Chapter 06 Anaesthesia
Pre-anaesthetic assessment of the patient
Prior to the patient undergoing an anaesthetic, a full assessment must be carried out. The preoperative assessment and preparation of the patient has been discussed in detail in Chapter 2. It is important to note the family history, especially of metabolic disease, as certain drugs and anaesthetic agents may affect patients who have a history of malignant hyperthermia. A drug history, including current medications and allergies, should be noted as the interaction of drugs can have serious consequences. A social history, including smoking, alcohol intake and use of illegal drugs, is important to note, as is the use of herbal dietary supplements that are known to produce central nervous system (CNS) stimulation or depression or interact with psychotropic drugs. All these issues can adversely affect the patient’s anaesthetic outcome (Marley, 2005).
The patient assessment must take into consideration the following:
Assessment of the airway
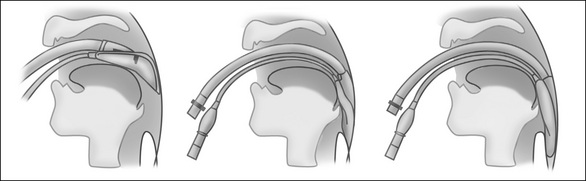
Mallampati assessment
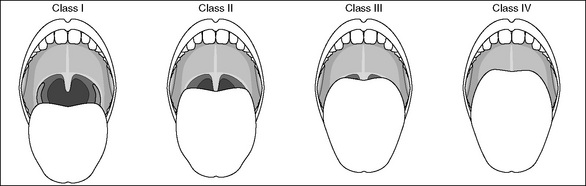
The Mallampati test is used to examine the patient’s oral cavity and soft palate visually to predict any possible difficulties with tracheal intubation. It can be conducted during the pre-anaesthetic assessment.Figure 6-1 shows the four classifications. Classes III and VI, which indicate that viewing of the soft palate is difficult or impossible, suggest a higher degree of difficultly with intubation in these patients (Fell & Kirkbride, 2007).
Further preoperative considerations
The grading system of the American Society of Anesthesiologists (ASA) was introduced in the 1960s as a description of the physical state of the patient, along with an indication of whether surgery is elective or emergency (Fell & Kirkbride, 2007). The ASA physical status classification system is presented in Table 2-2. The ASA classification of the patient will influence the anaesthetist’s decisions about anaesthetic care and postoperative management. These decisions include whether the patient requires postoperative care in the day surgery unit, inpatient bed, high-dependency unit or adult intensive care unit.
Identification and preparation of the patient
The patient is accompanied to the operating suite by a nurse from the ward, who will hand over care of the patient to a member of the perioperative team, usually a nurse in the arrival/waiting area of the operating suite, often termed the ’holding bay’. Both nurses and the patient will participate in completing a preoperative patient checklist (see Figs 2-2 and 2-3) as part of the admission procedure, which will vary according to hospital policy but will include the following:
In addition, it is imperative that an anaesthetic consult is present and complete. Any discrepancies should be noted, reported to the surgical team and rectified before commencement of anaesthesia (ACORN, 2006). The verification of patient details continues throughout each stage of the patient’s care according to local policy.
Types of anaesthetics
Anaesthesia is defined as the ‘loss of the sensations of pain, pressure, temperature and touch in a part of the whole of the body’ (Bryant & Knight, 2007). The main categories of anaesthesia are:
General anaesthesia
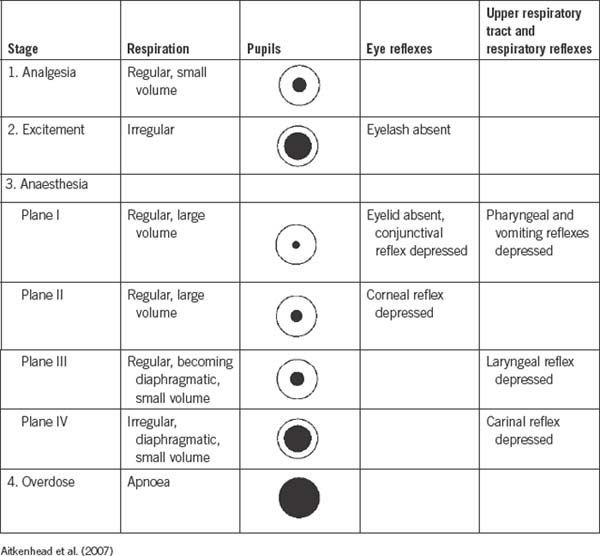
General anaesthesia is a reversible, unconscious state characterised by amnesia, analgesia and suppression of reflexes (DeLamar, 2007). The drugs and gaseous agents used to induce and maintain anaesthesia have a profound physiological effect on body systems, notably the CNS. The area in the CNS that is most affected is the sensory pathways from the thalamus to the cortex, thus depressing conscious thought, motor control, perceptions, memory and sensations. The medullary centres are the final cerebral area to be affected by anaesthesia and unconsciousness occurs, with both respiratory and cardiovascular centres temporarily depressed. These stages of anaesthesia were first described by the American anaesthetist, Arthur Guedel, and are outlined in Table 6-1 (Fell & Kirkbride, 2007).
Pharmacological agents used in general anaesthesia
Intravenous induction agents
IV induction agents are commonly used to induce general anaesthesia because they provide a smoother and more rapid induction than most inhalational agents. Short-acting IV induction agents (e.g. thiopentone, propofol) induce a pleasant sleep, and anaesthesia is maintained for the duration of the surgical procedure by using a combination of oxygen, nitrous oxide and volatile inhalational agents (e.g. sevoflurane). Some anaesthetists may use an IV induction agent as a continuous infusion to maintain anaesthesia, eliminating the need for inhalational agents (Brown & Edwards, 2007).
Inhalational agents
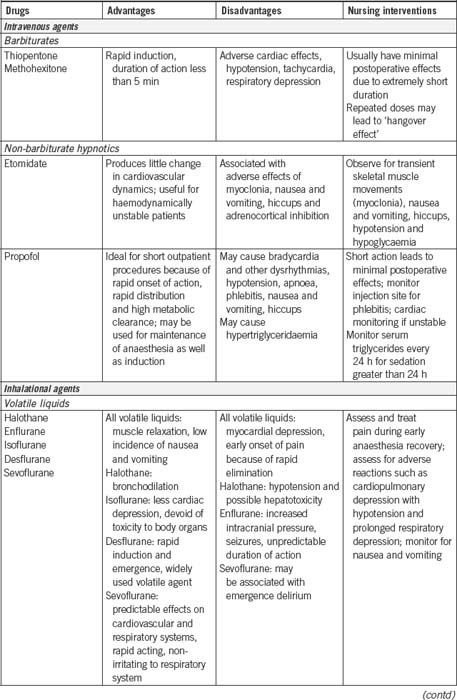
Volatile agents are liquid at room temperature and administered through a specialised vaporiser that is attached to the anaesthetic machine. Oxygen, which is another gas that must be used in all general anaesthesia, passes through the vaporiser and mixes with the liquid agent, changing the volatile agent into a gas. The mixture is delivered to the patient via the variety of airway and delivery equipment attached to the anaesthetic machine. The percentage of inhalational agents delivered to the patient can be adjusted by the anaesthetist depending on the depth of anaesthesia required. Table 6-2 provides a summary of the IV and inhalational agents used in general anaesthesia.
Adjuncts to general anaesthesia
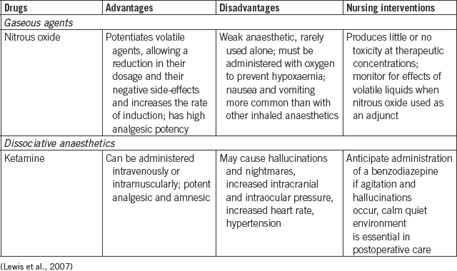
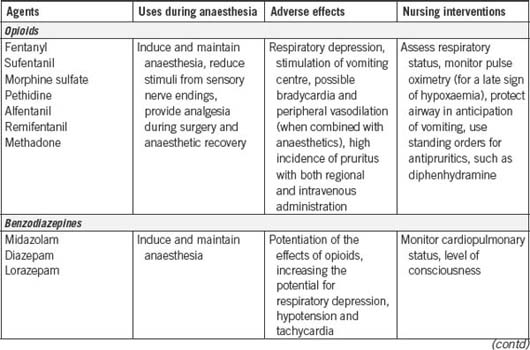
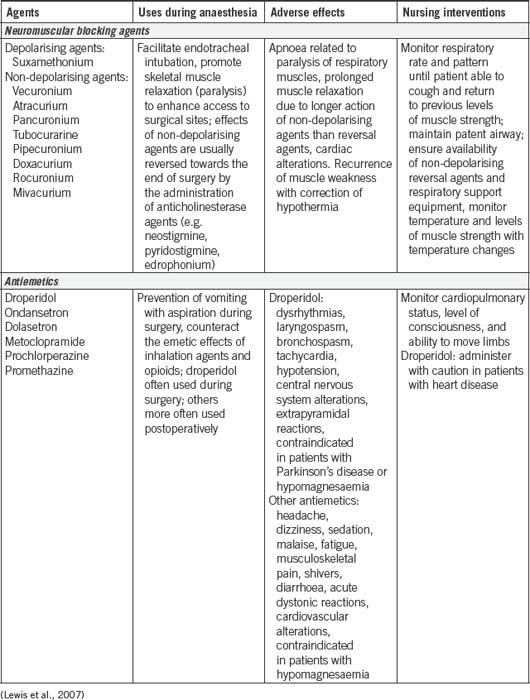
Table 6-3 provides a summary of the most commonly used adjunct drugs to general anaesthesia. As can be seen from Tables 6-2 and 6-3 , many of the agents used to induce anaesthesia and as adjuncts have a powerful effect on the patient’s cardiovascular and respiratory systems. This requires the anaesthetist and anaesthetic nurse to monitor the patient closely using a variety of invasive and non-invasive haemodynamic monitoring devices (see p 151), as well as observational skills.
Analgesics
In addition to the drugs designed to keep the patient under general anaesthesia, opioid analgesic drugs will be given to provide pain relief. Opioid is a term used to refer to a group of drugs, both naturally occurring and synthetically produced, that possess opium or morphine properties. One of the most commonly used opioids is fentanyl (Faut-Callahan & Hand, 2005).
Muscle relaxants
The discovery of curare, a naturally occurring muscle relaxant, by Harold Griffith and Enid Johnson in 1942, was a milestone in anaesthesia. Curare greatly facilitated endotracheal intubation and provided excellent relaxation for abdominal surgery. For the first time, surgery could be performed on patients without having to administer large doses of anaesthetic agents to produce the required muscle relaxation. A wide range of muscle relaxant agents have been developed since, giving today’s anaesthetist a variety of drugs for use in clinical practice (Hunter, 2007).
Muscle relaxation is achieved by blocking neuromuscular activity at the motor end plate of skeletal muscles where the receptors for acetylcholine are located. Acetylcholine, a naturally occurring neurotransmitter, plays an important role in facilitating the transmission of nerve impulses. Interference with the transmission of nerve impulses results in paralysis of skeletal muscle, which includes the muscles of respiration. There are two types of neuromuscular blocking agents: depolarising and non-depolarising agents (Bryant & Knight, 2007).
Suxamethonium is a short-acting depolarising muscle relaxant that acts in 30–60 seconds and lasts 3–5 minutes before it is metabolised by plasma cholinesterase, a naturally occurring enzyme. It is the only agent that creates good conditions for tracheal intubation in emergency airway management or rapid sequence induction. Its onset of action is characterised by facial twitching or fasciculations. However, the effect wears off due to the build-up of plasma cholinesterase (Bryant & Knight, 2007).
To maintain muscle paralysis for the duration of the surgical procedure, a longer acting muscle relaxant is required. These agents are known as non-depolarising muscle relaxants (e.g. rocuronium) and they have a different mode of action to the depolarising agents. Non-depolarising muscle relaxants compete with naturally occurring acetylcholine for receptors at the motor end plate of skeletal muscles, thus causing paralysis. To terminate the action of non-depolarising muscle relaxants, a reversal drug, such as neostigmine, has to be administered towards the end of the procedure. This allows acetylcholine to build up to normal levels and enables normal muscle contraction to return. This results in the patient commencing unassisted respiration once all other anaesthetic agents have been stopped. A side-effect of neostigmine is bradycardia, which is counteracted by the simultaneous administration of an antimuscarinic drug (e.g. atropine, glycopyrrolate), which has a parasympathetic effect and increases pulse rate (Simpson & Popat, 2001).
Procedure for general anaesthesia
Anaesthetic preparation and equipment checking
Prior to the commencement of the operating list, it is important that the anaesthetic machine is checked in accordance with the Australian and New Zealand College of Anaesthetists (ANZCA) guidelines by both the anaesthetist and anaesthetic nurse (ANZCA, 2003b). Anaesthetic machines deliver gases and volatile agents to the patient via delivery tubing that attaches to the patient’s airway management equipment (e.g. endotracheal tube). Oxygen, nitrous oxide and air are piped into the operating room via a network of pipes from a central bulk store of gases within the hospital. A pendant attached to the ceiling delivers the gases to the anaesthetic machine through colour-coded tubes (white for oxygen, blue for nitrous oxide). The fixtures for each gas outlet are gas-specific, which is an important safety feature to ensure that the oxygen tubing cannot physically be attached to the nitrous oxide outlet and vice versa. The same feature exists for the back-up gas cylinders attached to the anaesthetic machine. The anaesthetic machine is more than a gas delivery unit. It also contains a range of sophisticated equipment necessary to monitor the patient’s condition throughout the perianaesthesia period (e.g. ECG, oximetry and capnography).
Other preoperative equipment checks include suction, airway equipment, drugs, additional equipment such as infusion pumps, warming devices and all monitoring equipment. These must be available and in working order prior to the patient’s arrival in order to ensure a smooth and safe anaesthesia process for the patient. Figure 6-2 shows an anaesthetic machine complete with monitoring equipment.

Figure 6-2 Anaesthetic machine and monitoring equipment (Rothrock, 2007, p 108). A, BIS monitor display. B, Patient breathing circuit. C, Reservoir (‘breathing’) bag. D, Carbon dioxide absorber. E, Ventilator.F, Integrated ventilator controls, monitor and displays. G, Oxygen auxiliary outlet. H, Oxygen flush valve. I, On/off switch. J, Monitor display and controls for ECG, temperature, blood pressure, pulse oximetry and end-tidal carbon dioxide. K, Flow meters for air. L, Gauges for pipeline and E-tank pressures (air, nitrous oxide, oxygen). M, Flow-through vaporisers (e.g. desflurane, isoflurane, sevoflurane). N, Power surge protector for anaesthesia machine. O, E-cylinder with oxygen.
Induction of anaesthesia
Induction is defined as the administration of a drug or combination of drugs that results in a state of general anaesthesia (Bryant & Knight, 2007). Preoxygenation of the patient may be carried out to avoid transient hypoxaemia, which can occur before the establishment of an effective airway and ventilation.
During induction it is important that the environment is as quiet as possible to facilitate a smooth induction. Extraneous noise from people talking or the instrument and circulating nurses setting up equipment should be minimised during induction (Fell & Kirkbride, 2007).
Establishment of the airway
Once anaesthesia is induced, the patient will proceed through the stages of anaesthesia shown in Table 6-1. The establishment of an airway now becomes a priority. Depending on the type of procedure being undertaken, and the patient’s history and condition, suitable airways will be selected. To understand how artificial airways are used, it is important to review the anatomy of the airway.
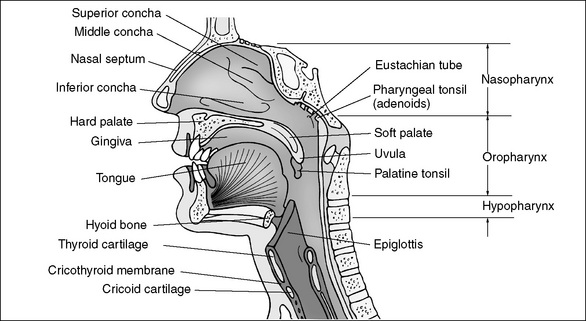
The airway is divided into two sections, upper and lower, which are separated at the level of the cricoid cartilage (Chipas et al., 2005). Figure 6-3 shows the anatomy of the upper airway.
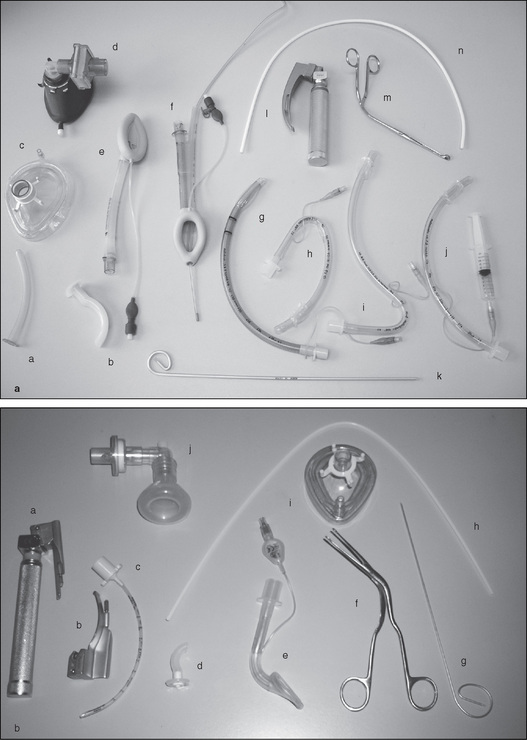
Artificial airways
Artificial airways include oropharyngeal airways, or Guedel airways, which are used in patients whose tongue is obstructing the airway. This can occur when the patient loses upper airway muscle tone, causing the tongue and epiglottis to fall back against the posterior wall of the pharynx. Guedel airways may be used in conjunction with other manoeuvres, such as chin lift and jaw thrust. Nasopharyngeal airways are also available and these require lubrication before insertion via the patient’s nose (Smith et al., 2007).
Face masks
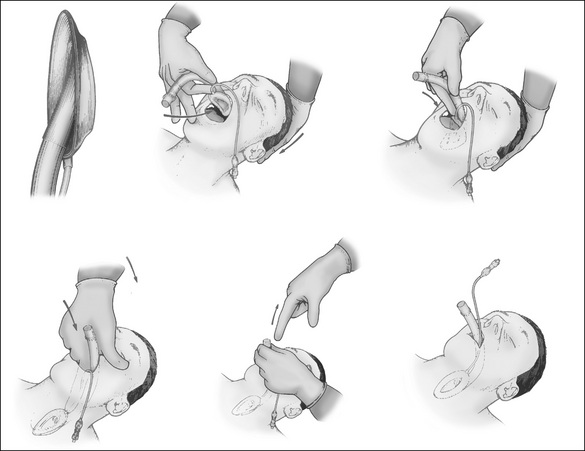
Face masks used in anaesthesia are made of silicone or polyvinyl chloride (PVC) and are designed to fit firmly over the nose and mouth, following the contours of the face as this will assist in providing effective ventilation of an unconscious patient. Several types of face masks are available, including transparent masks, which allow observation of exhaled gas and immediate recognition of vomiting, and cushioned masks, which allow for contouring to facial bone structures (Smith et al., 2007).
Holding face masks requires correct technique to maintain a patent airway. It involves holding the mask with a downward pressure using the thumb and index finger, while the middle and ring fingers grasp the mandible to extend the atlantomaxillary joint. The little finger slides under the angle of the jaw and pulls it anteriorly.
Laryngeal mask airway
Contraindications include patients who are at risk of aspiration due to:
Intubation
A secure airway for the purposes of delivering anaesthesia and emergency airway management can be achieved by the insertion of an ETT. This involves the anaesthetist passing a tube, under direct vision using a laryngoscope, through the vocal cords into the trachea. This tube is connected to the anaesthetic delivery system. A cuff (balloon) located at the distal end of the ETT is inflated to facilitate positive pressure ventilation and to prevent the stomach contents from being aspirated into the patient’s lungs, a condition which can lead to serious pulmonary consequences.
Indications for intubation include: