Sharon Oliver
Basics of Diagnostic Coding
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Identify three purposes of the most current diagnostic coding system.
3. Describe how to use the most current diagnostic coding system.
4. Explain and apply the basic coding rules in the use of the ICD-9-CM.
7. Explain the importance of the Tabular Index.
8. Correctly use instructional terms and symbols as defined in the ICD-9-CM.
9. Explain the use of V and E codes.
Vocabulary
ancillary diagnostic services Services that support patient diagnoses (e.g., laboratory or radiologic services).
and In the context of the ICD-9-CM, and should be interpreted as and/or.
coding Converting verbal or written descriptions into numeric and alphanumeric designations.
diagnostic statement Information about a patient’s diagnosis or diagnoses that has been extracted from the medical documentation.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) The manual that establishes the system for classifying disease to facilitate collection of uniform and comparable health information for statistical purposes, for indexing medical records for data storage and retrieval, and to facilitate payment.
International Statistical Classifications of Diseases and Related Health Problems, Tenth Revision, Clinical Modification (ICD-10-CM) The current ICM rules manual, which contains the greatest number of changes in the ICD-CM system in ICD history. To allow more specific reporting of diseases and newly recognized conditions, the ICD-10-CM contains approximately 55,000 more codes than the ICD-9-CM.
manifestation An indication of the existence, reality, or presence of something, especially an illness.
see category A direction to the coder to see a specific category (three-digit code); this instruction must always be followed.
Scenario
Mike Simeone has been employed by Dr. Buckner and Dr. Walker in their gastroenterology practice for the past 2 years. He works as an administrative assistant in medical records and simultaneously has been enrolled in the medical assisting program at his local college. As he has become more knowledgeable, Mike has been given more responsibility in tasks related to diagnostic coding, such as abstracting a diagnostic statement and selecting the most accurate diagnostic code for billing and reimbursement. To perform diagnostic coding, Mike uses a manual called the International Classification of Diseases, Ninth Revision, Clinical Modification, or ICD-9-CM.
Mike’s experience working in medical records gives him an understanding of the importance of correct, thorough documentation. His strong skills in reading and understanding physicians’ orders, treatment plans, chart notes, diagnostic statements, and other medical records will prove invaluable as Mike learns more about diagnostic coding and refines his coding skills.
Mike is aware of the legalities and importance of proper billing as it affects reimbursement. He knows that the practice is committed to compliance with all the regulations affecting the operation of the facility, and he knows the patients’ charts are well documented, which makes his new tasks easier to accomplish. Mike is a conscientious worker and looks forward to using his experience to advance his position in the practice and in the medical assisting profession.
While studying this chapter, think about the following questions:
Accurate medical record keeping and efficient claims processing are possible only if each and every procedure and service provided during an office visit or encounter is identified. An encounter is any contact between a patient and a provider of service. The term encounter is used for all settings, including hospital admissions.
The physician or provider also must provide diagnostic information that demonstrates the need for the procedures and services. A diagnosis is the determination of the nature of a condition, illness, disease, injury, or congenital defect. In medical coding, the terms assessment and diagnostic statement are synonymous with diagnosis.
Both components (i.e., the diagnostic findings and the procedures and services) are used to determine the charges for an encounter and to generate an insurance claim. This chapter focuses on teaching the medical assistant how to gather diagnostic information and translate it into a diagnostic code. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) coding manual is used for this purpose. Two main parts of the ICD-9-CM are the Tabular Index (Volume 1) and the Alphabetic Index (Volume 2). The Tabular Index describes conditions, illnesses, diseases, and injuries; it also includes the sections Classification of Factors Influencing Health Status and Contact with Health Service (V Codes), and an index for Supplemental Classification of External Causes of Injury and Poisoning (E Codes). The Alphabetic Index is used to locate the codes in the Tabular Index based on the diagnosis provided in the medical record.
The ICD-9-CM manual is used to assign a standardized numeric or alphanumeric code to the diagnostic statement written by the provider. Diagnostic statements are found in operative reports, discharge summaries, history and physical (H&P) reports, and reports on ancillary diagnostic services that support the patient’s diagnosis or diagnoses. Ancillary diagnostic services include radiology, pathology, and laboratory service reports. These reports are used by healthcare providers to code and report clinical information, as required for participation in Medicare and Medicaid insurance programs, and by most third-party payers and insurance carriers. The ICD-9-CM also is used to track healthcare statistics. Practice management software, clearinghouses, and third-party payers recognize these codes, which simplify the reimbursement process and speed payment to healthcare providers.
Getting to Know the ICD-9-CM
What Is Diagnostic Coding?
Diagnostic coding is the translation or transformation of written descriptions of diseases, illnesses, or injuries into numeric or alphanumeric codes. Use of the ICD-9-CM facilitates accurate medical record keeping and efficient claims processing. The manual identifies the disease or injury for which a patient was treated as a three-, four-, or five-digit code. ICD-9-CM codes are used in the claims submission process to request reimbursement from payers, to track the diagnoses treated by the physician to provide statistical data for research, and for other purposes.
The CMS publication “Avoiding Medicare Fraud and Abuse: A Roadmap for Physicians” maintains that the five most important federal fraud and abuse laws that apply to physicians include the:
Violations of these laws may result in non-payment of claims, Civil Monetary Penalties (CMPs), exclusion from the payor program, criminal and civil liability, and in extreme cases, jail time. These laws may be changed or updated, so the person who is responsible for coding must pay close attention to detail and act as a sort of “medical detective” to build a case against a physician or clinic. Both the ICD-9-CM and the CPT coding manuals are updated annually. The Federal Register announces most changes and new coding manuals often have a few pages dedicated to the updates for that particular year. Accurate use of the ICD-9-CM manual is essential for correct translation of the diagnostic statements in the medical record into numeric or alphanumeric codes.
Why Use ICD-9-CM Codes?
The ICD-9-CM codes are important for several reasons. They are used to:
• Create a more convenient method of data storage and retrieval
• Help maximize reimbursement to the provider
• Shortening the claims processing time
• Facilitate and assess regulatory compliance through the use of guidelines and other instructions
• Help evaluate the appropriateness and timeliness of medical care
Evolution of ICD Coding
Classification systems are used by healthcare organizations to organize healthcare data and make retrieval meaningful. The early Greeks were the first to group data by disease processes. Captain John Graunt of London was the first to publish mortality and morbidity statistics, in the London Bills of Mortality (1662), which was the first real attempt to study disease processes from a statistical viewpoint. Later, in the 1830s, William Farr introduced uniformity in the use of statistics. His work helped classify diseases by anatomic site. He published the International List of Causes of Death and provided the foundation for current vital statistics.
In 1893 Dr. Jacques Bertillon developed the Bertillon Classification of Causes of Death. The American Public Health Association (APHA) recommended adoption of this classification system for Canada, Mexico, and the United States and further recommended that the system be revised every 10 years. Subsequent revisions were called the International Classification System of Causes of Death. Revisions were completed in 1900, 1910, 1920, 1929, and 1938.
In the 1950s the U.S. Public Health Service published the International Classification of Diseases, which was adapted for indexing hospital records by diseases and operations. This became the International Classification of Diseases, Adapted (ICDA). Subsequent modifications in 1962 provided greater detail and introduced a classification for surgical procedures. In 1968, because of the need for even greater detail and specificity, the eighth revision of the ICDA was adapted for use in the United States (ICDA-8). ICDA-8 provided the basis for coding morbidity and mortality statistics in the United States and served as a method of indexing all diagnoses and operative procedures in hospital records.
In 1975 the ICDA was renamed the International Classification of Diseases, Ninth Revision (ICD-9). In 1979 the National Center for Health Statistics (NCHS) developed a modification of the ICD-9 for use in the United States. That modification, the ICD-9-CM, has been used in the United States ever since.
Legislation has been passed to formally adopt the tenth revision, or modification, of the diagnostic and procedural coding manuals (ICD-10) for use in the United States. ICD-10 is a significant upgrade and improvement to the coding manual currently in use. (See Appendix B for more information about the International Statistical Classifications of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) and the Procedural Coding System (ICD-10-PCS.) The effective date for these publications is October 1, 2014.
ICD-9-CM Codes
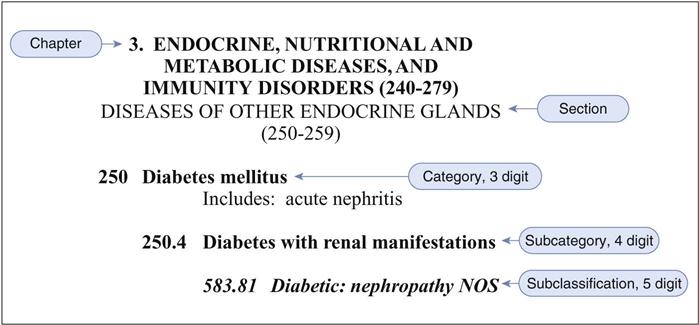
ICD-9-CM codes are listed in the Tabular Index (Volume 1) of the ICD-9-CM coding manual. The coding system consists of a three-digit category code that represents a specific disease, illness, condition, or injury within a general disease category. For example, 250 is the disease classification, or category, for diabetes mellitus. Up to two digits can be added for further definition and specificity. The two additional digits are the fourth digit, or subcategory, and the fifth digit, or subclassification.
Consider the example of diabetes category code 250 (Figure 18-1). Using this code and the conventions and guidelines (discussed later) in the ICD-9-CM manual, it can be determined that a fourth digit must be added that describes whether any disease manifestation is present that was caused by the diabetes, such as kidney disease or diabetic retinopathy. A fifth digit must also be added that describes the type of diabetes (e.g., type 1 controlled or type 2 uncontrolled).
The ICD-9-CM conventions, notes, and guidelines, combined with the diagnostic statement or statements from the medical record, provide the details needed to select the most accurate three-digit category code and, if applicable, a fourth digit (subcategory) and fifth digit (subclassification) code.
Structure of the ICD-9-CM
The ICD-9-CM is published in various media, including book, CD, and downloadable file. Every year the ICD-9-CM manual is reviewed for changes. Additions, revisions, and deletions are made to many of the diagnostic codes, code descriptions, and guidelines. The medical assistant must always use the current year’s coding manual to ensure correct coding and billing and to comply with regulatory guidelines.
Depending on the publisher, the layout, symbols, color coding, and some other features vary somewhat; however, the format, conventions, tables, appendixes, content, and basic structure are the same. The basic ICD-9-CM manual is made up of three volumes.
• Volumes 1 and 2, mentioned earlier, are used for diagnostic coding by hospitals, physicians, and all other providers of service. Volume 1, the Tabular Index, contains all the diagnostic codes, which are grouped into 17 chapters of disease and injury. Chapters are broad sections of the ICD-9-CM coding manual grouped by disease or illness (e.g., Chapter 10 contains diagnostic codes for diseases of the genitourinary system).
Most coding manuals, depending on the publisher, have an Introduction that provides the historical background. The ICD-9-CM coding manual also contains other useful information. In the ICD-9-CM, the coder will find the format and conventions of the coding manual; anatomic illustrations; special coding instructions for many conditions, illnesses, and injuries; and the current year’s ICD-9-CM Official Coding Guidelines for using ICD-9-CM codes. The Centers for Medicare and Medicaid Services (CMS) prepares the guidelines for using the ICD-9-CM codes and instructions on how to report them on claim forms. The guidelines are a set of rules that have been developed to accompany and complement the official conventions and instructions provided in the ICD-9-CM manual.
Annual modifications are made to the ICD-9-CM through the ICD-9-CM Coordination and Maintenance Committee. The committee holds meetings twice a year, at which time modification proposals are submitted to the committee. Modification proposals that are approved are incorporated into the official government version of the ICD-9-CM and become effective for use October 1 of the year after their presentation.
Tabular Index (Volume 1)
The Tabular Index is a numeric listing of diagnosis codes and detailed descriptions. As mentioned earlier, a diagnosis is the determination of the nature of a disease, injury, condition, or congenital defect. The Tabular Index consists of the following:
• Seventeen chapters that classify diseases and injuries
• Two sections containing supplementary classification codes (V and E codes)
• Four appendixes (Appendix B, Glossary of Mental Disorders, was deleted October 1, 2004)
A chapter is a group of three-digit code numbers that describes a general category. For example, the code range 240-279 comprises Chapter 3: Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders.
Each of the 17 chapters is subdivided into four levels (see Figure 18-1):
• Category: A three-digit code that represents a specific disease, illness, condition, or injury within a chapter (e.g., in Figure 18-1, Category 250 represents diabetes mellitus). A three-digit code is used only if it is not further subdivided.
• Subcategory: A fourth digit that adds information or description to the category code. For example, in Figure 18-1, under Category 250, a fourth digit is used to describe whether any disease process or manifestation exists that was caused by the diabetes mellitus. Category 250 has 10 fourth-digit subcategory codes. Fourth digits sometimes describe the location of the illness (e.g., code 410.2 indicates of inferolateral wall).
• Subclassification: A fifth digit which, when used appropriately, adds the highest level of detail to the illness or injury. In Figure 18-1, under Category 250, fifth digits are used to describe the type of diabetes mellitus (e.g., type 1 controlled or type 2 uncontrolled). Fifth digits sometimes describe the episode of care (e.g., code 410.21 indicates MI [myocardial infarction] of inferolateral wall, initial).
Supplemental Classifications
The two supplementary chapters in the Tabular Index contain V codes, which describe factors that influence health status and contact with health services that cannot be classified elsewhere, and E codes, which describe external causes of injury or poisoning.
V Codes.
V codes are used either when the patient is not currently ill or to explain problems that influence a patient’s current illness, condition, or injury. The Supplementary Classification of Factors Influencing Health Status and Contact with Health Service (V01-V89) is used in cases such as preventive vaccination or when a patient encounter is only for administration of a treatment, such as dialysis, chemotherapy, or screening.
E Codes.
The E code chapter, the Supplemental Classification of External Causes of Injuries and Poisoning (E800-E999), classifies environmental or external causes of injury, poisoning, or other adverse effects on the body. For example, an E code would be used to describe the details of an automobile accident to explain how a patient’s injuries occurred. E codes also identify the place of occurrence (i.e., where the event happened) and not the patient’s activity at the time of the event.
Appendixes
The Tabular Index currently has the following four appendixes (as mentioned, Appendix B, Glossary of Mental Disorders, was deleted October 1, 2004).
Conventions Used in the Tabular Index
Conventions are abbreviations, punctuation, symbols, instructional notations, and related entities that help the medical assistant or coder select an accurate, specific code. Conventions are found in the Tabular Index. Understanding their meaning and using them as guides are crucial to accurate coding. Each publisher offers its version of the ICD-9-CM, and some differences may be seen in the symbols, notations, colors, or other reference marks used. The most common conventions are described here.
Abbreviations.
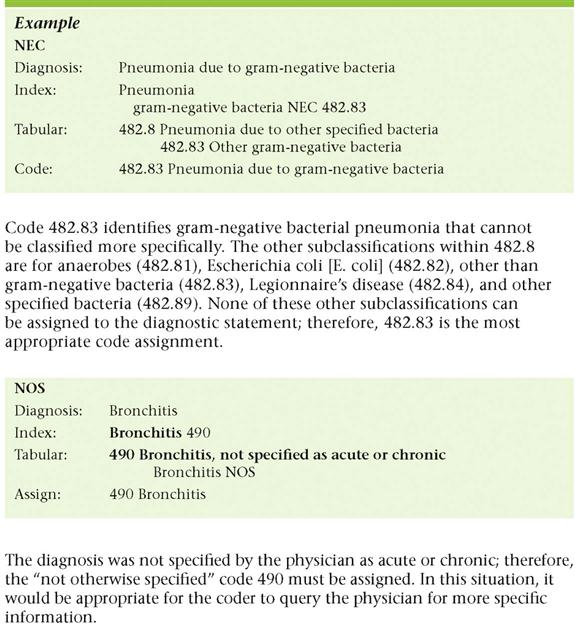
Two primary abbreviations are used in the Tabular Index: NOS and NEC (Figure 18-2).
Punctuation.
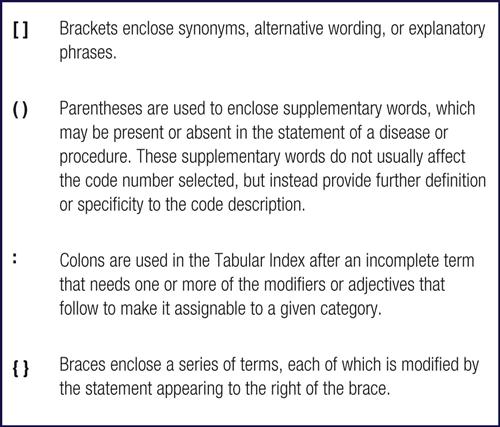
Four basic forms of punctuation are used in the Tabular Index: brackets, parentheses, colon, and braces (Figure 18-3). Each form serves a different purpose for reading and understanding the code descriptions.
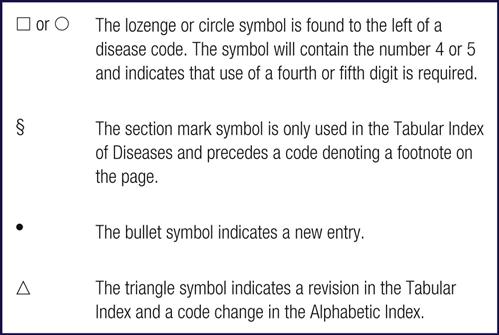
Symbols.
Symbols are used to designate the requirement of a fourth or fifth digit (or both), new entries, and revised text or codes. Other symbols may be included, depending on the publisher. Regardless of publisher, all symbols or other changes are described completely in the Introduction to the ICD-9-CM,. The most commonly used symbols are shown in Figure 18-4.
Other Conventions.
Two other conventions used in both the Alphabetic Index and the Tabular Index are bold and italic fonts.
Instructional Notations.
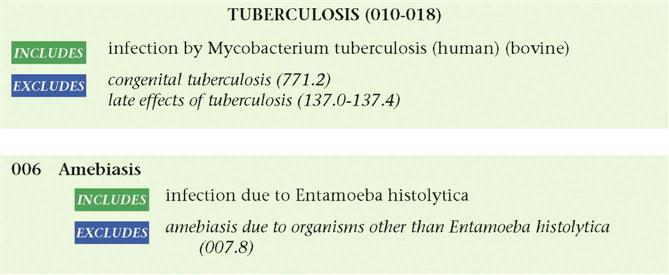
Instructional notations are critical to correct coding practices. The instructional notations appear in red type in the Tabular Index (Figure 18-5). The instructional notations include the following:
Related Terms
Alphabetic Index (Volume 2)
The Alphabetic Index consists of an alphabetic list of diagnostic terms and related codes; three supplementary sections (the Hypertension Table, Neoplasm Table, and Table of Drugs and Chemicals), and a separate Alphabetic Index for E Codes (Index to External Causes). In most published versions of volumes 1 and 2, a Summary of the Additions, Deletions, and Revisions to the Tabular Index for the current year is included and typically is found at the end of the main Alphabetic Index (Volume 2).
The Alphabetic Index includes main terms, nonessential modifiers, modifying terms, and subterms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree