Chapter 9 Analgesia and anaesthesia
ANALGESIA FOR LABOUR
Inhalational analgesia
The gas is self-administered by inspiration through a facemask or mouthpiece, which opens a demand valve. Diffusion from alveoli to pulmonary capillaries and delivery to the brain by the cardiac output is not instantaneous – inhalation should start as soon as a contraction begins so maximum effect is achieved at its peak (see Chapter 7, Box 7.3).
The drug is non-cumulative, and does not affect the fetus. N2O/O2 causes a variable degree of sedation. Some women appear to be dreaming or drunk; others become somnolent or even briefly unarousable. Hyperventilation with N2O/O2 can be followed by a short period of apnoea, therefore the woman should hold the mouthpiece or mask herself. If she loses consciousness, she will let go. A few breaths of air eliminate the N2O and consciousness will invariably be regained soon. A number of studies have questioned the analgesic effect of N2O/O2. Pain is still perceived under the influence of the drug – it is merely rendered more bearable by the intoxicated state.
Regional analgesia for labour
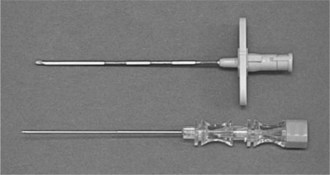
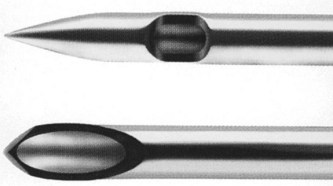
The epidural space is identified by the loss of resistance to depression of a syringe plunger as a Tuohy needle is advanced (Figure 9.1) through the ligamentum flavum. A catheter is then threaded through the Tuohy needle (Figure 9.2) to facilitate top-ups or continuous infusion. The subarachnoid space (containing cerebrospinal fluid (CSF)) is a few millimetres deeper, inside the meninges. Needles used for spinal injection are much finer than Tuohy needles (Figure 9.3). A significant advance has been the development of ‘pencil point’ tips (Figure 9.4). Compared with standard cutting bevel or Quincke needle tips, the leak of CSF and likelihood of consequent headache are vastly reduced.

Figure 9.2 Tuohy needle advanced through the ligamentum flavum, with a catheter in the epidural space.
A trained anaesthetist must always be immediately available whenever regional analgesia is provided. Regional techniques improperly administered can be as hazardous as any general anaesthetic. Resources that should be available on every labour ward in the event of complications (see below) which might arise during the provision of regional analgesia are listed in Box 9.1.
Signed consent is not necessary for regional analgesia in labour. Verbal consent is sufficient, and a brief record should be made in the notes of the risks/benefits that have been discussed.
Table 9.1 outlines the contraindications to regional analgesia, together with the associated risks.
Table 9.1 Contraindications to regional analgesia, with associated risks
| Contraindication | Risk |
|---|---|
| Uncorrected anticoagulation or coagulopathy | Vertebral canal haematoma |
| Local or systemic sepsis (pyrexia >38 °C not treated with antibiotics) | Vertebral canal abscess |
| Hypovolaemia or active haemorrhage | Cardiovascular collapse secondary to sympathetic blockade |
| Maternal refusal | Legal action |
| Lack of sufficient trained midwives for continuous care and monitoring of mother and fetus for the duration of the regional block | Maternal collapse, convulsion, respiratory arrest; fetal compromise |
All women should be warned about the possibility of dural tap – the inadvertent tearing of the meninges by the Tuohy needle or epidural catheter, which should have an incidence of <1%. This complication can predispose to two potentially serious sequelae: total spinal anaesthesia, and post-dural puncture headache (PDPH). The vast majority of pregnant women who develop PDPH will require an epidural ‘blood patch’. Other points worthy of explanation before performing a regional block in labour are listed in Box 9.2.
Box 9.2 Counselling before regional block
Before starting a regional block in labour inform women about:
Epidural analgesia is associated with the following:
It is well worth explaining in advance to women with risk factors for operative delivery that analgesia for labour can be converted to effective anaesthesia to facilitate forceps or caesarean delivery. Some women need time to consider the notion of being awake for a caesarean section.
Complications of regional analgesia
The two principal potential complications of epidural injection of local anaesthetic are local anaesthetic toxicity and total spinal anaesthesia. Aspirating the catheter to exclude intravenous or subarachnoid placement can prevent both. The delivery of local anaesthetic to the brain and heart by the bloodstream causes the symptoms and signs of toxicity (Table 9.2).
Table 9.2 Symptoms and signs of local anaesthetic toxicity
| Symptoms | Signs |
|---|---|
| Numbness of tongue or lips | Slurring of speech |
| Tinnitus | Drowsiness |
| Light-headedness | Convulsions |
| Anxiety | Cardiorespiratory arrest |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree