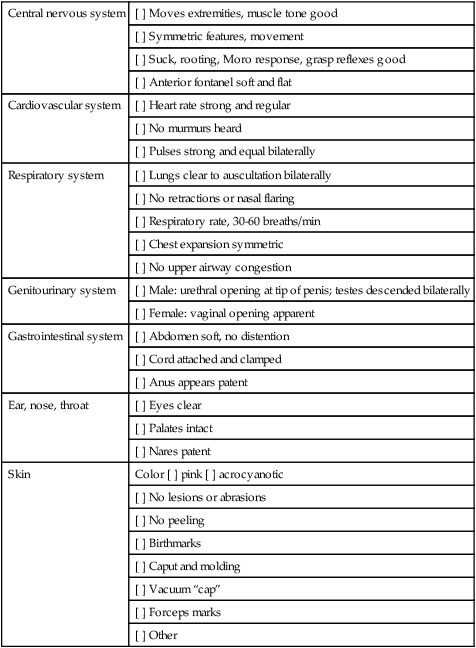
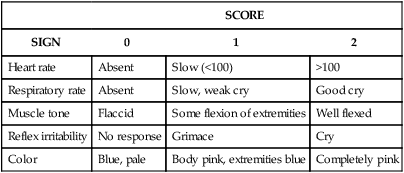
• Explain the purpose and components of the Apgar score. • Compare and contrast the characteristics of the preterm, late preterm, term, and postterm neonate. • Perform a gestational age assessment of a newborn. • Explain the elements of a safe environment. • Discuss phototherapy and the guidelines for teaching parents about this treatment. • Explain the purposes for and methods of circumcision, the postoperative care of the circumcised infant, and parent teaching regarding circumcision. • Review the procedures for performing a heel stick, collecting urine specimens, and assisting with venipuncture. • Evaluate pain in the newborn based on physiologic changes and behavioral observations. • Review anticipatory guidance nurses provide to parents before discharge. Additional related content can be found on the companion website at http://evolve.elsevier.com/Lowdermilk/Maternity/ • Assessment Videos: Circumcision, Crying Female Neonate • Case Study: The Normal Newborn • Critical Thinking Exercise: Circumcision • Critical Thinking Exercise: Jaundice • Nursing Care Plan: Immediate Care of the Newborn • Nursing Care Plan: The Normal Newborn and Family • Spanish Guidelines: Daily Care • Spanish Guidelines: General Advice The initial assessment of the neonate is performed immediately after birth using the Apgar score (Table 17-1) and a brief physical examination (Box 17-1). A gestational age assessment is completed within the first hours of birth in a stable newborn. A more comprehensive physical assessment is completed within 24 hours of birth (see Table 16-4). TABLE 17-1 The Apgar score permits a rapid assessment of the newborn’s transition to extrauterine existence based on five signs that indicate the physiologic state of the neonate: (1) heart rate, based on auscultation with a stethoscope or palpation of the umbilical cord; (2) respiratory rate, based on observed movement of respiratory efforts; (3) muscle tone, based on degree of flexion and movement of the extremities; (4) reflex irritability, based on response to bulb syringe or catheter inserted in the nasopharynx; and (5) generalized skin color, described as pallid, cyanotic, or pink (see Table 17-1). Evaluations are made at 1 and 5 minutes after birth and can be completed by the nurse or birth attendant. Scores of 0 to 3 indicate severe distress, scores of 4 to 6 indicate moderate difficulty, and scores of 7 to 10 indicate that the infant is having minimal or no difficulty adjusting to extrauterine life. Apgar scores do not predict future neurologic outcome but are useful for describing the newborn’s transition to extrauterine environment (Box 17-2). If resuscitation is required, it should be initiated before the 1-minute Apgar score (American Academy of Pediatrics [AAP] and American College of Obstetricians and Gynecologists [ACOG], 2007). The initial physical assessment includes a brief review of systems (see Box 17-1): 1. External: Note skin color, general activity, position; assess nasal patency by closing one nostril at a time while observing respirations; skin: peeling, or lack of subcutaneous fat (preterm or postterm); temperature; note meconium staining of cord, skin, fingernails, or amniotic fluid (staining may indicate fetal release of meconium); note length of nails and development of creases on soles of feet. 2. Chest: Auscultate apical heart for rate and rhythm, heart tones, and presence of abnormal sounds; assess rate and character of respirations and presence of crackles or other adventitious sounds; note equality of breath sounds by auscultation and observation. 3. Abdomen: Verify characteristics of the abdomen (rounded, flat, concave) and absence of anomalies; auscultate bowel sounds; note number of vessels in the cord and general status of the cord (e.g., thin, emaciated; thick, tortuous; presence of hematoma). 4. Neurologic: Check muscle tone, and assess Moro and suck reflexes; palpate anterior fontanel; note by palpation the presence and size of the fontanels and sutures; note bulging or depression of the anterior fontanel. 5. Genitourinary: Note external sex characteristics and any abnormality of genitalia; check anal patency (presence of meconium); note passage of urine. 6. Other observations: Note gross structural malformations obvious at birth that may require immediate medical attention (e.g., omphalocele, meningocele). If the infant has excess mucus in the respiratory tract, the mouth and nasal passages can be gently suctioned with a bulb syringe (Fig. 17-1). Routine chest percussion and suctioning of healthy term or late preterm infants is avoided; evidence is insufficient to support anything other than gentle nasopharyngeal and oropharyngeal suctioning to clear secretions (Hagedorn, 2006). The infant who is choking on secretions should be supported with the head to the side. The mouth is suctioned first to prevent the infant from inhaling pharyngeal secretions by gasping as the nares are touched. The bulb is compressed and inserted into one side of the mouth. The center of the mouth is avoided because the gag reflex could be stimulated. The nasal passages are suctioned one nostril at a time. The nurse should listen to the infant’s respirations and lung sounds with a stethoscope to determine whether crackles, rhonchi, or inspiratory stridor are present. Fine crackles may be auscultated for several hours after birth. If the bulb syringe does not clear mucus interfering with respiratory effort, mechanical suction can be used. If the newborn has an obstruction that is not cleared with suctioning, further investigation must occur to determine if a mechanical defect (e.g., tracheoesophageal fistula, choanal atresia [see Chapter 24]) is causing the obstruction. Four conditions are essential for maintaining an adequate oxygen supply: • Effective establishment of respirations • Adequate circulation, adequate perfusion, and effective cardiac function • Adequate thermoregulation (Exposure to cold stress increases oxygen and glucose needs.) Effective neonatal care includes maintenance of an optimal thermal environment (see Chapter 16). Cold stress increases the need for oxygen and may deplete glucose stores. The infant may react to exposure to cold by increasing the respiratory rate and may become cyanotic. Ways to stabilize the newborn’s body temperature include placing the infant directly on the mother’s abdomen and covering with a warm blanket (skin-to-skin contact), drying and wrapping the newborn in warmed blankets immediately after birth, keeping the head well covered, and keeping the ambient temperature of the nursery at 22° to 26° C (AAP & ACOG, 2012). Allowing vernix caseosa to remain on the infant’s skin has not been associated with a decrease in axillary temperature in the first hour after birth (Visscher et al., 2005). The instillation of a prophylactic agent in the eyes of all neonates (Fig. 17-2) is mandatory in the United States. This is a precautionary measure against ophthalmia neonatorum, which is an inflammation of the eyes resulting from gonorrheal or chlamydial infection contracted by the newborn during passage through the mother’s birth canal. In the United States, if parents object to this treatment, they may be asked to sign an informed refusal form, and their refusal will be noted in the neonate’s record. The agent used for prophylaxis varies according to hospital protocols, but usual agents include forms of erythromycin, tetracycline, or silver nitrate (Medication Guide). Canadian hospitals have not recommended the use of silver nitrate since 1986. Its use in the United States is minimal because silver nitrate does not protect against chlamydial infection and can cause chemical conjunctivitis. Instillation of eye prophylaxis may be delayed until an hour or so (up to 2 hours in Canada) after birth so that eye contact and parent-infant attachment and bonding are facilitated. Topical antibiotics such as tetracycline and erythromycin, silver nitrate, and a 2.5% povidone-iodine solution (currently unavailable in commercial form in the United States) are not effective in the treatment of chlamydial conjunctivitis. A 14-day course of oral erythromycin or an oral sulfonamide may be given for chlamydial conjunctivitis (AAP, 2006). Administering vitamin K intramuscularly is routine in the newborn period in the United States. A single intramuscular injection of 0.5 to 1 mg of vitamin K is given soon after birth to prevent hemorrhagic disease of the newborn. Administration can be delayed until after the first breastfeeding in the birthing room (AAP & ACOG, 2012). Vitamin K is produced in the gastrointestinal tract by bacteria starting soon after microorganisms are introduced. By day 8, healthy newborns are able to produce their own vitamin K (Medication Guide).
Assessment and Care of the Newborn and Family
Web Resources
![]()
Assessment
Initial Assessment and Apgar Scoring
SCORE
SIGN
0
1
2
Heart rate
Absent
Slow (<100)
>100
Respiratory rate
Absent
Slow, weak cry
Good cry
Muscle tone
Flaccid
Some flexion of extremities
Well flexed
Reflex irritability
No response
Grimace
Cry
Color
Blue, pale
Body pink, extremities blue
Completely pink
Apgar score
Initial physical assessment
Interventions
Airway maintenance

Maintaining an adequate oxygen supply.
Maintaining body temperature
Immediate interventions
Eye prophylaxis.

Vitamin K prophylaxis.

Assessment and Care of the Newborn and Family
Get Clinical Tree app for offline access
 to
to  weeks of gestation
weeks of gestation