Assessment of the baby
Capillary sampling
Learning outcomes
Having read this chapter, the reader should be able to:
This chapter considers capillary blood sampling from the baby. Obtaining blood samples from the neonate via a heel prick remains a simple, generally effective method. The midwife undertakes this as part of routine national screening in the UK, and also to detect or confirm deviations from the norm (e.g. serum bilirubin or serum glucose estimations).
Underpinning anatomy
For a heel prick blood test the blood is obtained from the capillaries contained within the skin. The arterial–venous network of the skin is located at the junction of the lower dermis and upper subcutaneous tissue. The skin should be punctured only to the depth of this junction to facilitate blood flow; a deeper puncture can have serious complications. If the calcaneus (heel bone) is punctured, there is a risk of osteochondritis or osteomyelitis. The distance between the skin and bone can vary depending on where on the foot the measurement is taken (with the narrowest distance being at the posterior curve of the heel) and the weight and gestation of the baby.
Another consideration is the position of plantar arteries and nerves, which should be avoided. Puncturing the arteries can result in haemorrhage and increases the risk of introducing infection, which could result in septicaemia. Puncturing the nerves can result in permanent damage to the nerve.
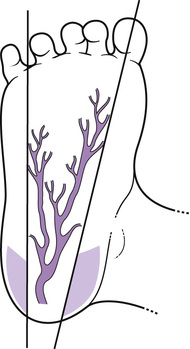
Blumenfeld et al (1979) estimated the distance from the surface of the skin to the arterial–venous network to be 0.35–1.6 mm (post-mortem). Jain & Rutter (1999) attempted to replicate this work with live babies and argue that none of the babies in their study had a distance of less than 3 mm between capillaries and skin, and thus argue that any part of the plantar surface would be suitable for pricking. However, for NBS the guidelines are clear that for a single test the sites shaded in Figure 39.1 should be used (described below), with a maximum puncture depth of 2 mm. For repeated testing the plantar surface of the whole heel may be considered but to a maximum puncture depth of 1 mm. Automated lancets vary in their puncture depth but often the greatest is 2.4 mm. Using something other than an automated device is forbidden; it is highly likely that puncture depth will be in excess of the maximum permitted.
Guidelines for site selection
• Use the lateral and medial portions of the heel (plantar surface) as puncture sites (UKNSPC 2012).
• Draw an imaginary line from midway between the fourth and fifth toes laterally and medially from the middle of the big toe as the calcaneus rarely extends beyond these (Fig. 39.1) (these points are also furthest away from the arteries and nerves). Puncture the skin on the sole of the heel, not on the side or back of the heel.
• Select a new puncture site not previously punctured and free from bruising, for each collection.
Repeated heel pricks can also make the localized skin sore or infected and the baby is also exposed to a repeatedly painful procedure (discussed below). A consistently good sampling technique reduces the risks for the baby and limits the number of negative experiences. The midwife and parents can be confident that the result is not influenced by a poor sampling technique. If repeated sampling is required some other form of venous access, e.g. peripheral cannula, may be considered as an alternative.
Newborn blood spot screening (NBS)
NBS is offered to all babies in the UK and should be taken between 5 and 8 days after birth (day of birth being day 0), ideally on day 5 (this may vary internationally). Screening at this age is recommended in order to instigate diagnosis/treatment as early as possible. Currently five different disorders are screened from these blood spots:
In 2015 a further four rare conditions were added to the list: maple syrup urine disease, isovaleric acidaemia, glutaric aciduria, and homocystinuria. The reader is encouraged to remain up to date with constantly evolving testing schedules.
The blood spot form is accompanied by its own glassine envelope. A type of blotting paper is used for the drops of blood; this allows the blood to soak through to the required depth for accurate testing. There are four circles, each one needs to have one drop of blood in it, that fills the circle fully. Three percent of tests per year (20,000 babies) need repeating because of poor sampling or incorrect documentation. Inaccurate results may be obtained if the blood:
• is multi-spotted (several smaller drops fill the circle)
• has been forced out of the heel by squeezing
Repeat tests are requested if:
• a specific condition, e.g. cystic fibrosis, requires it
• the test was taken before 4 days of age
• the specimen card has errors or omissions
• the test was taken less than 72 hours after transfusion of a blood product
• it is an insufficient or contaminated sample
• if there has been a delay in it reaching the laboratory (UKNSPC 2012). All specimens should be posted first class immediately.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree