direct bearing on the way that the injury is managed and on the outcome.
A robust and simple method of examination and diagnosis will be described in this chapter, together with the rationale for that approach. The aim is to provide the tools for the first assessment of an undiagnosed patient. The suggested methods are straightforward and, once learned, rapid. The detail of how to apply these ideas to the examination of individual parts is shown in the two chapters which follow.
Before going on to discuss examination, essential information about the language of examination, the anatomy of the musculoskeletal system and the management of acute injuries will be covered.
Terminology
The language of anatomy is used when writing patient records and making referrals. Some general terms are defined in this part. Additional new terms are introduced in bold type at the relevant parts of the text.
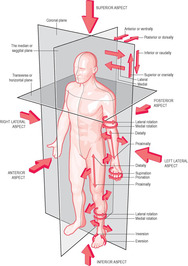
Anatomical position. Carry this image in your head and base your notes upon it (Figure 3.1). Any health professional who reads them will assume that you have that position in mind when you describe an injury. The anatomical position looks oddly hieratic, but the figure is standing in a conventional, symmetrical, neutral position except for a single detail, which is that the palms of the hands have been turned forwards in the supine position. The hands are in that position so that the radius and ulna are ‘uncrossed’, with the radius on the outer side of the arm at both elbow and wrist, and the ulna on the inner side.
 |
| Figure 3.1 • (Adapted from Standring 2008, with permission.) |
Right and left. Always means the patient’s right and left, not the examiner’s.
Axis and plane (Figure 3.1). An axis is an imagined line (which sometimes corresponds to the line of a real structure) around which movement happens. A plane is a flat surface. The idea of the body divided by imaginary planes is useful for describing the direction and angle of movement. Three basic planes are described, each at right angles to the others. A sagittal plane is vertical, passes from front to back and divides the body into left and right parts. A sagittal axis is a horizontal line passing from front to back on a sagittal plane. Movement about this axis (e.g. abduction and adduction of the hip) happens on a coronal plane. It may help to think of the sagittal axis around which the hip abducts as a bolt through the joint, passing from front to back and allowing free swinging movement from side to side. A coronal plane (also called frontal) is vertical, passes from side to side and divides the body into front and back parts. A coronal axis is a horizontal line passing from side to side on a coronal plane. Movement about this axis (e.g. flexion and extension of the hip) happens on a sagittal plane. A transverse plane is horizontal and divides the body into upper and lower parts. A longitudinal axis is a vertical line about which certain movements (e.g. lateral rotation of the shoulder) occur on a transverse plane.
Anterior (ventral) means to the front and posterior (dorsal) to the back.
Superior (or cranial, ‘towards the head’) means above and inferior (or caudal, ‘towards the tail’) means below.
Lateral means away from and medial means closer to the midline of the body.
Proximal means closer to and distal further from the origin of a limb or other structure (e.g. the elbow is proximal to the wrist, and the wrist is distal to the elbow, both in relation to the origin of the arm, which is the shoulder).
Flexion is movement at a joint which reduces the angle between bones on a sagittal plane. Extension is the opposite movement at the same joint (e.g. the elbow flexes to bring the hand nearer to the shoulder and extends to bring upper arm and forearm into a straight line). The position from which flexion begins varies from joint to joint. The elbow lies in full extension and flexion starts from that position, but the head and neck are usually held in a position mid way between flexion and extension. Note that flexion occurs in an anterior direction at the elbow and in a posterior direction at the knee, but both movements occur on the same plane. Flexion in the upper part of the body is related to purposeful coordination of hand and eye and always occurs in the anterior direction. The muscles of flexion are stronger than those of extension. Extension is a junior assistant to flexion. In the lower part of the body, the functional emphasis is on weight bearing, and the key relationship is with the pelvis and the spine. The spine is designed in a series of alternating curves in order to absorb the forces generated by walking. The legs continue that principle and, in comparison with the arms which they structurally resemble, they are rotated in a posterior direction. This explains why flexion is anterior at the hip but in a posterior direction at the knee.
Special terms are used for flexion and extension at the ankle (Figure 3.2). The foot joins the leg like the crosspiece on an upturned letter T. The angle between foot and leg is reduced and increased by movement in either direction, and it has been deemed that this makes a distinction between flexion and extension difficult. Therefore, movement of the foot towards the shin is dorsiflexion (Figure 3.2B) and pointing the toes down is plantar flexion (the sole of the foot is called plantar and the surface which we can see when we look down is the dorsum).
 |
 |
 |
 |
| Figure 3.2 • |
Abduction is movement away from the midline of the body on a coronal plane, for example at the shoulder when the arm is lifted away from the side (Figure 3.3). In the hand, abduction is movement of the fingers away from the midline of the middle finger. In the foot, the toes abduct from the midline of the second toe. Adduction is movement towards the midline, the reverse of abduction. Certain movements on the coronal plane cross the midline and combine abduction and adduction; consequently, these words are not useful. Movement to the side at the cervical and lumbar spine is lateral flexion, or side flexion, to right or left. Side-to-side movement of the hand at the wrist is called deviation, and its directions are named for the forearm bone that the hand moves towards, ulnar and radial. In other words, movement of the hand, at the wrist, towards the little finger is ulnar deviation and towards the thumb is radial deviation. Abduction is a term which causes confusion at the thumb. Movement of the whole thumb away from the hand in a palmar direction is palmar abduction, and movement of the whole thumb to the radial side is radial abduction. Movements of the thumb at its two internal joints are flexion and extension. These and other movements of the thumb are discussed in Chapter 4.
 |
| Figure 3.3 • |
Circumduction is a fluent sequence of four movements, flexion, abduction, extension and adduction, at one joint, to make a single circular movement. Hip, shoulder, wrist and base of thumb are all capable of circumduction.
Rotation is movement of a bone around a longitudinal axis (e.g. at the neck, shoulder and hip); towards the midline of the body is medial or internal rotation and away from the midline is lateral or external rotation. At the neck and waist, where the rotating part is in the midline, rotation can not be described as medial or lateral, and as with side flexion, it is named right or left.
Supine means facing upwards (or forwards in the anatomical position) and prone face down or backwards. Supination of the hand is movement to the palm-up position by lateral rotation of the forearm. Pronation of the hand means turning the palm down by movement of the forearm. (Note that the hand can also be rotated by shoulder movement when the elbow is extended, something which a patient may try to do if forearm movement is reduced. It is therefore best to examine forearm movement with the elbow flexed.) Supination of the foot means raising its medial edge, a movement more commonly called inversion (Figure 3.2C). Similarly, pronation of the foot, lifting its lateral edge, is usually called eversion (Figure 3.2D). (This is a simplification. Foot and ankle movements are complex, multi-joint combinations.)
Valgus and varus describe the direction of a body part or a movement in a coronal plane from a given point where that direction changes. The words are often used to describe angulated deformities in bones or around joints. They always refer to the direction of the distal part of the deformity. Valgus means angulation away from the midline of the body (e.g. knock knees). Hallux valgus, the condition commonly known as bunion refers to the abnormal lateral direction of the big toe (hallux) from the metatarsal phalangeal joint. If someone’s knee is struck on the lateral side so that the ligament on the medial side is stretched, this can be described as a valgus stress to the knee. Varus means an angulation towards the midline (e.g. bow legs).
The musculoskeletal system and healing
This part introduces musculoskeletal anatomy and contains general information on the healing process and the principles of treatment of injuries. This is followed by a survey of anatomy, types of injury and healing and treatment of each of the tissues of the musculoskeletal system. Particular injuries are described at the appropriate places in Chapters 4 and 5.
The musculoskeletal system
The musculoskeletal system is a frame made of segments of hard connective tissue, bone, held together by various softer connective tissues (skeletal muscle, tendons, cartilage, ligaments, synovium, bursa and fascia). Connective tissue is characterised by large amounts of extracellular material, mainly the proteins collagen and elastin, which give it strength and resilience. The frame is moved, at its joints, by the contractile skeletal muscles. The functions of the musculoskeletal system are protection of the organs, movement and stability.
Movement and stability are conflicting priorities. Stability is easily attained by lying down and doing nothing. In our waking lives we stand erect, we move around, we reach out with our hands, we give up absolute stability so that we can interact with the world around us. Stability becomes relative and dynamic, subordinate to movement but an indispensable partner with it. Our stability may be challenged by the forces which we meet in the world beyond our bodies. Internally, the forces generated by our own muscles and the alterations caused by our slightest movements require an endless stream of stabilising adjustments.
The structure of different parts of the musculoskeletal system, and the problems to which they are prone, reflect, in part, this trade-off between movement and stability. The shoulder is highly mobile but prone to dislocation. The knee will accept heavy loads but can be injured by slight abnormal movements.
Severity of injury
Various labels are used for the severity of soft tissue injuries, and certain aspects of description are peculiar to individual tissues. There is a general tendency to assign injuries, especially tears to ligament or muscle, which make up the bulk of acute soft tissue injuries, to one of three categories. These may be called grades 1, 2 and 3, or minor, moderate and severe (Box 3.1).
Box 3.1
Degrees of severity – two variables, pain and disability (muscle disability = weakness, ligament disability = laxity)
• pain with no disability = grade 1 = patient home with advice
• pain and disability = grade 2 = physiotherapy
• disability with no pain = grade 3 = orthopaedic review
In the minor clinic, these distinctions are made by assessing the severity of the mechanism of injury, the appearance of the injury, and the pain and disability it has caused. You can use this grading system for three purposes: to clarify your thinking about the severity of an injury by assessing it in line with simple criteria, pain and disability; to document the injury in a way that is common to other professionals; and to support your chosen management decisions. You use the two variables to give you a simple, useful documentation which incorporates the broad outline of your plan of management.
Grade 1
A grade 1 injury will typically damage only a small number of fibres, perhaps 5% in the case of a muscle (although this figure is meaningless in the clinical setting, where only examination findings are useful). It will cause pain when the part is used or stressed, and perhaps some visible swelling and bruising, but the patient will not be disabled and recovery should be relatively swift, with marked improvement in one to two weeks, and uncomplicated. Severe signs such as deformity, heavy bruising, the inability to walk will be absent. You will discharge the patient with clear advice on the care of the injury, and advice to seek further help if it is not improving.
Grade 2
A grade 2 injury is caused by a more severe mechanism and there will be a larger number of damaged fibres. The bleeding and the disability is greater; there may be some abnormal laxity in the case of a ligament injury or pain and weakness in the case of an injured muscle. There will not be a complete division of the whole structure (if there is doubt about this, treat the patient as having a grade 3 injury). This injury will take weeks or months to heal, and will be prone to the complications of soft tissue healing which are discussed later in this chapter. You should initiate treatment and refer the patient to a physiotherapist.
Grade 3
A grade 3 injury is a complete division of an injured tissue, most commonly ligament or muscle. The most notable clinical finding will be a complete loss of function in the injured part, which means complete laxity in the case of a ligament and weakness in the case of a muscle. Pain may or may not be present, depending on other factors such as inflammation. It will not, however, hurt to stress the torn tissue, simply because it will not be possible to put stress on a divided structure. Clinical findings, such as deformity, absence of the structure in its normal position, visible and palpable gaps in the structure, abnormal laxity of movement, will support the suspicion of a grade 3 injury. The management of grade 3 injuries is either prolonged immobilisation or surgical repair. For some injuries there may be a choice, and there are cases where the techniques are combined. These decisions are made by orthopaedic surgeons in consultation with the patient and you should refer promptly.
Tissue healing
The various tissues of the musculoskeletal system have different capacities to heal and renew themselves. However, it is possible to describe the process of healing in general terms and to propose some basic principles for the treatment of injuries.
Scarring
The optimum form of healing is replacement of injured cells with identical new cells, so that the tissue looks and functions exactly as before. Skin has a high, but not absolute, capacity to regenerate itself in this manner, and it tends to heal relatively quickly. Other tissues, including some in the musculoskeletal system, heal slowly and replace injured tissue with an inert, tough, fibrous tissue which forms a scar at the injury site. Ligament can take more than a year to heal and cartilage may not heal at all.
Scar tissue in a moving part such as ligament or muscle causes problems. The scar cannot reproduce the functions of its host. It is strong but inelastic. It shrinks as it forms, distorting the balance of the surrounding tissue. It may block nerve impulses. It may give rise to adhesions and be the site of complications such as chronic inflammation, pain and calcification of muscle or ligament. The host tissue will probably not return to full function and may be prone to reinjury.
Many patients arrive in a minor injury clinic with acute injuries such as muscle tears and small sprains. These tend to be seen as ‘self-limiting’, not serious, but they may have a better outcome with treatment which minimises the problems caused by the scar.
Cyriax & Cyriax (1993) declare the aim of recovery, when moving parts are injured, to be ‘the formation of a strong and mobile scar’. This means that ‘healing must take place in the presence of movement’. However, healing of a soft tissue occurs through several phases, each requiring a different approach. A premature return to exercise can be as damaging as prolonged inaction.
The healing of soft tissue injuries is normally described in three phases, with graduated changes in the treatment of each phase.
The inflammatory phase
Inflammation is a non-specific response of the body to injury or infection. Its chief signs are redness, heat, swelling and pain. When inflammation affects a moving part it will also cause disability, a fact which matters if the injury is to heal ‘in the presence of movement’. Injury damages blood vessels and cells. These release chemicals which cause a momentary vasoconstriction followed by a prolonged vasodilatation at the site of the injury. Blood fluids full of clotting factors and antibodies swell the area, causing the signs of inflammation. These substances form a clot from which the construction of healing tissue will begin. Macrophages begin to remove waste material from the area.
The inflammatory phase, in the patient’s experience, is dominated by pain, swelling and disruption of normal routines and sleep. It usually lasts for 2 to 7 days. The first aim of treatment is to reduce the severity of these symptoms and to ensure that inflammation is banished as early as possible. Regeneration is yet to begin. Recommend rest rather than movement.
Some complaints, such as supraspinatus tendinitis (Ch. 4) show a non-infective, chronic inflammation which can last for years. Inflammation then becomes the main problem, rather than a stage on the road to healing. It may cause pain and disability with degeneration, scarring and the risk of rupture of the tissue. In these cases, a more active treatment of inflammation is required.
The proliferative phase
The proliferative (or organisation) phase begins as the period of acute inflammation ends.
Fibroblasts synthesise collagen; macrophages remove the haematoma, and a frail network of new capillaries begins to grow. The new scar is developing.
At this stage, a certain amount of movement will improve the organisation of the scar and its ability to cope with the loads that normal use will place on it. However, heavy exertion will damage the delicate new tissues. Prescribing the correct type and degree of exercise is important. If the injury is more than minimal, early advice from a physiotherapist is invaluable.
The maturation phase
The last stage of healing, known as the maturation or remodelling phase, is prolonged, lasting for up to 2 years.
The tissue combines regeneration and fibrosis and develops new tissue or a mature scar. A developing scar becomes stronger in response to the stresses placed on it, loses vascularity and shrinks. Excess tissue produced around the wound during the earlier phases is reabsorbed.
The patient will gradually return to full activity during this phase.
Treatment of acute injury
The treatment of broken bone is dealt with below. This part will cover the treatment of acute injuries to the other musculoskeletal tissues. These are often classed together as soft tissue injuries. There is a variety of soft tissues, and they differ in their responses to injury. It is not always necessary to find out which tissues are injured: it does not always make a practical difference to treatment. There are however many situations where you are expected to make a precise diagnosis, grade the severity of the injury and choose the correct alternative for treatment.
Holistic care
Assess not only the physical effect of a patient’s injury but also the effect it will have on his or her daily life and modify treatment as much as you can to help with any problems.
Bring out the necessary information when taking a history. When patients have injured their hands, find out if they are right- or left-handed, what their jobs are, how they spend their leisure. If a patient cannot walk, ask about home circumstances: is there someone to help them, are there stairs? These questions are more important if the patient is elderly. A minor injury may result in a hospital admission for an elderly person, or in the launching of a concerted effort by community services to avoid that admission.
Patients may have problems related to their jobs. They may be casual workers, or self-employed, and feel unable to take time off to rest an injury. Advise on the best management of the injury and consider whether there are any workplace safety concerns. Your patient may not be able to follow your best advice. Discuss options. Are light duties available? Can schedules be reorganised? It may help the patient in dealing with the employer to give a copy of the treatment sheet, bearing clear advice to rest. (The patient should not normally go to a GP for a sickness certificate until after a week’s absence from work.) You may also be able to speed recovery by referral to a physiotherapist.
The treatment of sports injuries is now a separate specialty. Young athletes often need advice on safe levels of training and the dangers of recurring injury and overuse. They feel pressure to achieve and they may be impatient of the restrictions caused by injury. They are prone to patterns of injury, such as growth plate injuries and bone avulsions, which are specific to their stage of development. Do not ignore a complaint because the history is vague. Seek advice when a problem is not settling down in the expected way (see Chapter 2 for discussion of sports injuries in children).
Treatment in the inflammatory stage
Treatment of a fresh soft tissue injury is the management of the inflammatory stage of healing. This is normally a period of 2 to 3 days but may, depending on the severity of the problem, be as little as 1 day or as much as a week.
Inflammation is a source of pain and disability and, if prolonged, inhibits healing and may worsen scarring and other complications. The aim of treatment is to minimise the period of inflammation and reduce swelling. The method of doing this is known by the acronym PRICE, which means protection, rest, ice, compression and elevation.
Surprisingly, although some approximation to this method of treatment is found everywhere, there has been no consensus on whether or how it works and its optimum application. The Chartered Society of Physiotherapy has tried to address this by issuing a set of guidelines, based on a review of the evidence, for the management of soft tissue injuries during the first 72 hours. This section is based upon that work.
Protection
The idea of protection is to prevent tension on a freshly injured tissue. There are two reasons for this.
1. The tissue will become weakened, over a period of days, in proportion to the severity of the injury, while the inflammatory phase progresses. It may not be clear at the outset how severe this weakness will become.
2. The new fibres which will appear at the site of the injury when healing begins will be frail, and undue stress on the tissue will disrupt them.
Methods of protection are many and are adapted to the part of the body affected, the severity of the injury, the lifestyle of the patient and other factors. They may include bedrest, crutches, plaster casts, strapping, splints and slings.
Minimise the intervention as much as possible while still achieving the aim. Complete immobilisation of the injury, or of the patient, will have adverse results.
Swelling is a feature of the fresh injury, and any treatment should allow for it.
Rest
There is a conflict between the need for rest and the benefits which healing tissues gain from movement. Overuse of a fresh injury may lead to more severe scarring and poorer muscle regeneration, but prolonged immobilisation causes new fibres to be weak and badly organised. Recovery is slower and the results are less than optimal. A middle-ground approach, tailored to the severity of the injury, is required.
Patients are often reluctant to rest. Some people are simply impatient and others have difficult lives. The problem is at its worst when a leg is injured and the patient is asked not to walk.
Nevertheless, rest is the cornerstone of early treatment. Deterioration in the cells and fibres of injured tissues can continue for up to a day after the incident. This can be aggravated by use of the injured part. Swelling will worsen, pain will increase, mobility will decline and the second stage of healing will be delayed and prejudiced.
Rest means not using the injured part, usually for 2 days but in more severe injuries, for up to a week. This time should be spent on the other parts of the early treatment, ice, compression and elevation. Emphasise that time invested now in healing may save time later and lead to a better outcome.
Athletes often have a higher level of knowledge of the management of injuries than the general population and they are strongly motivated to maintain fitness even when injured. You may wish to offer more detailed advice, and you may have a lower threshold for making an early referral to a physiotherapist. The concept of resting the injured part is compatible with exercise to maintain other parts provided that the patient can isolate the different structures while maintaining rest. There are techniques, some discussed later in the chapter, for exercising the structures which are closest to the injury.
Ice
Putting ice on an acute injury (sometimes called cryotherapy) has multiple benefits. The cold reduces nerve conduction, and this is the probable reason why it relieves pain after a brief period when it may feel uncomfortable. The metabolism of oxygen is slowed down at the injury site. This reduces the rate of cell death caused by lack of oxygen, with a beneficial knock-on reduction in the inflammatory process. The ice pack causes local vasoconstriction, which helps to stop bleeding.
Ice is thought to reduce swelling, but it is hard to assess this in the clinical situation because ice is normally used in combination with elevation and compression, and the contribution of the different components of the treatment is unclear. There is experimental evidence which suggests that ice alone may actually increase swelling.
The guidelines urge the value of ice in the first few hours after injury and are less emphatic about its use in later days. This seems to be because the benefits from ice which research actually confirms are all most useful in the early hours. The main reason for continuing use, the reduction of swelling, is not upheld by current research.
Certain risks and contraindications, with greater or lesser degrees of evidential support, apply to the use of ice.
There is some evidence that prolonged use of ice may trigger a reflex vasodilatation (the so-called hunting response, a reflex which is thought to prevent tissue damage in cold conditions). An increase in blood flow would be counterproductive.
Ice should not be put directly against skin or left on for too long. There is the potential for an ice burn, a frostbite injury, if it is used for too long or without a suitable barrier.
Peripheral nerves which lie near the skin can suffer injury from ice. Thin people are more susceptible to the effects of ice than those who have plentiful subcutaneous fat, and the recommended times of application should be adjusted accordingly.
Certain patients should not use ice. It should not be placed over a cut, to an area of poor circulation or reduced sensation, in the case of increased or reduced sensitivity to cold, and where a skin condition exists. Be wary with patients suffering from diabetes, peripheral vascular disease, peripheral neuropathy, sickle cell anaemia and Raynaud’s disease.
The Chartered Society of Physiotherapy recommends the following:
• Apply ice to a fresh injury
• Crushed ice on top of a wet cloth seems to have the best penetration
• Cover the whole area which is injured
• The bigger the circumference of the part which is injured, and the thicker the layer of subcutaneous fat, the longer it takes for ice to cool the deep tissues. Thirty minutes is the maximum recommended time to leave an ice pack on, and this should be reduced where there may be complications. The treatment can be repeated 2 hourly.
Compression
A compression bandage discourages bleeding and swelling by exerting circumferential pressure on the limb. It offers benefits during the first 3 days after injury. Misapplication of pressure, or poor timing of its use, may have undesirable effects. It may cause an increase in swelling.
Compression should not be used in combination with elevation or when the patient is lying down, because it can compromise the circulation to the area. Compression should be at a level which enhances venous and lymphatic drainage out of the limb, but does not reduce arterial flow into it. When a patient is standing gravity makes venous drainage from the leg more difficult and arterial flow easier. The degree of compression needed is relatively high. However these ratios change when the patient walks, sits, elevates the leg or goes to bed. If the foot is elevated arterial flow will require more pressure and venous drainage less. The compression which was ideal when standing is now too great. For this reason do not apply the bandage while the limb is raised. It should exert even pressure, and not be tighter at its proximal end than the distal. Apply in a distal to proximal direction. The standard compression bandage is the double-layer tubigrip, applied, in the appropriate width, from the joint above the injury to the joint below the injury. (The guidelines state that tubigrip is regarded as an effective compression agent but are unclear about the fact that tubigrip tends to apply greater proximal than distal pressure because its standard product is not graduated in width, while limbs taper to ankle and wrist.) It offers gentle compression only, if correctly fitted and is unlikely to restrict the circulation. Patients generally report that it gives comfort and some reduction in pain. It is easy for the patient to put it on himself, a factor which makes crepe bandage impractical if the compression is to be removed and reapplied often.
The chief hazard of a compression bandage is that it may restrict the circulation. Give the patient a few minutes to assess its comfort, check the capillary refill yourself. The patient should remove the bandage if it becomes uncomfortable.
Elevation
The drainage of swelling from the limbs is easier if the patient can reverse the burden of gravity on the venous circulation by raising the injured part above the level of the heart.
The arm needs comfortable support on cushions or pillows so that the hand can be raised to head height or higher and kept there. The ankle will only be raised above the level of the heart if the patient lies down and props the feet above the level of the chest.
Compression should not be combined with elevation for reasons discussed above.
Other aspects of treatment
Exercise
The prescription of exercise for the patient with an injury of grade 2 or more is a task for the physiotherapist or the orthopaedic doctor. Patients with grade 1 injuries will not usually require further referral. For them, you should give simple advice on exercise after injury. When the problem is more severe you may have to give advice on the management of the injury until the physiotherapist can see the patient.
This section offers an outline of the use of exercise, during the three stages of soft tissue healing and the rationale for the advice offered to patients. This is not a blueprint for action. These techniques should only be used by appropriately qualified people. Advice to the patient should be based on the individual, the injury and other circumstances, and it should be simple and cautious. Consult the local orthopaedic and physiotherapy services and make advice compatible with their practice and policies.
The purpose of exercise in the treatment of an injury is to maintain those parts which are not affected by the injury, to restore the parts which are damaged and to allow the patient to return to normal function. Exercise is used to improve flexibility, strength and coordination.
Exercise in the inflammatory phase
During the 2 days after injury, the patient will experience pain, swelling and loss of function of the injured part. There may be muscle spasm. The priority of treatment at this stage is rest and protection of the injury, and the reduction of swelling.
There is no role for active movement or stretching of the injured part. In the case of a muscle injury, this could increase bleeding and separate the torn fibres. If the injury is at a joint, it could increase pain and swelling. If pain is too severe for comfortable exercise, or if exercise triggers pain, it should not be attempted.
Adhesion of an injured ligament to bone is a complication which very gentle passive movement of the joint, without stretching, may help to prevent. Massage of the ligament fibres may also help.
The muscles around the injured joint are prone to wasting and progressive weakness. Isometric exercise, a contraction of the muscle maintained for 6 seconds without changing its length, can help to maintain tone without disturbing the joint. A gentle form of isometric contraction, called muscle setting (contraction without external resistance), is used at this stage, with the joint in a comfortable, neutral position. It is sufficient to increase circulation and delay wasting, and it can reduce spasm. It can also be valuable for injured muscle, provided that the muscle is in a relaxed position. It can reduce shrinkage of the scar. However, it will be counterproductive if the muscle contracts in a stretched position, or too forcefully, and tears the healing fibres.
When muscle is torn, it is difficult to keep mobility in the surrounding joints because the muscle should not be stretched. Joint play exercises allow some mobility to be maintained without stress on the injured tissue. These exercises are a passive exploration of the joint’s range of accessory movements (see below), by distraction (pulling apart the joint surfaces), compression of the joint surfaces, gliding (moving the joint surfaces across each other) and rotation.
The patient should maintain parts not affected by the injury by active movements, taking care not to involve the inflamed area.
Exercise in the proliferative phase
The new tissue which is laid down during the healing phase aligns its fibres in the direction of the stresses which it experiences. In other words, it develops its strength to cope with the tasks which are imposed on it. The forming scar is more elastic and less shrunken if it develops in the presence of movement. Collagenous fibres which are laid down at an immobile injury are badly organised and weak, and the scar is shrivelled. There may also be other complications such as adhesion and contracture.
However, the new tissue is very frail, and violent exercise can damage it, reignite inflammation (sometimes in a chronic cycle) and worsen scarring.
In the proliferative phase, there should be less pain, less swelling and an increased range of movement. If the exercise programme is too heavy, there may be a return of earlier symptoms, and the aim is to avoid this and make improvement at a pace which is comfortable.
There can be some resumption of active and weight-bearing exercise, using aids such as splints, strapping and walking sticks (see below). Isometric exercise, below the intensity which causes pain, can continue.
Specific difficulties can be addressed, joint restriction and shortness of muscle, by combinations of stretching, passive joint play and isometric exercise, depending on the features of the problem.
Exercise in the remodelling phase
As the new collagen strengthens, a graduated programme of exercise should subject it to the types of stress which it will face in normal life. Attention must still be paid to any adverse symptoms. If the new tissue is injured, the risks of regression, chronic inflammation, restricted movement and poor healing are still there.
The difficulties of reintegrating the injured part into the body’s overall activity must be addressed. If the injury has involved sensory nerves, especially in ligaments, it may be that there is a loss of proprioception. This is the capacity of the brain to locate parts of the body in space without seeing them. It allows you to touch your nose with a fingertip with your eyes closed. Loss of proprioception damages coordination in that part of the body. There is also some evidence that sensory changes occur at other sites not directly related to the injury. The aim of rehabilitation must be to regain full coordination of healthy and injured tissues. The programme will progress from uncomplicated to multi-directional movement, and to movements which challenge the patient’s coordination. The intensity and nature of such a programme will depend upon the activity the patient is returning to, whether an office worker, a builder, an athlete or a couch potato. The target is to restore full function as the patient knew it before the injury.
Problems such as weakness in the muscles around an injured joint, or restriction in the joints around an injured muscle, together with any other complications such as adhesions must be addressed by the means already described. Splints and other devices may still be required until any imbalance between joint and muscle has been rectified.
Heat
The effect of heat on an injury is to increase the blood flow and stimulate cell activity. Its benefits include a decrease in muscle spasm, a reduction of pain and a spur to the healing process. It may also help to prepare tissues for a session of exercise.
Heat should not be used in the first stage of healing, when the objective is to reduce swelling and inflammation.
A simple way to warm injured tissue, and to relax muscle which is in spasm, is to use a hot water bottle – take care to avoid burns. There are various packs and rubefacient rubs which are more or less effective. The patient must avoid painful levels of heat, prolonged use of heat and irritant and allergy-provoking substances. Any person with a tendency to bleed or a restricted circulation, poor sensation or malignancy should avoid the use of heat treatment.
Ultrasound
Ultrasound is a treatment normally used by physiotherapists and has several applications for musculoskeletal injuries. It sends high-frequency sound waves, through the medium of gel on the skin, directly into tissue. Its effects are described as thermal and non-thermal. The thermal effects are similar to those of other forms of heat therapy. Non-thermal effects improve the healing environment by stimulating tissue renewal and reducing swelling.
Ultrasound is helpful for the reduction of haematoma, swelling, spasm, certain kinds of pain, myositis ossificans, adhesions and contractures.
Walking aids
The walking aids which are commonly available for the otherwise healthy and mobile person with an acute injury are walking sticks, elbow crutches and wooden axilla crutches.
Patients often resist the idea of using a walking aid. For those patients who need one, it is a part of their treatment. Explain that it is not regarded as optional.
It is worth emphasising that the purpose of a walking aid, based on the rationale that healing should occur in the presence of movement, and that healing tissue organises itself to meet the demands that are placed on it, is to return the patient to a normal walking pattern at the earliest possible time. A walking aid combines two virtues: it lets the patient use the damaged part in the correct way, which means that the injured tissue is getting the best preparation for the tasks that will follow healing, and it supports the vulnerable new fibres during the proliferative stage. It is also the case that limping, even for a few days, is tiring, depressing, and stressful to parts of the body which were not originally injured. There can also be a safety issue. A limp may occur because a joint, perhaps the knee or ankle, is too swollen to move through its full range. This will prevent the patient from standing on a straight, stable leg. There is a risk of a fall, and of further injury.
There is often reluctance to issue walking aids in emergency departments, caused, perhaps, by arbitrary local policies, by lack of awareness of the indications for their use or by a lack of the resource. Recovery of the sticks and crutches which patients have discarded is a universal problem for emergency areas which it is difficult to solve without wasting excessive resources chasing them up. However, it is an interesting experience, when you have a patient who is able to walk but who has a limp, to supply a single walking stick and observe the change, both in the gait and in the patient’s mood.
A patient who needs a walking aid probably also needs review, either by you or the physiotherapist. This can be a good time to reclaim the walking aid. A physiotherapist may take a patient through a graduated process, from axilla crutches through elbow crutches to walking stick.
The indication for giving a walking stick is that the patient has a limp which is significant for the walking pattern, but not unstable. Two walking sticks can also be given. If one stick is used, the patient should hold it in the hand opposite the injury so that the arm and leg swing in the natural way, left with right and right with left. If walking sticks are not sufficient to stabilise the patient, but he or she can still take some weight on the injured foot, then elbow crutches can be tried for the support of partial weight bearing. They are more convenient (and usually more aesthetically acceptable) than axilla crutches but not quite so stable. Some young, fit patients can manage to use elbow crutches while non weight bearing, but there is a marked increase in stability when axilla crutches are used. The usual indication for giving axilla crutches is that the patient is completely unable to walk on one foot.
Crutches and sticks should be fitted so that there is slight flexion at the elbow when the hand rests on the grip, but the shoulder should not be pushed up, nor should the patient have a bobbing motion. If the walking aid is too short the patient tends to stoop and his or her body weight will be badly placed for safety and for the effort of moving forwards.
Elderly patients will rarely cope with crutches, which require strong arms, balance and agility, and judgement in hazardous places such as roads, kitchens and stairs. A Zimmer frame is sometimes useful for the injured elderly, but it requires some ability to bear weight on the injury and is not a substitute for axilla crutches. Treatment may have to be directed primarily to the patient’s immobility rather than the injury itself. This may involve crisis community care or hospital admission.
Splints, strapping and slings
Splints, strapping and slings are used to prevent movement around one or more joints. The immobilisation of fractures is discussed below. Some of the devices mentioned here are also used for bone injuries.
Devices used in the emergency department and the minor injury clinic for immobilising injured parts include the wrist brace, the thumb spica, buddy strapping for fingers and toes, the soft collar and the collar and cuff sling for the shoulder. Plaster of Paris, and similar materials is sometimes used for severe soft tissue injuries.
The degree of immobilisation varies depending on what is possible at the particular joint, on the device used and on the intended effect of the treatment. There are different indications for the use of these devices, and some of these will be discussed throughout the book.
Use splints with care. Restriction of movement is never a good option, although it is often necessary. It can lead to complications, such as stiffness, contracture, wasting, weakness and adhesion. Certain joints, notably in the hand, can suffer permanent contracture if they are splinted in an unsafe position. Strapping at a fresh injury can restrict circulation if the swelling increases. Always have a clear objective when using a splint, based on accepted principles of treatment and the particular patient’s condition. Give advice, preferably in writing, on how it is to be used, any possible complications and an appropriate exercise routine.
Rest
Rest is the foundation of the PRICE programme, and a splint or similar device will certainly rest a joint. However, complete immobilisation is not necessarily the same thing as rest. In the case of a bleeding muscle, a patient may need to rest completely, whereas one with a ligament tear may be advised to perform gentle movement to prevent adhesions. PRICE is usually recommended for 2–3 days only, after which movement is gradually introduced. The advice on the use of the splint should be consistent with the rest of the treatment.
Relief of pain and other symptoms
Random movement of an injured joint may be the main source of a patient’s pain. There may be spasm. Support might do more than any other measure to make the patient comfortable. The most painful phase of an injury may only last for a couple of days. Advise the patient to wean off the splint and on to gentle exercise after this time.
Supported movement
Physiotherapists will sometimes use strapping to stabilise a painful joint so that the patient can begin to exercise it with reduced movement at selected tissues. The ankle can be strapped so that the foot is slightly everted, and this will reduce stress on the lateral ligaments, while still allowing them to have some movement. Such strategies are in keeping with the aims of treatment during the proliferative phase of healing. Sportsmen often use strapping to stabilise an injury or a vulnerable joint while they play.
Safety
In cases where complete examination is deferred to a later day, or where a patient is to be transferred with an unstable injury, a splint may be of value in preventing any worsening of the problem. The decision to immobilise a joint may have more to do with the severity of the patient’s symptoms than the exact type of injury. Guiding factors are the patient’s posture (torticollis, cradling the arm, holding the head to prevent neck movement), the range of movement at the affected part, the ability to use the injured part, the level of pain and signs such as swelling and bruising.
Bone
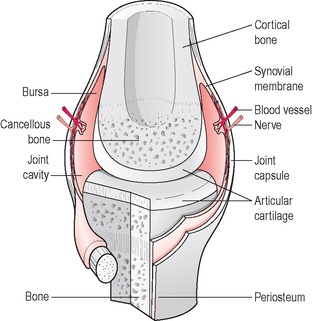
Bone is a hard connective tissue, made of collagen and mineral salts, especially calcium. There are two basic bone tissues, cortical (also compact, or dense) and cancellous (also spongy, or trabecular) (Figure 3.4). Cortical bone is smooth and dense and forms the outer shaft of the long bones. Cancellous bone is porous and its tiny calcium struts absorb and channel weight like a buttress.
 |
| Figure 3.4 • |
Bones are classified into various types:
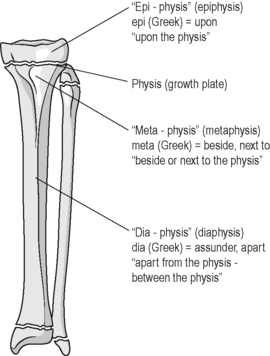
1. Long bones: the main group represented in the limbs. These bones have a cylindrical shaft or diaphysis, made of cortical bone on the outside and spongy bone within, with a hollow core, the medullary cortex, where yellow marrow is produced. The diaphysis is covered in a membrane called the periosteum, which has a lavish nerve and blood supply and which provides attachment for tendons and ligaments. The ends of the bone are called the epiphyses (singular, epiphysis). In children there is the physis, or epiphyseal plate, between the epiphysis and the diaphysis, made of cartilage, where growth occurs in the bone. This plate closes when growth is complete. The articular ends of the epiphyses, the parts which form joints with other bones, are coated in articular or hyaline cartilage.
2. Flat bones (the scapula and sternum).
3. Short bones (the carpals and tarsals).
4. Sesamoid bones, which lie within tendons apparently to increase the mechanical efficiency of the tendon (e.g. the patella and pisiform, with others in hand and foot).
5. Irregular bones (the bones of the pelvis). These bones all have an outer layer of cortical bone, with spongy bone inside. They may be cuboidal, plate-like, oval or irregular.
Figure 3.5 illustrates a growing child’s bone.
 |
| Figure 3.5 • |
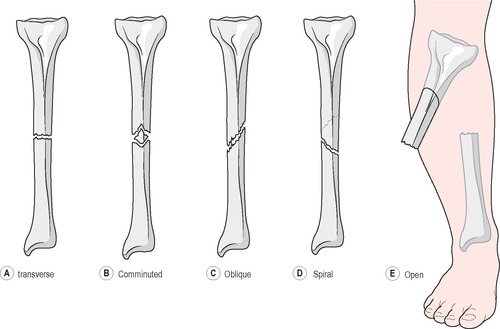
Bone injury: fracture
A fracture is a break in the continuity of a bone (Figure 3.6). It can be caused by direct violence or by indirect, transmitted force, with injury at a distance from the point of contact. Injury may be transmitted by an axial force, often along the shaft of a long bone (e.g. the head of the radius, at the elbow, is fractured by a fall on the outstretched hand), or by twisting or leverage. Traction (or distraction), a pulling force which separates joint surfaces, can cause avulsion, when a soft tissue such as tendon or ligament pulls off a piece of the bone to which it is joined (and it can cause dislocation). Crush force, the compression of the part between two hard surfaces, may break bone, often with soft tissue damage and the complications of swelling. Areas of cancellous bone, such as the vertebrae, are subject to crush, but the commonest crush injuries seen in a minor injuries clinic are to the tips of the fingers.
 |
| Figure 3.6 • |
Stress fracture is caused by the cumulative fatigue of overuse, rather than a single violent event, and pathological fracture by disease which weakens bone.
Types of fracture
Fractures may be open (compound) or closed (simple). An open fracture has a wound at the site of the injury which may have been caused by the broken end of the bone pushing through the skin. If the injury is closed, the skin is intact. An opening in the skin over a broken bone, or the protrusion of the bone through the skin, exposes the bone to infection. Bleeding may be severe in such injuries.
A fracture may be transverse, with a break at approximately a right angle across the shaft of a long bone, dividing it into two pieces. This happens after a direct blow or bending force to the shaft. The separated surfaces are horizontal and usually keep good position and unite without shortening. However, the broken areas are small and poised one on top of the other, like two pencils balanced end on end. They need support until healing is well advanced.
An oblique fracture is one where the bone is broken diagonally along its shaft. This is caused by a blow to the site or indirect force. A twisting force may cause an obliquely angled spiral fracture. The broken areas are larger than is the case with a transverse fracture. This makes union easier, but the angle of the broken surfaces and the action of the muscles attached to the bone, may encourage slippage, angulation and shortening. The bone is sharply pointed and wounding of soft tissue, nerve and blood vessel is possible.
Fractures in which the bone is broken into more than two parts are called comminuted. Injuries of this kind are usually caused by direct force, sometimes by crush. There are various classifications of these fractures, depending on the number of fragments and their potential for union. They tend to be unstable and difficult to treat. The violence of the injury is usually severe and soft tissue damage and impaired blood supply, at least to some of the fragments, are common.
Impacted fractures are those in which the broken ends of bone are driven together by a force along the axis of the bone. Shortening and displacement coexist with an unreliable stabilising of the broken ends. Sometimes the position will obstruct normal function. Fracture in which bone is punched out and deposited in the underlying soft tissues is called depressed. This type of injury occurs in the skull.
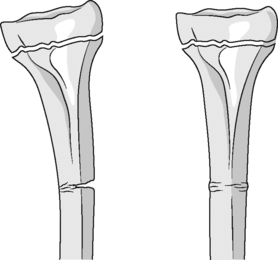
In children, the bones are soft and greenstick fracture is common (Box 3.2, Figure 3.7). This occurs when an angulation force is applied to one side of the bone, and the bone bends and breaks, with a tear of the periosteum, on the opposite side. The periosteum remains intact on the concave side of the injury. There is a degree of deformity, but, unless it is severe, it is likely to correct itself during healing. A buckle or torus fracture (torus is an architectural ‘collar’ which is found on classical pillars and the term evokes the bulge which is seen on the outline of the bone) is one where axial force has compressed the bone (Box 3.3). The periosteum remains intact but there is a small bulge which can be seen on the outline of the bone on an X-ray. These injuries usually heal quickly.
Box 3.2
• Young bones are relatively porous and soft, leading to various forms of incomplete fracture
• The periosteum is thicker and less firmly attached to bone, so that it tends to remain at least partially intact in fracture and helps to keep the bone together. Non-union is relatively rare
 |
| Figure 3.7 • |
Box 3.3
• Greenstick fracture results from an angulation of the bone, with tension on the convex side, and compression on the concave
• One side of the cortex is broken, through half the width, and often there is a vertical split at the inner end of the fracture
• Torus is a Greek architectural word for a round projection, it results from axial compression
• There is buckling without angulation, usually in the metaphysis
• The commonest site is the distal forearm
A bow fracture occurs when sufficient force is applied to a soft long bone to bend it, but it does not break. This can cause special problems because there has not been sufficient trauma to trigger healing, and therefore no remodelling and no correction occurs. If the injury is to a forearm bone it may change the relationship between radius and ulna and impair pronation and supination. A bow fracture may need to be manipulated. Fractures to the child’s growth plate, sometimes involving the near joint, may arrest the growth of the bone and need expert assessment and, in a few cases, surgical reduction. The Harris–Salter classification of growth plate injuries is widely used (Figure 3.8 and Box 3.4). It is a quick guide to severity, treatment and likely outcome of the various types of injury.
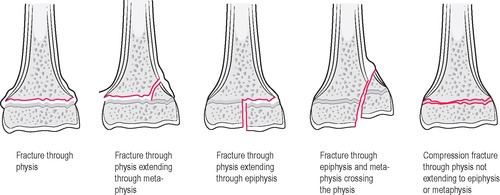 |
Figure 3.8 • Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|