CHAPTER 3 Affective changes
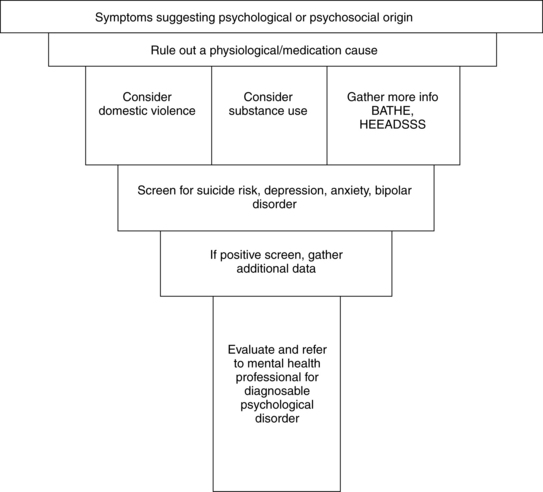
A large percentage of primary care visits have psychological or psychosocial origins. A practitioner must first rule out organic causes for symptoms, mood changes, and behavior changes. Some patients are able to express that their symptoms could be related to situational stress or a psychosocial cause. Others can identify that psychological or emotional difficulties are causing worrisome symptoms or symptoms that interfere with their ability to function. Often the practitioner suspects an underlying psychological or psychosocial disturbance that the patient is not able to articulate. In some cases a parent has concerns about a child’s or adolescent’s behavior. This chapter focuses on commonly encountered psychological conditions and psychosocial concerns, and provides an approach to elicit more information, determine suicide risk, and evaluate for a diagnosable psychological disorder (Figure 3-1).
Diagnostic reasoning: focused history
Symptoms
Physiological problems often present in the patient as abdominal pain (Chapter 2), chest pain (Chapter 7), confusion (especially in the older adult, Chapter 8), dizziness (Chapter 12), fatigue (Chapter 15), headache (Chapter 18), and sleep disturbances (Chapter 28). Refer to the specific chapters that discuss the evaluation of the presenting concern and symptom(s).
Major illness/chronic conditions
The mnemonic THINC MED is useful when evaluating for underlying organic causes of changes in mood or behavior. Box 3-1 identifies conditions that are commonly associated with anxiety and depression.
Box 3-1 THINC MED
Major categories of medical conditions that mimic psychological conditions are as follows:
| T: | Tumors |
| H: | Hormones (e.g., thyroid, adrenal, gonads, insulin) |
| I: | Infections and immune diseases (e.g., AIDS, lupus, syphilis, Lyme disease) |
| N: | Nutrition |
| C: | Central nervous system (e.g., head trauma, seizures, multiple sclerosis, Parkinson’s disease, dementia) |
| M: | Miscellaneous (e.g., sleep apnea, anemia, congestive heart failure) |
| E: | Electrolyte abnormalities and toxins (e.g., hypercalcemia, hypo/hyperphosphatemia, hypo/hypernatremia) |
| D: | Drugs (including nicotine, caffeine, prescribed medications, illicit drugs, and alcohol) |
From Goolsby MJ, Grubbs L: Advanced assessment: interpreting findings and formulating differential diagnoses, Philadelphia, 2006, F.A. Davis.
Medication history
Many medications can cause psychiatric symptoms and mood changes. Box 3-2 lists medications that can produce symptoms of depression, anxiety, and mania.
OTC medications, herbal medicines, and dietary supplements
Is this a domestic violence situation?
Key questions
 Have you been hit, kicked, punched, or otherwise hurt by someone within the past year?
Have you been hit, kicked, punched, or otherwise hurt by someone within the past year?
 Do you feel safe in your current relationship?
Do you feel safe in your current relationship?
 Is there a partner from a previous relationship who is making you feel unsafe now?
Is there a partner from a previous relationship who is making you feel unsafe now?
A positive response to any one of these three questions constitutes a positive screen for partner violence (Feldhaus et al, 1997). The first question, which addresses physical violence, has been validated in studies as an accurate measure of 1-year prevalence rates. The latter two questions evaluate the perception of safety and provide estimates of the short-term risk of further violence and the need for counseling, but reliability and validity evaluations have not yet been established. A positive screen requires further assessment and clinical followup, including ascertaining patient safety.
Could this be situational stress or normal grief?
The BATHE model provides a framework for understanding the patient in the context of his/her total life situation (Lieberman, 1997). BATHE is a mnemonic for Background, Affect, Trouble, Handling, Empathy.
Key questions
Background—ascertains the context of the visit
Affect—elicits the emotional response and allows the patient to label the feeling
Trouble—determines the symbolic meaning of the situation for the patient
Handling—helps to assess patient resources and responses to the situation
Empathy—reflects an understanding that the patient’s response is reasonable under the circumstances
BATHE model
Could this be a result of substance abuse?
Key questions
 In the past year, have you used alcohol or drugs more than you meant to?
In the past year, have you used alcohol or drugs more than you meant to?
 Have you wanted or needed to reduce your drinking or drug use in the past year?
Have you wanted or needed to reduce your drinking or drug use in the past year?
A positive response to one question indicates a substance use concern. When the screen is positive, the CAGE questions can be used to detect alcoholism. Other substances can be substituted for alcohol in the CAGE questionnaire (Box 3-3). Other questionnaires, T-ACE and RAFFT, for alcohol use are also available (Box 3-4 and Box 3-5).
Box 3-3 CAGE Questionnaire
| A Framework for Detecting Alcoholism* | ||
| C: | Concern, Cut down | Have you ever felt you should cut down on your drinking? |
| A: | Annoyed | Have people annoyed you by criticizing your drinking? |
| G: | Guilt | Have you ever felt bad or guilty about your drinking? |
| E: | Eye-opener | Have you ever had an eye-opener drink first thing in the morning to steady your nerves or get rid of a hangover? |
* Answering yes to one or more of the four questions raises a high index of suspicion for alcohol abuse and dependence. The CAGE questionnaire has been used and tested extensively in many populations. It is considered to be a reliable method of screening for alcohol abuse in adults. It has reported sensitivities of 43% to 94% and specificities ranging from 70% to 97%.
From Ewing JA: Screening for alcoholism using CAGE. Cut down, annoyed, guilty, eye opener, JAMA 280:1904, 1998.
Box 3-4 T-ACE Questionnaire
| A Framework for Prenatal Detection of Risk Drinking* | ||
| T: | Tolerance | How many drinks does it take to make you feel high? (Positive = more than 2) |
| A: | Annoyed | Have people annoyed you by criticizing your drinking? |
| C: | Cut down | Have you felt you ought to cut down on your drinking? |
| E: | Eye-opener | Have you ever had an eye-opener drink first thing in the morning to steady your nerves or get rid of a hangover? |
* A positive answer to T alone or to two of A, C, or E can signal a problem with a high degree of probability, and positive answers to all four indicates great certainty of a problem.
From Sokol RJ, Martier SS, Ager JW: The T-ACE questions: Practical prenatal detection of risk-drinking, Am J Obstet Gynecol 160:863, 1989.
Box 3-5 The RAFFT Questionnaire
| A Framework for Detecting Substance Use Disorders in Adolescents | ||
| R: | Relax | Do you drink or take drugs to relax, feel better about yourself, or fit in? |
| A: | Alone | Do you ever drink or take drugs while you are alone? |
| F: | Friends | Do any of your closest friends drink or use drugs? |
| F: | Family | Does a close family member have a problem with alcohol or drugs? |
| T: | Trouble | Have you ever gotten into trouble from drinking or taking drugs? |
From Bastiaens L, Francis G, Lewis K: The RAFFT as a screening tool for adolescent substance use disorders, Am J Addict 9:10, 2000.
How can I narrow my diagnosis?
Key questions
 Is there a personal or family history of mental illness?
Is there a personal or family history of mental illness?
 Is there a family history of autism?
Is there a family history of autism?
 Over the past 2 weeks, have you felt down, depressed, or hopeless?
Over the past 2 weeks, have you felt down, depressed, or hopeless?
 Over the past 2 weeks, have you had little interest or pleasure in your daily activities?
Over the past 2 weeks, have you had little interest or pleasure in your daily activities?
 Do you tend to be an anxious or nervous person?
Do you tend to be an anxious or nervous person?
 Have you had periods of feeling so happy or energetic that your friends told you were talking too fast or that you were too “hyper”?
Have you had periods of feeling so happy or energetic that your friends told you were talking too fast or that you were too “hyper”?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree