Chapter 23 provides details of the admission assessment. Before arrival in the unit (unless it is an emergency admission) the client reports to the admitting department. Here a member of the clerical staff obtains and records information including the person’s full name; age; sex; marital status; religion; address; the name, address and telephone number of next of kin; and details about any hospital insurance. An identification band (Figure 24.1) is placed on the client’s wrist as a basic safety precaution against mistaken identity and treatment. Some facilities require clients to wear two identification bands, one on the wrist and one on the ankle. The person is advised whether to attend the X-ray or pathology department before admission to the unit. The individual is then escorted to the unit, where a nurse receives them.
The nurse who is responsible for admission to the unit should greet the client, and any accompanying relative or friend, in a warm and friendly manner. The nurse should address the person by name and introduce themselves, then escort the person to the room and begin the process of admission. Depending on the circumstances, a relative or friend may be present and may be offered a seat in a waiting area.
The admission procedure is basically the same in most health care facilities but will vary in detail in different settings, and in sequence, according to circumstances. The client is taken to the room and introduced to any other person in the room. If sharing a room, privacy must be ensured. The client is shown the general layout of the room and where to put personal belongings. It is important that the client is shown how to use the signal device, any fitted television or radio controls, and lights. The client’s identification band should be checked and compared with the card on the bed to see that they are correct. The client is shown the location of the bathroom, toilet, sitting room and telephones. Depending on circumstances, the client may remain in day clothes and be able to walk about the ward, or may be required to change into night clothes and get into bed.
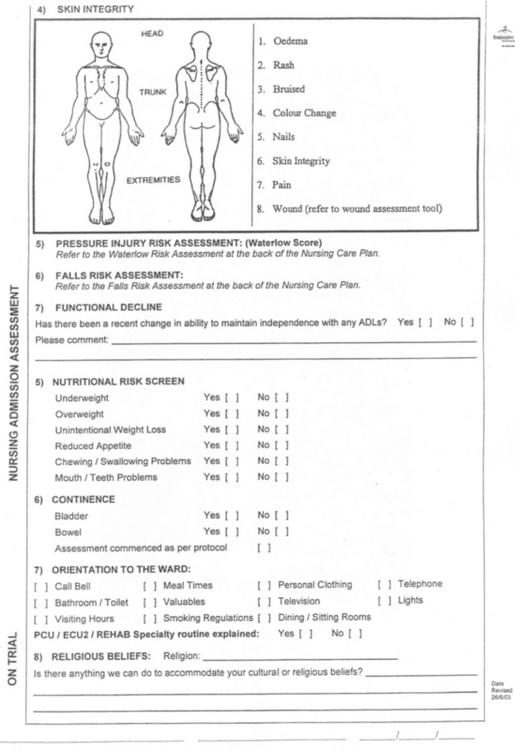
Although the client will have been advised not to bring valuable items, documentation is made of any personal effects. It is not generally necessary to itemise clothing, but a list is compiled of any items of value, such as a wristwatch, jewellery, television set, radio and money. Some health care facilities also require that documentation is made of any prosthesis, such as dentures, a hearing aid or artificial limb. If the client has a large sum of money they are advised to either send it home or to place it in the health care facility’s safe. A ‘valuables’ envelope is provided for the safe-keeping of money or valuable items. It is very important to inform the client that the health care facility does not accept responsibility for valuable items unless they are deposited in the safe. The nurse should refer to the facility’s policy regarding the procedure to be followed when the person’s valuables are to be stored.
Many health care facilities have a booklet that contains information about various aspects of the organisation. The booklet contains details such as visiting times; meal times; how to identify the various personnel; kiosk, telephone, television and laundry facilities available; regulations regarding smoking, and the time the individual is expected to vacate the room on discharge.
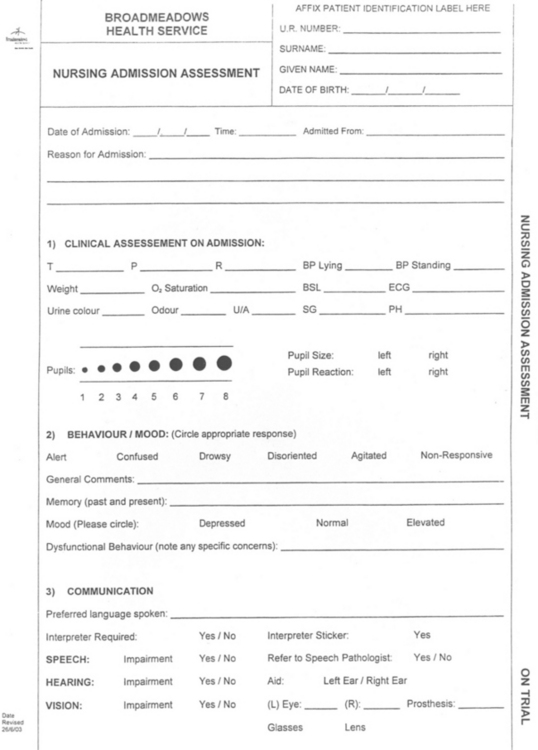
As soon as practicable, assessment is made of vital signs and weight, and the information documented. A sample of urine is obtained and urinalysis performed. (Information on vital signs and urinalysis are provided in Chapters 21 and 22.) The client’s height may also be measured and documented.
Throughout the admission procedure, the nurse should discreetly observe the client to gain information that will assist in planning care. Assessment is made, and documented (Figure 24.2), of the client’s:
At the time of admission or as soon as possible afterwards, a nursing history is compiled and a nursing care plan developed. (Information on these and other aspects of the nursing process are provided in Chapters 19 and 20.)
The client should be provided with a flask of fluid and offered a cup of tea or coffee, unless oral fluids are contraindicated. Anybody accompanying the client may also be offered a drink or shown where to find the kiosk. This is of particular importance if it is an emergency admission. The client’s significant others may be very distressed, and may appreciate being shown to an area where they can sit and rest for a while. The health care facility may also provide accommodation for the relatives if the client is very ill.
Before leaving the room the nurse should ensure that the client and significant others have been given all the information they require. The nurse should answer any questions or, if not able to, refer them to the nurse in charge. The nurse should also bear in mind that a person who is stressed tends not to hear or remember all the information given; therefore, ensure that the information is repeated whenever necessary.