Chapter 5 Asepsis and infection control
After reading this chapter, you should be able to:
Classification and types of microorganisms
In order to understand the infective process and the measures taken to prevent transmission of microorganisms, it is necessary to review aspects of microbiology. It is beyond the scope of this text to explore microbiology in depth but a brief examination of the particular organisms of concern, in relation to the care of surgical patients, is presented. Two main classifications of microorganisms are described by Burton and Engelkirk (2000):
Bacteria
Bacteria are simple, unicellular organisms containing internal structures, such as a nucleus, cytoplasm, plasmids and ribosomes (Lee & Bishop, 2006). Even though there are thousands of bacteria, very few cause disease/infection. Bacteria are extremely adaptable and survive and grow in various environments, often multiplying rapidly. For example, a single Escherichia coli bacterium can reproduce itself in 20 minutes and give rise to over a million bacterial cells in about 10 hours (Lee & Bishop, 2006).
Bacteria are the commonest cause of surgical site infections (SSIs), with staphylococci and streptococci being responsible for many of these (Lee & Bishop, 2006; Nicolette, 2007). Most bacteria found in the perioperative environment are shed from the skin of personnel (Nicolette, 2007); hand washing is the most efficacious way of countering their spread.
Gram-positive cocci
Staphylococci
Staphylococci (e.g. Staphylococcus aureus and Staphylococcus epidermidis) are round or spherical-shaped Gram-positive bacteria, and are part of the normal flora found on the skin and mucous membrane of the nasopharynx, urethra and vagina. They can exist in these areas without any adverse effect on the host and those that live on the skin are termed ‘transient’ organisms. Staphylococci can survive for long periods in the air, dust, bedding and clothing, making cleanliness of the perioperative environment paramount (Phillips, 2007). These bacteria are transmitted from the hands of the host to another person, where they can subsequently have significant negative effects. For example, they can enter the wound of a surgical patient and cause a wound infection or worse, because of their ability to develop resistance to antibiotics quickly (Lee & Bishop, 2006). Exotoxins secreted by S. aureus can cause toxic shock syndrome which, if left untreated, can be fatal (Lee & Bishop, 2006; Phillips, 2007). Staphylococci are strongly associated with healthcare-associated (nosocomial) infection (HAI).
Streptococci
Streptococci are responsible for a wide range of diseases and infections. These include throat and wound infections, pneumonia, septicaemia and necrotising fasciitis. Streptococcus pyogenes is frequently implicated in SSIs. Streptococci tend to be more virulent than staphylococci; however, they are much more likely than the latter to be sensitive to penicillin (Nicolette, 2007). Streptococci can be a normal resident of the upper airway, vagina and anus (Lee & Bishop, 2006; Nicolette, 2007) and are spread via direct and indirect contact, causing infection and illness in susceptible populations.
Enterococci
Enterococci are bacteria normally found in the gastrointestinal tract and female genital tract. They cause infections, such as SSI and septicaemia, when they are transmitted via the hands or contaminated equipment to susceptible, high-risk patients, including surgical patients (Nicolette, 2007). They are becoming an increasingly significant hospital pathogen because strains of enterococci have developed resistance to the antimicrobial drug vancomycin, which is the last resort treatment for methicillin-resistant staphylococcal infections (MRSA) (Lee & Bishop, 2006).
Gram-positive rods
Clostridia are Gram-positive anaerobic bacteria that produce toxins that cause serious illness, such as tetanus (Clostridium tetani) and gangrene (Clostridium perfringens). They have the ability to produce endospores, which enables them to encapsulate themselves in a special protein coat, giving them the ability to survive under adverse conditions (Lee & Bishop, 2006). Endospores can survive for many years and are highly resistant to drying and heat (Phillips, 2007). When conditions improve, the endospore germinates into a new bacterial cell. Sterilisation techniques must be able to destroy bacterial spores; these are discussed later in the chapter. Clostridium difficile, another example of this genus, can cause serious infection within the large intestine, especially in patients on long-term antibiotic therapy (Lee & Bishop, 2006; NZ Ministry of Health, 2007).
Fungi
There are two major types of fungi—yeast and moulds—and many are beneficial to humans; for example, moulds are a source of antibiotics (Lee & Bishop, 2007). They are often termed ‘nature’s original recyclers’ because they secrete enzymes that decompose dead plant and animal matter, turning them into absorbable nutrients. Although of less significance within the perioperative setting, some fungal strains, such as Candida albicans, cause localised infections in the mouth and reproductive tract, which have the potential to become systemic infections. Fungi have been isolated in the nail beds of nurses who wear acrylic nails, even following normal surgical scrub techniques (NSW Health, 2007b). This has led to policies prohibiting acrylic nails within the operating suite due to the danger of transmitting fungal infections to patients (Australian Department of Health and Ageing, 2004).
Viruses
Unlike bacteria, viruses do not have a cellular structure and do not fit the classification for a living cell because they cannot reproduce or carry out any metabolic reactions. However, like some bacteria, they cause significant infections. Viruses replicate by invading a host cell and using the host cell’s DNA, protein and other nutrients to survive and reproduce. In the process, they damage or destroy the host cell. The reproductive process concludes when the host cell bursts (cell lysis), spreading new viruses to nearby cells, where the process is repeated (Lee & Bishop, 2006). This process stimulates an antibody response in the infected person.
Prions
Prions are small infectious particles consisting of protein only with no nucleic acid. They are implicated in unusual neurodegenerative disorders, including bovine spongiform encephalopathy (BSE) or ‘mad cow disease’ and, in humans, Creutzfeldt-Jakob disease (CJD) (Lee & Bishop, 2006). The mechanism of infection that causes CJD is still unclear, although it is thought that prions have the ability to convert normal protein molecules into dangerous ones (Burton & Engelkirk, 2000). Prions are unusually resistant to conventional chemical and physical sterilising methods, and special protocols for managing instruments that have been used on infected or potentially infected patients are discussed later in this chapter (Nicolette, 2007). Table 5-1 summaries the common microorganisms found in the perioperative environment.
Table 5-1 Common microorganisms found in the perioperative environment
| Microorganism | Usual environment | Mode of transmission |
| Staphylococci | Skin, hair | Direct contact |
| Upper respiratory tract | Airborne | |
| Escherichia coli | Intestinal tract | Faeces, urine |
| Urinary tract | Direct contact | |
| Streptococci | Oronasopharynx | Airborne |
| Skin, perianal area | Direct contact | |
| Mycobacterium tuberculosis | Respiratory tract | Airborne, droplet |
| Urinary tract | Direct contact | |
| Pseudomonas | Urinary tract | Direct contact |
| Intestinal tract | Urine, faeces | |
| Water | Water | |
| Serratia marcescens | Urinary tract | Direct contact |
| Respiratory tract | Water | |
| Clostridium | Intestinal tract | Direct contact |
| Fungi | Dust, soil | Airborne |
| Inanimate objects | Direct contact | |
| Hepatitis virus | Blood | Blood-borne |
| Body fluids | Direct contact |
Development of resistance to antimicrobial drugs
The emergence of strains of pathogens that are resistant to currently available antimicrobial drugs represents a significant threat to surgical patients. Those of concern in the perioperative environment include methicillin-resistant S. aureus (MRSA), which is also resistant to other categories of antimicrobials. MRSA has become a serious concern among hospitalised patients and can be fatal in those who are susceptible (Phillips, 2007). S. aureus is frequently implicated in SSIs (Lee & Bishop, 2006). Other microorganisms that have become resistant to antimicrobial drugs include vancomycin-resistant enterococci (VRE) and multi-drug resistant tuberculosis (TB), which is transmitted by droplets from infected individuals or improperly cleaned bronchoscopes and anaesthetic equipment. The prohibitive costs of developing new antimicrobial drugs have led to a greater emphasis on appropriate prescribing practices and more stringent infection control measures to limit the spread of resistant organisms in hospitals (Lee & Bishop, 2006; NZ Ministry of Health, 2007).
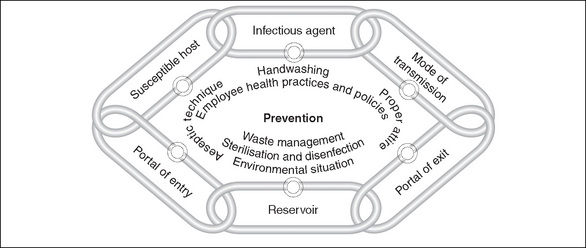
Process of Infection
The process of infection can be likened to the links in a chain—break any of the links and infection can be prevented (Nicolette, 2007). There are six links in the chain of infection:
Reservoir
The microorganisms responsible for the majority of HAI (nosocomial infections) originate either from the patient’s own body flora (endogenous infections) or exogenous (external) sources, such as other patients, staff or equipment. Some microorganisms exist harmlessly on patients’ skin, in hair follicles, sweat glands (staphylococci) or within the bowel as normal flora (E. coli). However, when these microorganisms enter another area of the body, they can cause infection (e.g. E. coli can cause bladder infections and S. aureus causes SSIs). Both transient and resident microorganisms are found on the skin (Tanner et al., 2007) and these can be transferred by direct contact between patients, health care workers, visitors and equipment, or by transfer to other body sites within the same patient, where infection can subsequently develop. Transient microorganisms are easily removed by good hand hygiene.
Portal of entry
Transmission
The transmission of microorganisms cannot occur unassisted. In the hospital setting, the most common mode of transmission is through people; this is mainly via the hands of health care workers, other patients or visitors directly touching the patient or through the use of contaminated objects (Gilmour, 2005). Vigilance in hand hygiene and the use of aseptic technique are the most efficient methods of preventing the transmission of microorganisms. Understanding the routes and sources of transmission is vital if this link in the chain is to be broken.
Portal of exit
For microorganisms to continue infecting other hosts, they must have a means of leaving the body. This may be via blood or other body fluids, faeces or droplets from the respiratory tract (Gilmour, 2005).
Normal body defences
Whether or not a person develops an infection as a result of invasion by microorganisms will depend on the susceptibility of that person (the host) and the virulence of the microorganism. It will also depend on the body’s ability to defend itself against the invading pathogens.
External barriers
External barriers include the skin, mucous membranes and their respective secretions; these are the body’s first line of defence in preventing infection. The epidermal layer of the skin contains a protein, keratin, which provides substantial resistance to bacterial enzymes and toxins. The dermal layer of skin contains sebum-secreting sebaceous glands, which lower the pH of the skin, inhibiting the growth of some bacteria and fungi (Lee & Bishop, 2006). Mucous membranes heal quickly despite much wear and tear, and their sticky, mucous secretions trap foreign particles and microorganisms.
Inflammatory response
The onset of inflammation is a non-specific defence. It is the body’s response to tissue damage and is evoked following any injury (e.g. physical, chemical, radiation) or invasion by microorganisms. The function of inflammation is to clear the injured site of cellular debris and any pathogens present, and to enable tissue repair to commence (Phillips, 2007). Once the inflammatory response is evoked, several biochemical mediators are released, localised vasodilation occurs and plasma fluid (containing leucocytes and proteins) moves into the injured area. This causes the four outward signs of inflammation, namely, redness, heat, swelling and pain (Lee & Bishop, 2006). If the inflammatory response does not eliminate all organisms or foreign material, healing of the injury is delayed and chronic inflammation can be result, which can persist for weeks or even months (Lee & Bishop, 2006).
Immune response
The immune response, the third line of protection, is a specific body defence. Immunity is the capacity of the body’s immune system to defend itself successfully against potentially infectious agents. Immunity is acquired in two ways. Firstly, active immunity is acquired when the body has been exposed to or suffered an infection; this is ‘naturally acquired’ immunity. Artificially acquired active immunity results from immunisation, such as with vaccines (e.g. diphtheria) given in childhood. Passive immunity may be natural and occurs when antibodies are transferred from a person with immunity to another who does not have immunity (e.g. from mother to fetus across the placental barrier) (Lee & Bishop, 2006), or artificial and can be conferred with injections of immune globulins. For example, hepatitis B immunoglobulin injections may be given to a health care worker following a sharps injury and potential exposure to hepatitis B virus. Unlike active immunity, passive immunity is relatively short-lived (Lee & Bishop, 2006).
Infection as an adverse event
Infection is one of the most frequent adverse events associated with surgical procedures and/or interventions (Wicker & O’Neill, 2006). The cost of HAIs can be measured in terms of increased morbidity and mortality, increased length of stay in hospital and an increase in both human and clinical resources (Pittet, 2005). Worldwide, HAIs and the present threat from multiresistant organisms (MROs) are said to be responsible for the death of up to 1400 people daily; this constitutes one of medicine’s greatest challenges (Best & Neuhauser, 2004). Such is the significance of MROs that health departments are now developing and implementing MRO-specific policies (NSW Health, 2007a; NZ Ministry of Health, 2007). Surgical patients have a three-fold greater risk of HAI compared to other patients (Australian Department of Health and Ageing, 2004). Despite compelling evidence about the effectiveness of hand washing in reducing the spread of infection within health care facilities, compliance remains problematic. Increasingly, attention must be paid to all of the practices described here because they are either effective or they reduce reliance on antibiotic therapies.
Bioterrorism
Finally, microorganisms are a key component of biological warfare, which has become a very real threat (Nicolette, 2007). The US Centers for Disease Control (CDC) has identified anthrax and smallpox as the two most likely biological weapons with the ability to be spread quickly and easily within large populations. The resultant panic and disruption to the social fabric requires all health professionals to be aware of local procedures when dealing with a potential pandemic (Nicolette, 2007). Although it is unlikely that perioperative nurses will care for surgical patients with these diseases, in the event of a national crisis, they may well be called upon as part of the emergency preparedness plan.
Infection control
Successful infection control practices focus on prevention; this involves identifying hazards and classifying associated risks (Australian Department of Health and Ageing, 2004). In turn, this requires health care facilities to develop infection control risk management plans, ideally within a clinical governance framework, to minimise the risk of preventable nosocomial infections (NSW Health, 2007a). Elements of successful infection control include quality and risk management policies, effective work practices and procedures, and adequate physical facilities and operational controls (Australian Department of Health and Ageing, 2004; Nicolette, 2007; NZ Ministry of Health, 2007). Major risk factors can be found within the perioperative setting, so additional and specific requirements to prevent infection are needed (Australian Department of Health and Ageing, 2004). These are addressed below.
Environmental controls
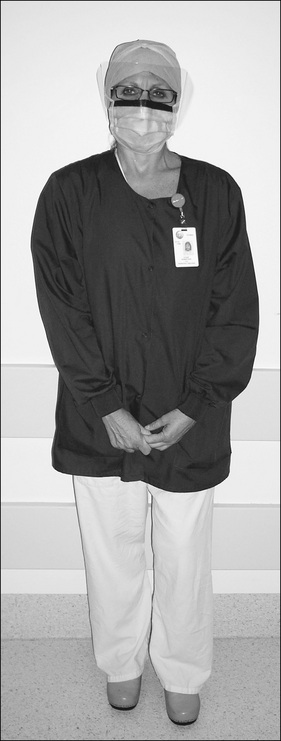
Chapter 3 looked at all aspects of the perioperative environment, noting that many operating suite design features are necessary for good infection control. These include the concept of the four zones of the perioperative environment. Personnel entering the semi-restricted and restricted zones of the operating suite must be correctly dressed in perioperative attire in order to minimise the entry of microorganisms found on the outside (street) clothing of personnel.
Attire
Correct perioperative attire (Fig 5-2) includes the following:
Face masks
The wearing of fluid-resistant face masks is an important part of perioperative attire. The tradition of wearing masks was based on the unfounded assumption that their use protected patients, although there is limited evidence to support this (Lipp & Edwards, 2002). However, there is now sufficient evidence to warrant the use of face masks to prevent the droplet spread of oropharyngeal flora during insertion of spinal or epidural anaesthesia (Siegel et al., 2007). Their continued use is also predicated on the need to protect health care workers (Australian Department of Health and Ageing, 2004; Phillips, 2007; Siegel et al., 2007). Within the perioperative setting, the following practices are recommended.
Moving around the operating room
Too much activity within the operating room provides opportunities for the transmission of microorganisms (Lee, 2005). In order to reduce unnecessary movement, forward planning is needed; for example, place all the requirements for a case in the operating room prior to commencement. Other considerations include the following:
Infection control practices
Consistent with international standards and practices, a two-tiered approach to infection control is endorsed in Australia and New Zealand. Standard precautions are used for all patients regardless of their diagnosis or presumed infection status. Additional (or transmission-based) precautions are applicable only to the care of specified patients (Australian Department of Health and Ageing, 2004; NSW Health, 2007a).
Standard precautions
Standard precautions are designed to reduce the transmission of microorganisms from both recognised and unrecognised sources. They involve safe work practices and protective barriers (Siegel et al., 2007). Standard precautions protect patients and health care workers, and they apply to:
Hand hygiene is the single most important practice to reduce transmission of infectious agents in health care settings (NSW Health, 2007b). Hands must be washed after contact with the patient, after removing gloves and between tasks that involve contact with potentially contaminated equipment. Antimicrobial agents, such as chlorhexidine and waterless alcohol-based hand rubs, are available for routine hand hygiene.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree