B
Barium enema
Also called: (BE); Double-Contrast Barium Enema, (DCBE)
Basics the nurse needs to know
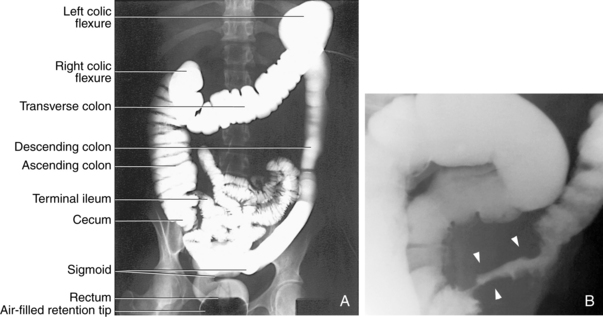
The barium enema is a radiographic test that is used to investigate the cause of a change in elimination patterns, melena (blood in the stool), obstruction of the colon, or the presence of an abdominal mass that has a suspected location in the colon. Barium is a contrast medium that is radiopaque, has a different density than body tissue, and can be instilled into hollow organs such as the colon. In the barium enema procedure, the entire colon and the distal portion of the ileum can be visualized on x-ray film (Figure 18). The technique may be done as a single contrast study that takes spot x-ray images of the colon with the barium filling the lumen. Alternatively, a double contrast study may be done. In this method, barium is instilled and then drained out of the colon, leaving a residual coating of contrast on the luminal mucosal surface. Then the colon is slowly filled with air that serves as a second contrast medium and also dilates the lumen of the colon. Spot x-ray images of the colon are taken after the contrasts are instilled completely.
How the test is done
After the colon is emptied of feces, the contrast medium enema is administered by the radiology technologist. Barium and possibly additional air contrast are instilled as contrast media. If perforation is suspected or the patient is at risk for intraperitoneal leakage of the contrast, barium is not used and a water-soluble contrast medium is used in substitution. Fluoroscopic images are taken at intervals to monitor the instillation of the contrast. The patient must retain the contrast medium in the colon during the test. The patient’s positional changes, (supine, prone, lateral) are used to enhance gravity flow of the contrast medium throughout the entire colon. X-rays are taken to image the colon and in particular, the abnormal area(s). The procedure takes 45 minutes to 1 hour to complete.
Interfering factors
NURSING CARE
Pretest
Posttest
Bilirubin, serum, urine
Basics the nurse needs to know
Bile, with its component direct bilirubin, flows from the hepatic ducts of the liver to the biliary ductal system. It is stored in the gallbladder and, on demand, flows through the cystic duct, the common duct, and enters the duodenum to help in the process of digestion of fats.
Jaundice
Classifications of jaundice
One way to classify jaundice is based on the physiologic location of bilirubin manufacture, transport, and excretion. As seen in Table 4, pathophysiologic changes will be detected by elevated values of the indirect or direct bilirubin tests. These tests help provide information about the cause of the problem. The prehepatic category refers to bilirubin manufacture and transport before the blood circulation reaches the liver. The hepatic category refers to problems within the liver because of injury to the liver cells or blockage within the intrahepatic bile ducts. The posthepatic category refers to blockage of bile within the liver or in the gallbladder or gallbladder ducts.
Table 4 Classifications of Jaundice
| Category of Jaundice | Type of Bilirubin Elevation | Origin of the Problem |
| Prehepatic | Indirect (unconjugated) | Excessive hemolysis of red blood cells |
| Hemolytic jaundice | ||
| Hepatic | Indirect (unconjugated) | Defect in transport or conjugation in hepatocytes |
| Physiologic jaundice | ||
| Direct (conjugated) | Injury to, or disease of, hepatocytes | |
| Blockage of intrahepatic bile ducts | ||
| Intrahepatic cholestasis | ||
| Posthepatic | Direct (conjugated) | Blockage in the biliary ductal system |
| Extrahepatic cholestasis |
If the infant is born with biliary atresia, the biliary drainage system is incompletely developed and there is no open passageway for bile to flow into the duodenum. Because of the blockage, a rapid, severe rise in total bilirubin and direct bilirubin will occur. Urinary bilirubin will be positive in biliary atresia and hepatic disease, but not in hemolytic jaundice.
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other venipuncture or capillary puncture procedures (see Chapter 2), with the following additional measures.
Posttest
 Nursing response to critical values
Nursing response to critical values
If the neonatal serum bilirubin rises to a critical value in the newborn or premature infant, notify the physician immediately. If the elevation is considered to be pathologic, rather than physiologic, the baby must be evaluated medically to determine the cause of hyperbilirubinemia. At the level of the critical value, the physician will consider the treatment of phototherapy. If the level goes higher, phototherapy will be performed, and exchange transfusion may also be necessary.
Biopsy, bone
Also called: Bone Needle Aspiration Cytology
Basics the nurse needs to know
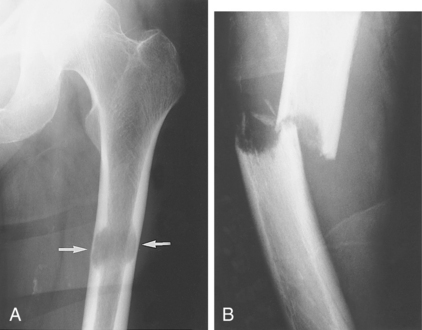
Malignant primary bone tumors are characterized by borders that extend outward into the surrounding fat or muscle tissue or inward into the marrow and medullary cavity, or both (Figure 19). The most common primary bone malignancy is osteogenic sarcoma, which is often located in the region of the knee. Malignant bone tumors may also be metastatic tumors, with the primary site located elsewhere in the body. Most bone metastases are in multiple sites, usually located in the vertebrae, ribs, sternum, or pelvis.
When a bone tumor is suspected, a bone scan or computed tomographic (CT) scan is performed first. These preliminary tests are used to verify the presence of the tumor and identify the site for bone biopsy. They also are used to identify additional metastatic sites and to help assess the extent of growth or invasion of the tumor. Unlike biopsy, the preliminary imaging cannot distinguish benign from malignant disease.
Interfering factors
NURSING CARE
Pretest
During the test
Biopsy, bone marrow
Also called: Bone Marrow Aspiration
Includes: Genetic testing, bone marrow cells
Basics the nurse needs to know
The bone marrow is responsible for hematopoiesis—the formation of blood cells. The aspirated cells of the bone marrow are used to investigate hematologic disorders. A small sample of the cells is often representative of the whole marrow. Microscopic examination of the cells provides information about the cause, type, and extent of the abnormality. A peripheral blood smear is performed on the same day to compare and incorporate pertinent findings.
Leukocytes from the marrow have a number of different proteins attached to the cell surfaces. Many blood disorders have distinctive distributions and patterns of the proteins on these cell surfaces. In the presence of fluorescent antibodies, the different cellular proteins will react and bond with specific antibodies and the analysis of the cell patterns provides for many diagnoses. The proteins serve as markers to help diagnose different diseases, such as leukemia and lymphoma, and can distinguish between different types of each of these cancers (Jenkins, Karunanithi, & Hewamana, 2008).
How the test is done
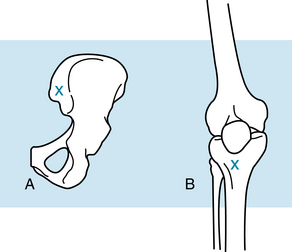
The aspiration and biopsy sites include the iliac crest and proximal tibia (Figure 20). In adults, the posterior iliac crest is the best site. In infants and young children, the proximal tibia is used. The sternal site is only used for obese patients.
Conscious sedation may be indicated for bone marrow biopsy, particularly for the children and adults who have undergone treatment for cancer. In the minimal residual disease monitoring process, the bone marrow biopsy sites are often multiple, with multiple specimens obtained.
Interfering factors
NURSING CARE
Pretest
During the test
Biopsy, breast
Includes: Estrogen receptor (ER), progesterone receptor (PR), HER-2/neu receptor
Basics the nurse needs to know
A suspicious, palpable or nonpalpable lesion of the breast requires a biopsy to determine the cause and differentiate between benign and malignant tissue. Imaging by ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) is done to visualize the size and location of the suspicious tissue. A core needle biopsy, or an open surgical biopsy are commonly used because of their high level of accuracy in obtaining a tissue sample. A fine needle aspiration biopsy may be used, but is not as accurate in obtaining a tissue sample.
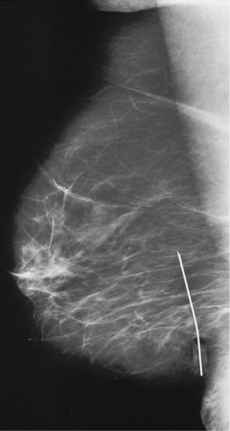
When the suspicious tumor or microcalcification is small and nonpalpable, the radiologist uses CT imaging to insert a clip as a tissue marker. This marker is left in place so that malignant tissue can be located for excision. Alternatively, a localizing needle wire can be placed directly into the tissue site or very close to it. The needle is then removed and the wire is left in place, held firm by a hook in the tip of the wire (Figure 21). The wire will provide additional guidance for the surgeon to locate the specific tissue to take a biopsy. Shortly after the wire is in place, the biopsy is performed.
Estrogen receptor (ER), progesterone receptor (PR), and HER-2/neu receptor
These tests are all tumor markers for breast cancer. These tests are done on the biopsy tissue when the biopsy result is invasive cancer of the breast. Estrogen receptor and progesterone receptor assay results provide information about prognosis and responsiveness to hormonal therapy, such as tamoxifen or aromatase therapy. Positive results for each of these tests can indicate that the tumor is highly likely to respond to hormonal therapy and a negative result means that the tumor is not likely to respond to this therapy. In recent testing advances, the patient with a positive ER-PR assay also can have genetic testing to identify a genetic variant that would prevent tamoxifen from being effective. If the patient is genetically resistant to tamoxifen, an alternative treatment with an aromatase inhibitor (anastrozole) would also act to inhibit the effect of estrogen on breast cancer.
Interfering factors
NURSING CARE
Pretest
During the test
Posttest
Biopsy, endomyocardial
How the test is done
The procedure involves a cardiac catheterization (see p. 221). A catheter with a jawlike tip is inserted under fluoroscopy or echocardiography, and several small tissue samples are obtained. Echocardiography is considered superior to fluoroscopy because of improved visualization of the tricuspid value. A right or left ventricular sample may be taken. For patients at high risk, such as those with a history of left ventricular thrombus or infarction, a right ventricular biopsy may be preferred.