Assessment: Using the Public Health Nursing Assessment Tool
Marie Truglio-Londrigan
Sandra B. Lewenson
|
The public health movement did not create the public health nurse, it found her at work in her district nursing the sick, watching over their families, and the neighborhood, and teaching in the homes those sanitary practices, those measures of personal and home hygiene, which do much to prevent disease and to promote health (Nutting, 1923/1991, p. 361).
LEARNING OBJECTIVES
At the completion of this chapter, the reader will be able to
Identify the importance of a public health nursing assessment.
Describe the components of the Public Health Nursing Assessment Tool.
Apply the Public Health Nursing Assessment Tool.
KEY TERMS
Assessment
Determinants of health
Disparities
General health status
Health-related quality of life and well-being
Minnesota Department of Health Population-Based Public Health Nursing Practice Intervention Wheel Strategies
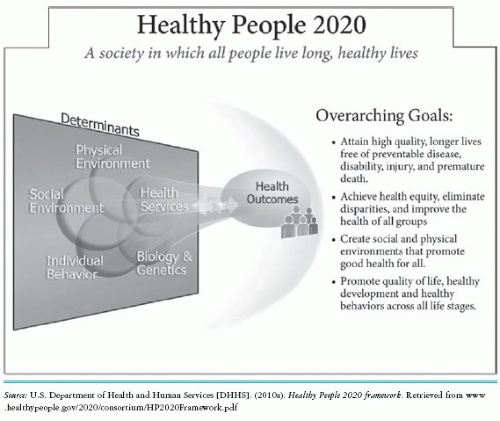
Assessment supports decision making in health care by providing information about the health of the individual, family, community, system, and population. Shuster and Goeppinger (2008) state that “community assessment is one of the three core functions of public health nursing and is the process of critically thinking about the community” (p. 351). Public health nurses recognize that communities in which the individual, family, system, or population reside influence the health and well-being of all stakeholders. Likewise, the individual, family, system, and population affect the health of the community and each other. An assessment tool guides the public health nurse through the process of discovery. This chapter presents the Public Health Nursing Assessment Tool (PHNAT), designed by Lewenson and Truglio-Londrigan, which uses the concepts found in Healthy People 2020 (Figure 3-1) and the Minnesota Department of Health Population-Based Public Health Nursing
Practice Intervention Wheel Strategies as its organizing framework. Specifically, the PHNAT uses the four foundation health measures that serve as indicators of progress toward achieving the goals of Healthy People 2020. These indicators include general health status, health-related quality of life and well-being, determinants of health, and disparities (U.S. Department of Health and Human Services {DHHS}, 2010b, para. 4p). Using the four foundation health measures helps the public health nurse determine the priority needs of the community and then develop, implement, and evaluate a plan using the intervention wheel strategies as a guide. The PHNAT also asks the public health nurse to reflect on the experience of doing a public health nursing assessment. Box 3-1 provides an outline of the organization of the PHNAT; it does not include all the detail that is found in the PHNAT, but rather provides a quick schematic.
Practice Intervention Wheel Strategies as its organizing framework. Specifically, the PHNAT uses the four foundation health measures that serve as indicators of progress toward achieving the goals of Healthy People 2020. These indicators include general health status, health-related quality of life and well-being, determinants of health, and disparities (U.S. Department of Health and Human Services {DHHS}, 2010b, para. 4p). Using the four foundation health measures helps the public health nurse determine the priority needs of the community and then develop, implement, and evaluate a plan using the intervention wheel strategies as a guide. The PHNAT also asks the public health nurse to reflect on the experience of doing a public health nursing assessment. Box 3-1 provides an outline of the organization of the PHNAT; it does not include all the detail that is found in the PHNAT, but rather provides a quick schematic.
Overview of the Unique Qualities of the PHNAT
The PHNAT offers a kaleidoscopic way to view the process of assessment. The authors see this kaleidoscopic capability as essential to public health nurses’ practice as they work with a wide spectrum of clients. In the public health nurse’s practice, clients include individuals, families, communities, systems, and populations. Therefore, a tool that permits the public health nurse to focus on each of these types of clients must be flexible. The PHNAT permits the public health nurse to assess the individual as well as simultaneously assess the community, population, and system, and this flexibility permits the public health nurse to shift his or her view back and forth depending on the area of focus and the priority needs at that moment in time. The authors developed the PHNAT using the Process Model for Healthy People 2020: Improving Health of Americans (Process Model) as a guide. It is located on the inside front cover of this text, and facilitates this shifting back and forth.
Box 3-1 PUBLIC HEALTH NURSING ASSESSMENT TOOL (PHNAT)
Schematic
Section I: Four Foundational Health Measures
Section I Part 1: Foundational Health Measures General Health Status (Certain aspects of this portion of the PHNAT may be directed toward the individual/family.)
A-1 Individual and Family
B-1 Population: Vital Statistics
B-2 Population: Mortality
B-3 Population: Morbidity
B-4 Population: Life Expectancy (with international comparisons)
B-5 Population: Healthy Life Expectancy
B-6 Population: Years of Potential Life Lost (YPLL) (with international comparisons)
B-7 Population: Physically and Mentally Unhealthy Days
Section I Part 2: Foundational Health Measures Health-Related Quality of Life and Well-Being (Individual/family assessment)
A-1 Individual and Family
Section I Part 3: Foundational Health Measures Determinants of Health
Part 3-1 Biology and Genetics
A-1 Individual and Family Assessment
B-1 Population Assessment
B-2 Population: Age Distribution
B-3 Population: Race Distribution
B-4 Population: Gender Distribution
Part 3-2 Social Factors
A-1 Social Determinants: Housing Conditions
A-2 Social Determinants: Transportation
A-3 Social Determinants: Workplace
A-4 Social Determinants: Recreational Facilities
A-5 Social Determinants: Educational Facilities
A-6 Social Determinants: Places of Worship
A-7 Social Determinants: Social Services
A-8 Social Determinants: Library Services
A-9 Social Determinants: Law Enforcement
A-10 Social Determinants: Fire Department
A-11 Social Determinants: Communication
A-12 Social Determinants: Employment Distribution
A-13 Social Determinants: Leading Industries in Community
A-14 Social Determinants: Educational Level of People Older Than 25 Years
A-15 Social Determinants: Family Income
Section I Part 3-2: Physical Determinants
B-1 Physical Determinants: History of the Community
B-2 Physical Determinants: Windshield Survey
B-3 Physical Determinants: The Built Environment
B-4 Physical Determinants: Natural Environment
B-5 Physical Determinants: Physical Barriers/Boundaries
B-6 Physical Determinants: Environmental/Sanitation/Toxic Substances
Section I Part 3-3: Health Services
A. Types of Services
A-1 Acute Care
A-2 Home Care
A-3 Primary Care
A-4 Long Term Care
A-5 Rehabilitative
A-6 Assistive Living
A-7 Mental Health Services
A-8 Occupational
A-9 School Health Programs
A-10 Dental
A-11 Palliative
Section I Part 3-3: Access to Care
B-1 Access to Care: Using the Seven A’s
Section I Part 3-4: Policymaking
A-1 Local, State, and Federal Organizational Structure of Community
A-2 Political Issues in the Community
A-3 Health Policies
Section I Part 3-5: Behavior
A. Individual (choices for healthy living: exercise, stress reduction activities, sleep and rest, healthy diet, etc.)
B. Population (participation in town weight loss programs or exercise programs)
Section I Part 4: Foundational Health Care Disparities Assessment: Frequently takes place after the collection of data, during the analysis located in Part II of this document. The public health nurse, along with partners, may note disparities from their direct observations of the environment as well as noting disparities within data collected in all of the previous sections of this document. For example, 5-year cancer survival rate differences between races.
Section II: Analysis of Health Status
Section III: Prioritize Public Health Issues
Section IV: Plan and Implementation Using Minnesota Intervention Wheel Strategies
Section V: Tracking and Evaluation Section
Section VI: Reflection
Source: Public health nursing: Applying and doing. Sandra B. Lewenson and Marie Truglio-Londrigan. Adapted from U.S. Department of Health and Human Services. (2010a). Healthy People 2020 framework. Retrieved from www.healthypeople .gov/2020/about/default.aspx
The PHNAT is embedded in and guides the user throughout the Mobilize, Assess, Plan, Implement, and Track (MAPIT) process discussed in Chapter 1, including the mobilization of partners who work together toward ensuring the health of the public. These partners participate in the assessment data gathering, analysis, planning, implementation, tracking of data, evaluation, and reflection. A visualization of the MAPIT process is also presented in the Process Model. Each part of the tool includes space for responses to questions, tables where data can be organized, and definitions for each of the foundational measures. The PHNAT prompts the user to analyze and reference the data collected. As the user becomes more familiar with the PHNAT, additional information and data may be sought, new tables formed, and original ones revised, depending on the needs of the user. For example, if the user wants to compare the findings with national or global data, he or she can do so. An online version of the PHNAT further facilitates the use of this tool because it can be more easily manipulated and implemented. The comprehensiveness of the PHNAT also suggests that the completion of a public health nursing assessment would lend itself to group work in a course or in the practice setting.
The Internet provides a wealth of data that can be incorporated into the study. Information such as geography and history of a community, as well as census track boundaries and data, can also be found on the Internet and facilitates the assessment of the community. Online databases, such as those found in Box 3-2, are examples of important resources the public health nurse can use when completing the PHNAT. The data needed for many of the suggested tables on the PHNAT can be found through the Internet and the various electronic databases. The public health nurse should be sure to select reliable and valid sources on the Internet by taking the time to search sites to see what types of information they offer. When public health nurses come across other sites and resources, they can share them with their colleagues.
Box 3-2 POTENTIAL DATABASES FOR DATA COLLECTION
http://www.census.gov
http://www.fedstats.gov
http://cdc.gov/nchs
http://health.gov/nhic
http://www.cdc.gov/BRFSS/
http://seer.cancer.gov/
http://www.cdc.gov/nchs/ahcd.htm
http://www.cdc.gov/nchs/nhanes.htm
The various parts of the PHNAT can be completed in any sequence. This flexibility permits the group to work on this tool and collect the data simultaneously. Assessment is not a linear process and allows for the public health nurse to complete the process based on expediency, interest, time, and efficiency.
The PHNAT can be used by faculty to teach graduate and undergraduate nursing students. It is also meant to be used by public health nurses who work in all types of community settings such as home care, visiting nurse service, health departments, neighborhood health centers, schools, and industry. Because the PHNAT encourages mobilization and collaboration within a community, this tool can be shared and used by others in the community. The ethics of public health practice warrant that public health nurses who collect data be mindful and respectful of those they are assessing— for example, students assessing a community must schedule appointments with the various stakeholders rather than showing up unannounced. They also should carry identification and a letter of introduction from their school in some instances. Just as an assessment is never a static process, neither is the PHNAT a final product.
PHNAT Four Foundational Health Measures
General health status is one of the four foundational health measures. It refers to data that inform the public health nurse and partners in the health initiative about the health of the population and includes information located in Box 3-1 (U.S. DHHS, 2010c). It is important to note that some of this information is not population-focused, such as self-assessed health status; however, this is an example of how public health nurses serve individuals in the community as well as the general population.
Another foundational health measure is health-related quality of life. Health-related quality of life is a complex concept and focuses on “the impact health status has on quality of life” (U.S. DHHS, 2010d). This portion of the PHNAT also focuses on the individual and again sheds light on those public health nurses who do practice on a one-to-one basis with clients in the community. The particular areas included in this portion of the tool are (1) patient-reported outcomes measurement information system (PROMIS) tools to measure health outcomes from a patient perspective, (2) well-being measures, and (3) participation measures that also reflect an individual’s perception of his or her health or ability to participate in and interact with the environment (U.S. DHHS, 2010d).
A major portion of the PHNAT includes the determinants of health. In this section the public health nurse collects information pertaining to those factors that determine the health of the individual, family, and the population living in a community. The health determinants that organize this section include biology and genetics, social factors, health services, policymaking, and individual behavior (U.S. DHHS, 2010e).
Biology and Genetics
The determinant of health under biology and genetics may include data that are individual/family-focused or population-focused. The public health nurse gathers the information on the individual and family with whatever health assessment tool he or she uses in the particular academic or clinical setting. Pertaining to the population, aggregate data such as age, race, and gender are important. Box 3-1 offers a comprehensive view of the type of information that needs to be collected. In addition, the databases listed in Box 3-2 help the public health nurse complete this section.
Examples of the types of questions the public health nurse may ask that are representative of this kaleidoscopic view include:
Who is the client/family?
What is the health of the client/family?
What are the client’s/family’s health behavior and choices?
Do these choices support health and a healthy lifestyle?
What are the resources in the community that facilitate health?
Does the client/family have access to these resources?
What part of the population does the client/family represent?
What is the status of health for this population?
Who makes up this population?
What do the aggregate data tell about this population?
Is this family’s particular issue reflected in the population as well?
Social Factors
Social factors, the next determinant of health to be considered, include social determinants of health and physical determinants or conditions in the environment (U.S. DHHS, 2010f). Social factors that the public health nurse assesses include the client’s interactions and connections with family, friends, and others in the community. These interactions are important for positive health outcomes in individuals/families and a population. Social support is the type of supportive behavior offered to an individual/family or population by another person, family, or agency/organization. The support may be emotional, instrumental as in services provided, informational such as knowledge, and appraisal such as feedback (House, 1981). Social supports may be offered informally, as in the type of support offered to an individual by a family member or a friend, or they may be more formal, as in the support offered by an agency such as Meals On Wheels. The social assessment section of the PHNAT, as shown in Box 3-1, asks for information about formal and informal support systems in the community. Some of the areas that the public health nurse assesses include housing, transportation, work, recreation, education, places of worship, health care, social services, library services, law enforcement, fire protection, and communication services (U.S. DHHS, 2010f). As public health nurses assess these areas, they must pay careful attention to the Seven A’s (Krout, 1986; Truglio-Londrigan & Gallagher, 2003; Williams, Ebrite, & Redford, 1991), which are discussed later in this chapter.
The second part of social factors includes physical determinants. The public health nurse must assess the physical environment of the community-at-large. The physical environmental factor informs the public health nurse about the health of the community and the population that resides in that community. Generally speaking, the physical environment is represented by that which can be seen, touched,
heard, smelled, and tasted. However, the physical environment also contains less tangible elements, things such as radiation and ozone. The physical environment can harm individual and community health, especially when individuals and communities are exposed to toxic substances; irritants; infectious agents; and physical hazards in homes, schools, and work sites. The physical environment also can promote good health, for example, by providing clean and safe places for people to work, exercise, and play (U.S. DHHS, 2000, p. 19).
heard, smelled, and tasted. However, the physical environment also contains less tangible elements, things such as radiation and ozone. The physical environment can harm individual and community health, especially when individuals and communities are exposed to toxic substances; irritants; infectious agents; and physical hazards in homes, schools, and work sites. The physical environment also can promote good health, for example, by providing clean and safe places for people to work, exercise, and play (U.S. DHHS, 2000, p. 19).
In Healthy People 2020, a limited definition is offered with an extensive list of physical environment examples that can be used throughout the PHNAT. Collecting assessment data on the physical environment includes what is often referred to as a “windshield survey” (Anderson & McFarlane, 1988; Stanhope & Lancaster, 2008). The windshield survey reflects what one can view from a car window as one drives through a community and contains observations of various components of the community such as housing, open spaces, transportation, race, ethnicity, restaurants, and stores. In urban areas where the use of cars is limited, walking through the community yields similar results. As public health nurses walk or drive through a community, they assess the physical environment using their five senses (Matteson, 1995). Are there trees, flowers, blue sky, trash, cracked asphalt, smokestacks, or garbage? Can birds, dogs, rain, car horns, screams, or traffic be heard? Can nurses smell flowers, grass, gas, or sewerage? And, finally, what tastes abound? In other words: Is the environment clean and safe for the people or are there hidden dangers such as radiation, ozone, carbon monoxide, and lead in their homes? The PHNAT asks the public health nurse to identify the boundaries of the community, the physical characteristics in relation to topography and terrain, the history of the community, sanitation services such as garbage pickup and recycling, and environmental programs that protect air, food, water, and provide animal and vector control. Here the public health nurse can obtain the data by using the Internet and electronic databases, by walking or driving through a community, or by interviewing members of the community.
HEALTH SERVICES
The determinant of health known as health services is more than a listing of the physical, social, and mental health programs offered to individuals/families or populations in a particular community (see Box 3-1). It also includes an assessment of access to these services. This access to quality care is an important part of the PHNAT. Most community- or populationbased assessment tools request an assessment of health service organizations; however, the inclusion of access to care using the Seven A’s is unique to the PHNAT. The Seven A’s address more than the single concept of access. Whether or not there is access frequently depends on the additional factors of awareness, availability, affordability, acceptability, appropriateness, and adequacy of the service. It is essential for the public health nurse to assess and analyze each of these for whether individuals or populations can gain access to essential services that influence their health and well-being (Krout, 1986; Truglio-Londrigan & Gallagher, 2003; Williams et al., 1991).
The following Seven A’s questions can assist the public health nurse in analyzing his or her findings:
Is the population aware of its needs and the services of the community?
Can the population gain access to the services that it needs?
Is the service available and convenient to the population in terms of time, location, and place for use?
How affordable is the service for the population in question?
Is the service acceptable to the population in terms of choice, satisfaction, and cultural congruence?
How appropriate is the service for the specific population, or is there a fit?
Is the service adequate in terms of quantity or degree?
Policymaking
The public health nurse must also assess the policies that influence the health of the individual, family, community, system, and population under study. Examples include policies on seat belt use, helmet use, phone use and texting while driving, smoking, and child car seats. Each of these policies has had a positive influence on the health and well-being of individuals and the population at large, resulting in a decrease in disabilities and injuries. The public health nurse must be knowledgeable about how his or her community functions with regard to the political infrastructure, and as such must assess this infrastructure to be familiar with how it works: who are the formal and informal political leaders? How can they be reached? What initiatives have they supported in the past? What are the laws that affect the individual/family, population, and community with regard to the public’s health? Are these laws upheld? Are there issues that have not been addressed, and, if so, what can be done to address these issues? The data collected in this section include the organizational structure of the community, a description of the political issues in the community, and an identification of some of the public health laws that affect the community and its members’ health. As the public health nurse conducts this portion of the assessment, it is important to explore what the local newspapers report, to meet with the local government, and to check out the school boards or any of the governing bodies in the area. Meet the candidates if it is an election year and listen to what the community is saying. Check websites, social networking sites, and local blogs. Using the Internet, here and throughout the PHNAT, assists the public health nurse in obtaining the necessary data and learning about the community.
Behavior (Individual and Population)
The data to be collected in this section of the PHNAT are the behaviors of individuals and families; however, population behavior may also be observed. The type of behavior an individual or population exhibits affects health— an individual who chooses to smoke cigarettes may have a different set of health outcomes compared to an individual who chooses not to smoke cigarettes. In recent years, there have also been examples of population-based behavior; for example, towns have gathered and participated in a collective great smoke-out or weight loss program. The public health nurse collects data on the individual and family that reflect their behavior and again turns the kaleidoscope to look outward to the community and population within that community. Some of the questions that provide insight into individual or population-based behavior are as follows:
What does the assessment of the client tell about his or her behavior?
What types of choices does he or she make with regard to diet, physical activity, alcohol, cigarette smoking or other drug use, and so forth?
How does the family support health choices?
How does the community support health choices?
Have there been community-driven health promotion initiatives, like weight loss or physical activity programs such as a walk to school program?
Disparities is the fourth and final foundational health measure. According to Healthy People 2020, “If a health outcome is seen in a greater or lesser extent between populations, there is disparity. Race or ethnicity, sex, sexual identity, age, disability, socioeconomic status, and geographic location all contribute to an individual’s ability to achieve good health” (U.S. DHHS, 2010g, para. 1). Frequently, the public health nurse will note disparities as he or she makes observations within the community and analyzes the data that are being gathered. Hence, for this foundational health measure much of the information needed is gathered throughout the PHNAT.
Analysis of Health
The public health nurse, along with other partnering members of a health initiative, analyzes the information gathered during the assessment process. Many times the public health nurse will examine past data to see whether trends and patterns have emerged over time. This process of analysis takes time and reflection. The key here is that the public health nurse does not do this alone but takes part in a partnership. This process identifies issues in a community and sets priorities.
Prioritize Public Health Issues
Once the public health nurse and partners conduct the assessment, an analysis of the data elucidates which priority public health issues exist in the community. In determining the priority health issues, the public health nurse, using a population-based focus, collaborates with other public health practitioners, key informants in the community, and any organization or agency that may have a voice with regard to the population and public health issue. In population-based care, partnerships form the necessary bonds to make sustainable changes necessary for health in the particular targeted population. Those involved in the partnership work together to form a common understanding of the issue. All involved, including the population of interest residing in the community, agree on the priority issue identified; this is essential for a positive outcome. Once the priority is noted, the partners confer with the Healthy People 2020 topic areas and corresponding objectives for guidance in creating and implementing a plan to address the issue (U.S. DHHS, 2010h).
Plan and Implementation: Applying the Minnesota Intervention Wheel Strategies
In this section of the PHNAT, the public health nurse, along with any members of the partnership, develops a plan of action using the intervention wheel strategies. Again, working with members of the partnering organizations as well as other stakeholders is critical, because partnering is more likely to ensure a plan that is congruent with cultural ideas, values, and beliefs. It is also important to engage in reviews to determine a plan that is based in best practice. The PHNAT involves the application of the intervention wheel, which identifies 17 nursing interventions applied to three levels of practice: individual/family, community, and system. The intervention wheel began in
the mid-1990s as part of a “grounded theory process carried out by the public health nurse consultants at the Minnesota Department of Health” (Keller, Strohschein, & Briske, 2008, p. 189). Questioning the contribution public health nurses made in population-based care, the consultants held a series of workshops that informed them of the work of public health nurses. Using a systematic, evidenced-based review of the literature, they analyzed the input of public health nurses who worked in a variety of community settings. This enabled the consultants to construct the wheel graph depicting the 17 intervention strategies applied to the three levels of practice (Stanhope & Lancaster, 2008). The intervention strategies visually depicted and color coded on the wheel are case finding, surveillance, disease and health event investigation, outreach, screening, referral and follow-up, case management, delegated functions, health teaching, counseling, consultation, collaboration, coalition building, community organizing, advocacy, social marketing, and policy development and enforcement. The intervention wheel was “conceived as a common language or catalog of general actions used by public health nurses across all practice settings” (Keller et al., 2008, p. 193).
the mid-1990s as part of a “grounded theory process carried out by the public health nurse consultants at the Minnesota Department of Health” (Keller, Strohschein, & Briske, 2008, p. 189). Questioning the contribution public health nurses made in population-based care, the consultants held a series of workshops that informed them of the work of public health nurses. Using a systematic, evidenced-based review of the literature, they analyzed the input of public health nurses who worked in a variety of community settings. This enabled the consultants to construct the wheel graph depicting the 17 intervention strategies applied to the three levels of practice (Stanhope & Lancaster, 2008). The intervention strategies visually depicted and color coded on the wheel are case finding, surveillance, disease and health event investigation, outreach, screening, referral and follow-up, case management, delegated functions, health teaching, counseling, consultation, collaboration, coalition building, community organizing, advocacy, social marketing, and policy development and enforcement. The intervention wheel was “conceived as a common language or catalog of general actions used by public health nurses across all practice settings” (Keller et al., 2008, p. 193).
For the purposes of this text, these intervention strategies have been separated out into five themes addressed in specific intervention chapters:
Hitting the pavement includes the strategies of case finding, surveillance, disease and health event investigation, outreach, and screening.
Running the show includes the strategies of referral and follow-up, case management, and delegated functions.
Working it out includes the strategies of health teaching, counseling, and consultation.
Working together includes the interventions of collaboration, coalition building, and community organizing.
Getting the word out includes the interventions of advocacy, social marketing, and policy development and enforcement.
These intervention chapters focus on each of the themes noted above by using case study examples from public health nurses who use the intervention wheel strategies to address public health problems experienced by individuals, families, and populations within their communities. The reader can refer to these chapters when using the PHNAT.
Overall, when selecting the intervention strategy and developing a plan of action, the public health nurse works in concert with others in the community and considers the following:
The population to be targeted for the plan
Short-term goal(s), long-term goal(s)
Community resources, including human, financial, time, technology, and educational resources
Financing of the implementation and evaluation of the plan
Evidence that supports the intervention for this population
Evidence that the strategy is culturally appropriate
Evidence that the Seven A’s are accounted for
Best place to implement the strategy
Best person to implement the strategy
How to evaluate whether or not the outcomes are met
Tracking and Evaluation
Tracking and evaluation are critical to the entire Process Model outlined on the inside front cover of this text and noted as the last part of the MAPIT process. While the partnership is
determining what the plan will be and how the plan will be implemented, it is also important for them to determine what type of information will be collected, where it will be collected, who will collect it, where it will be stored, what kind of technology will be used, how it will be collected, and what type of resources will be needed. This is important for tracking so that the public health nurse and partners may determine if progress is being made in meeting objectives. If it is determined that there is progress, the public health nurse and partners will need to decide if the same plan and course of action will be sustained. If there are questions about the progress, changes may need to be initiated. This tracking of information and evaluation feed back to all levels of the Process Model. Over time, analysis of the data may inform the public health nurse and the members of the partnership that the vision or goals may need to change, or the partners may determine that the plan is not based in evidence or is not culturally congruent or that one or more of the Seven A’s is not met and that these are the reasons for the weak outcomes. The tracking of data and evaluation, although at the bottom of the model, are important and inform every part of the Process Model. In 2010, the Institute of Medicine (IOM) published a report, For the Public’s Health: The Role of Measurement in Action and Accountability, which speaks to some of the issues related to tracking and evaluation. Some of the interesting and complex questions raised include: How do we measure our progress as a nation in our movement toward a healthier America? What measurement approaches can we implement that will help us evaluate and critique agencies’/partnership’s health initiatives with regard to population-based health outcomes? What are the best ways to gather and analyze data with a focus on all of the foundational health measures? So much time, energy, and resources are spent in partnership development, assessment, prioritizing of issues, planning, and in the implementation of health initiatives; tracking and evaluation are critical to all of these processes in that they bring us back to the three core functions of public health: assessment, policy development, and assurance.
determining what the plan will be and how the plan will be implemented, it is also important for them to determine what type of information will be collected, where it will be collected, who will collect it, where it will be stored, what kind of technology will be used, how it will be collected, and what type of resources will be needed. This is important for tracking so that the public health nurse and partners may determine if progress is being made in meeting objectives. If it is determined that there is progress, the public health nurse and partners will need to decide if the same plan and course of action will be sustained. If there are questions about the progress, changes may need to be initiated. This tracking of information and evaluation feed back to all levels of the Process Model. Over time, analysis of the data may inform the public health nurse and the members of the partnership that the vision or goals may need to change, or the partners may determine that the plan is not based in evidence or is not culturally congruent or that one or more of the Seven A’s is not met and that these are the reasons for the weak outcomes. The tracking of data and evaluation, although at the bottom of the model, are important and inform every part of the Process Model. In 2010, the Institute of Medicine (IOM) published a report, For the Public’s Health: The Role of Measurement in Action and Accountability, which speaks to some of the issues related to tracking and evaluation. Some of the interesting and complex questions raised include: How do we measure our progress as a nation in our movement toward a healthier America? What measurement approaches can we implement that will help us evaluate and critique agencies’/partnership’s health initiatives with regard to population-based health outcomes? What are the best ways to gather and analyze data with a focus on all of the foundational health measures? So much time, energy, and resources are spent in partnership development, assessment, prioritizing of issues, planning, and in the implementation of health initiatives; tracking and evaluation are critical to all of these processes in that they bring us back to the three core functions of public health: assessment, policy development, and assurance.
Reflection
This final section of the PHNAT reminds the public health nurse to be reflective in his or her practice. Self-reflection aids in the decisionmaking process (Truglio-Londrigan & Lewenson, 2008) and causes the public health nurse to be vigilant during the assessment process and in the implementation of any plans. Questions that the public health nurse may ask include: What am I observing? What am I hearing? Am I seeing and hearing all that needs to be seen and heard? What am I missing? What feelings am I experiencing during this assessment process? Are these feelings facilitating this assessment or creating a barrier to the assessment? Are these feelings hindering the development of the partnership and the development of trust? Am I engaging in activities that help in mobilizing the community of interest?
The table in this reflection section asks the public health nurse to keep a record of the experience. The public health nurse can use this table to record when he or she worked on the assessment and how he or she responded to the various parts of the assessment, reflect on the group experience if the assessment was conducted in a group, or record any personal or professional reflection observed during the assessment process.
Conclusion
This chapter explains how to conduct a public health nursing assessment using the author-designed PHNAT. The unique qualities of the PHNAT include the use of the U.S. DHHS (2010a,b,c,d,e,f,g,h) foundational health measures including general health status, health-related quality of life and well-being, determinants of health, and disparities; application of the intervention wheel strategies; and self-reflection. The application of the PHNAT provides the public health nurse with the information that needs to be analyzed and ultimately determines the priority healthcare issues for a specific population within a community. To carry out the assessment, the public health nurse uses a variety of methods to obtain the data, including observation, interviews, Internet research, census tracks, government reports, newspaper accounts, and evidence of best practice. The public health nurse collaborates with other public health practitioners, key informants in the community, and other agencies to determine the priority. Once this priority is identified, the public health nurse works toward the development and implementation of a culturally congruent initiative based in evidence. The tracking evaluation of the initiative is part of the plan, as is the reflective piece by the public health nurse. Both the outcomes of the evaluation and the reflections provide rich feedback to the community and the public health nurse as he or she continues the ongoing assessment process.
References
Anderson, E. T., & McFarlane, J. (Eds.). (1988). Community as client: Application of the nursing process. Philadelphia, PA: Lippincott.
House, J. S. (1981). Work stress and social support. Reading, MA: Addison-Wesley.
Institute of Medicine (IOM). (2010). For the public’s health: The role of measurement in action and accountability. Washington, DC: National Academies Press.
Keller, L. O., Strohschein, S., & Briske, L. (2008). Population-based public health nursing practice: The intervention wheel. In M. Stanhope & J. Lancaster (Eds.), Public health nursing: Population-centered health care in the community (7th ed., pp. 186-214). St. Louis, MO: Mosby Elsevier.
Krout, J. A. (1986). The aged in rural America. Westport, CT: Greenwood.
Matteson, P. S. (1995). Teaching nursing in the neighbor-hoods: The Northeastern University Model. New York, NY: Springer.
Nutting, A. (1923/1991). Thirty years of progress in nursing. In N. Birnbach & S. B. Lewenson (Eds.), First words: Selected addresses from the National League for Nursing 1894-1933 (pp. 358-369). New York, NY: National League for Nursing Press.
Shuster, G. F., & Goeppinger, J. (2008). Community as client: Assessment and analysis. In M. Stanhope & J. Lancaster (Eds.), Public health nursing: Population-centered health care in the community (7th ed., pp. 339-372). St. Louis, MO: Mosby Elsevier.
Stanhope, M., & Lancaster, J. (Eds.). (2008). Public health nursing: Population-centered health care in the community (7th ed.). St. Louis, MO: Mosby Elsevier.
Truglio-Londrigan, M., & Gallagher, L. (2003). Using the Seven A’s to determine older adults’ community resource needs. Home Healthcare Nurse, 21(12), 827-831.
Truglio-Londrigan, M., & Lewenson, S. B. (2008). Know yourself: Reflective decisionmaking. In S. B. Lewenson & M. Truglio-Londrigan (Eds.), Decision-making for nurses: Thoughtful approaches to practice (pp. 1-11). Sudbury, MA: Jones and Bartlett.
U.S. Department of Health and Human Services. (2000). Healthy people 2010 (Vol. 1). Washington, DC: U.S. Government Printing Office.
U.S. Department of Health and Human Services. (2010a). Healthy people 2020 framework. Retrieved from http://www.healthypeople.gov/2020/Consortium /HP2020Framework.pdf
U.S. Department of Health and Human Services. (2010b). About healthy people. Retrieved from http://www.healthypeople.gov/2020/about/default.aspx
U.S. Department of Health and Human Services. (2010c). General health status. Retrieved from http://www .healthypeople.gov/2020/about/GenHealthAbout.aspx
U.S. Department of Health and Human Services. (2010d). Health-related quality of life. Retrieved from http://www.healthypeople.gov/2020/about/QoLWBabout.aspx
U.S. Department of Health and Human Services. (2010e). Determinants of health. Retrieved from http://www .healthypeople.gov/2020/about/DOHAbout.aspx
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree