Arterial Pressure Monitoring
Direct arterial pressure monitoring permits continuous measurement of systolic, diastolic, and mean arterial pressures and allows for arterial blood sampling. Because direct measurement reflects systemic vascular resistance as well as blood flow, it’s generally more accurate than indirect methods (such as palpation and auscultation of Korotkoff, or audible pulse, sounds), which are based on blood flow.
Direct monitoring is indicated when highly accurate or frequent blood pressure measurements are required, such as for patients with low cardiac output and high systemic vascular resistance. It may also be used for hospitalized patients who are obese or have severe edema—conditions that may make indirect measurement difficult to perform. It’s also useful for patients receiving titrated doses of vasoactive drugs and for those requiring frequent blood sampling.
Arterial pressure monitoring is used in critical care settings. To carry out monitoring, the doctor inserts an arterial catheter, which allows for direct arterial pressure monitoring. The procedure can be performed at the bedside under surgically sterile conditions.
Arterial monitoring equipment permits waveform evaluation and allows the nurse to make clinical decisions about changes in the patient’s therapy. (See Understanding the arterial waveform, page 30.)
Understanding the Arterial Waveform
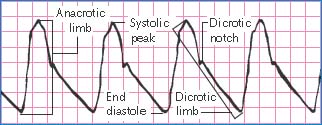
Normal arterial blood pressure produces a characteristic waveform, representing ventricular systole and diastole. The waveform has five distinct components: the anacrotic limb, systolic peak, dicrotic limb, dicrotic notch, and end diastole.
The anacrotic limb marks the waveform’s initial upstroke, which results as blood is rapidly ejected from the ventricle through the open aortic valve into the aorta. The rapid ejection causes a sharp rise in arterial pressure, which appears as the waveform’s highest point. This is called the systolic peak.
As blood continues into the peripheral vessels, arterial pressure falls, and the waveform begins a downward trend. This part is called the dicrotic limb. Arterial pressure usually will continue to fall until pressure in the ventricle is less than pressure in the aortic root. When this occurs, the aortic valve closes. This event appears as a small notch on the waveform’s downside, called the dicrotic notch. When the aortic valve closes, diastole begins, progressing until the aortic root pressure gradually descends to its lowest point. On the waveform, this is known as end diastole.
A patient being monitored with an arterial pressure monitoring system can have blood samples for laboratory testing withdrawn from the arterial catheter. The arterial pressure monitoring system can be open or closed. An open system is one in which a Vacutainer is attached to the stopcock, withdrawing 5 to 10 mL of blood for waste, which is then discarded. A closed system has an attached reservoir that withdraws the waste; when all appropriate blood samples have been obtained, the blood in the reservoir can be returned to the patient.
According to the Centers for Disease Control and Prevention and the Infusion Nurses Society, the tubing and flush solution for an arterial line is considered a closed system and should be changed every 96 hours, immediately if contamination is suspected, or when the integrity of the product is compromised.1,2 In some cases, however, you may need to change the flush solution more frequently due to use.
Removal of an arterial catheter should occur as soon as possible to decrease the risk of complications, such as thrombosis and infection.1
Equipment
For Catheter Insertion
Disposable pressure transducer system ▪ 250-mL bag of normal saline solution ▪ arterial catheter ▪ unvented or dead-end caps ▪ pressure tubing ▪ pressure bag or IV pump ▪ transducer holder on an IV pole ▪ monitoring system and equipment (module, bedside monitor, cable, and hookup) ▪ suture material ▪ sterile transparent dressing ▪ sterile hypoallergenic tape ▪ carpenter’s level ▪ Optional: arm board or limb-immobilization device, chlorhexidine-impregnated sponge.
For Blood Sampling
Gloves ▪ gown ▪ mask ▪ protective eyewear ▪ linen-saver pad ▪ laboratory request forms and labels ▪ appropriate blood sample collection tubes ▪ laboratory biohazard transport bag ▪ antiseptic wipes (alcohol, tincture of iodine, or chlorhexidine-based) ▪ sterile nonvented cap ▪ vacutainer ▪ needleless Vacutainer luer adapter.
For Tubing Change
Gloves ▪ gown ▪ mask ▪ protective eyewear ▪ linen-saver pad ▪ preassembled arterial pressure tubing with flush device and disposable pressure transducer ▪ sterile gloves ▪ 500-mL bag of IV flush solution (typically normal saline solution) ▪ antiseptic solution swabs ▪ sterile dressing ▪ medication label ▪ pressure bag ▪ site care kit ▪ tubing labels.
For Catheter Removal
Gloves ▪ mask ▪ gown ▪ protective eyewear ▪ two sterile 4″ × 4″ gauze pads ▪ linen-saver pad ▪ 3- or 5-mL syringe ▪ sterile suture removal set ▪ dressing ▪ hypoallergenic tape ▪ Optional: sterile scissors, laboratory biohazard transport bag, sterile container, hemostatic pad, patch, or powder.
Preparation of Equipment
Before setting up and priming the monitoring system, perform hand hygiene.3,4,5,6 Set up and prime the monitoring system. (See “Transducer system setup,” page 739.) Make sure you keep all parts of the pressure monitoring system sterile. Label all medications, medication containers, and other solutions on and off the sterile field.7 When you’ve completed equipment preparation, turn on the bedside monitor alarms according to your facility’s policy.
Implementation
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.8
Maintain asepsis by wearing personal protective equipment throughout all procedures described.
Position the patient for easy access to the catheter insertion site. Place a linen-saver pad under the site.
Inserting an Arterial Catheter
Explain the procedure to the patient and his family, including the purpose of arterial pressure monitoring and the anticipated duration of catheter placement.
Make sure that informed consent has been obtained and is documented in the patient’s medical record.9
Check the patient’s history for any allergy or hypersensitivity to iodine, heparin, or the ordered anesthetic.
If the catheter will be inserted in the radial artery, perform Allen’s test to assess collateral circulation in the hand.
Obtain baseline data, including vital signs, level of consciousness, and hemodynamic stability, to help identify acute changes in the patient.
Assist the doctor as needed during catheter placement. After insertion and while the doctor holds the catheter in place, activate the fast-flush release to flush blood from the catheter. After each fast-flush operation, observe the drip chamber to verify that the continuous flush rate is as desired. A waveform should appear on the bedside monitor.
The doctor may suture the catheter in place, or you may secure it with sterile tape. Cover the insertion site with a chlorhexidine-impregnated sponge (according to your facility’s policy) and then a sterile occlusive dressing (as specified by your facility’s policy), and label the dressing with the date and time.10
Immobilize the insertion site. With a radial or brachial site, use an arm board. With a femoral site, maintain the patient on bed rest, with the head of the bed raised no more than 30 degrees to prevent the catheter from kinking.
Level the zeroing stopcock of the transducer with the phlebostatic axis. Then zero the system to atmospheric pressure.
Nursing Alert
Keep the catheter site visible at all times. Don’t allow linens to cover the site; intra-arterial catheter dislodgment requires prompt recognition and intervention to reduce the risk for exsanguination.
Make sure that the monitor alarms are activated and set appropriately according to your facility’s policy.
Continuously observe the arterial waveform quality on the monitor and record variances to ensure the accuracy of the waveform and to detect changes in the patient’s hemodynamic status. A normal waveform has a peak systole, clear dicrotic notch, and end diastole. Compare the intra-arterial pressure with blood pressure readings obtained by a cuff at least once per shift.
Monitor for potential complications of the arterial catheter, and notify the doctor immediately if any occur.
Troubleshoot the arterial waveform, as needed. Notify the doctor, as appropriate. If the waveform suddenly becomes dampened, check the patient before attempting to determine its cause or fix the problem because a sudden hypotensive episode can look like a dampened waveform on the monitor and can be potentially life-threatening if not treated properly. (See Recognizing abnormal waveforms, page 32.)
Document the procedure.11
Obtaining A Blood Sample
Explain the procedure to the patient.
Position the patient for easy access to the catheter insertion site. Place a linen-saver pad under the site.
Assemble the equipment following sterile technique, taking care not to contaminate the nonvented cap and stopcock.
Label the discard blood sample collection tube to prevent accidentally confusing it with a true specimen.
For an Open Monitoring System
Attach the needleless luer adapter to the Vacutainer.
Temporarily silence the monitor alarms.
Locate the blood sampling port of the stopcock nearest the patient. Remove the nonvented cap from the stopcock.
Connect the needleless adapter of the Vacutainer into the sampling port of the stopcock and turn off the stopcock to the flush solution.
Insert the labeled blood sample collection tube for the discard sample into the Vacutainer. (This sample is discarded because it’s diluted with flush solution.) Follow your facility’s policy on how much discard blood to collect. In most cases, you’ll withdraw 5 to 10 mL.
Insert each blood sample collection tube into the Vacutainer, keeping the stopcock turned off to the flush solution. Because the Vacutainer is a nonvented system, there won’t be any backflow of blood from the patient. If the doctor has ordered coagulation tests, obtain blood for this sample last to prevent dilution from the flush device.
After you’ve obtained blood for the final sample, turn off the stopcock to the Vacutainer. Activate the fast-flush release to clear the tubing.
Turn off the stopcock to the patient, attach a labeled discard blood sample collection tube to the Vacutainer, and repeat the fast flush to clear the stopcock port.
Turn off the stopcock to the stopcock port, and remove the Vacutainer. Place a new sterile, nonvented cap on the blood sampling port; blood or debris left in the existing cap increases the risk for infection.12,13,14,15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access