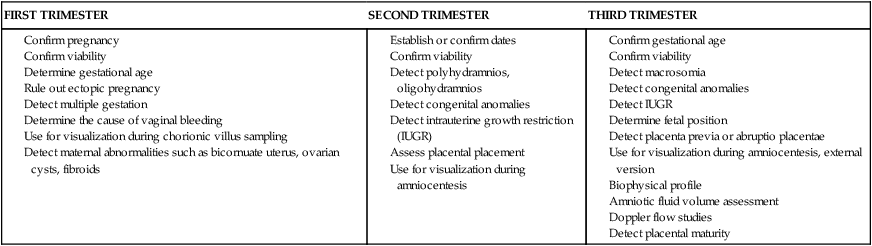
• Explore the biophysical, psychosocial, sociodemographic, and environmental aspects of high risk pregnancy. • Examine risk factors identified through history, physical examination, and diagnostic techniques. • Differentiate among diagnostic techniques, including when they are used in pregnancy and for what purposes. • Develop a teaching plan to explain diagnostic techniques and implications of findings to patients and their families. chorionic villus sampling (CVS) Removal of fetal tissue from the placenta for genetic diagnostic studies percutaneous umbilical blood sampling (PUBS) (also called cordocentesis) Procedure during which a fetal umbilical vessel is accessed for blood sampling or for transfusions In the past, risk factors were evaluated only from a medical standpoint; therefore only adverse medical, obstetric, or physiologic conditions were considered to place the woman at risk. Today, a more comprehensive approach to high risk pregnancy is used, and the factors associated with high risk childbearing are grouped into broad categories based on threats to health and pregnancy outcome. Categories of risk are biophysical, psychosocial, sociodemographic, and environmental (Gilbert, E.S., 2007) (Box 19-1). Risk factors are interrelated and cumulative in their effects. Biophysical risks include factors that originate within the mother or fetus and affect the development or functioning of either one or both. Examples include genetic disorders, nutritional and general health status, and medical or obstetric-related illnesses. Box 19-2 lists common risk factors for several pregnancy-related problems. Sociodemographic risks arise from the mother and her family. These risks may place the mother and fetus at risk. Examples include lack of prenatal care, low income, marital status, and ethnicity (see Box 19-1). Environmental factors include hazards in the workplace and the woman’s general environment and may include environmental chemicals (e.g., pesticides, lead, mercury), radiation, and pollutants (Silbergeld & Patrick, 2005). The major expected outcome of all antepartum testing is the detection of potential fetal compromise. Ideally, the technique used identifies fetal compromise before intrauterine asphyxia occurs so that the health care provider can take measures to prevent or minimize adverse perinatal outcomes. Antepartum testing is used primarily in patients at risk for disrupted fetal oxygenation. In most cases, monitoring begins by 32 to 34 weeks of gestation and continues regularly until birth. Assessment tests should be selected based on their effectiveness, and the results must be interpreted in light of the complete clinical picture. Box 19-3 lists common maternal and fetal indications for antepartum testing that are supported by currently available evidence (Miller, Miller, & Tucker, 2013). Assessment of fetal activity by the mother is a simple yet valuable method for monitoring the condition of the fetus. The daily fetal movement count (DFMC) (also called kick count) can be assessed at home and is noninvasive, inexpensive, simple to understand, and usually does not interfere with a daily routine. The DFMC is frequently used to monitor the fetus in pregnancies complicated by conditions that may affect fetal oxygenation (see Box 19-2). The presence of movements is generally a reassuring sign of fetal health. Diagnostic ultrasonography is an important, safe technique in antepartum fetal surveillance. It provides critical information to health care providers regarding fetal activity and gestational age, normal versus abnormal fetal growth curves, visual assistance with which invasive tests may be performed more safely, fetal and placental anatomy, and fetal well-being (Richards, 2007). Ultrasound examination can be performed abdominally or transvaginally during pregnancy. Both methods produce a two- or three-dimensional view from which a pictorial image is obtained (Fig. 19-1, A, B). It is also possible to produce a four-dimensional image. Abdominal ultrasonography is more useful after the first trimester when the pregnant uterus becomes an abdominal organ. During the procedure, the woman usually should have a full bladder to displace the uterus upward to provide a better image of the fetus. Transmission gel or paste is applied to the woman’s abdomen before a transducer is moved over the skin to enhance transmission and reception of the sound waves. She is positioned with small pillows under her head and knees. The display panel is positioned so that the woman or her partner (or both) can observe the images on the screen if they desire. The American College of Obstetricians and Gynecologists (ACOG) (2004) describes three levels of ultrasonography. The standard examination is used most frequently and can be performed by ultrasonographers or other heath care professionals, including nurses, who have had special training. Indications for standard ultrasonography are described in detail in the next section. Its primary uses are to detect fetal viability, determine the presentation of the fetus, assess gestational age, locate the placenta, examine the fetal anatomic structures for malformations, and determine amniotic fluid volume (AFV). Limited examinations are performed for specific indications such as identifying fetal presentation during labor or evaluating fetal heart rate (FHR) activity when it is not detected by other methods (ACOG). Specialized or targeted examinations are performed if a woman is suspected of carrying an anatomically or a physiologically abnormal fetus. Indications for this comprehensive examination include abnormal findings on clinical examination, especially with polyhydramnios or oligohydramnios, elevated alpha-fetoprotein (AFP) levels, and a history of offspring with anomalies that can be detected by ultrasound examination. Specialized ultrasonography is performed by highly trained and experienced personnel (ACOG). Major indications for obstetric sonography are listed by trimester in Table 19-1. During the first trimester, ultrasound examination is performed to obtain information regarding the number, size, and location of gestational sacs; the presence or absence of fetal cardiac and body movements; the presence or absence of uterine abnormalities (e.g., bicornuate uterus or fibroids) or adnexal masses (e.g., ovarian cysts or an ectopic pregnancy); and pregnancy dating (by measuring the crown-rump length). TABLE 19-1 Major Uses of Ultrasonography during Pregnancy
Assessment of High Risk Pregnancy
Assessment of Risk Factors

Antepartum Testing
Biophysical Assessment

Daily Fetal Movement Count
Ultrasonography


Levels of ultrasonography
Indications for use
FIRST TRIMESTER
SECOND TRIMESTER
THIRD TRIMESTER
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Assessment of High Risk Pregnancy
Get Clinical Tree app for offline access
