. ADMINISTRATIVE PROCEDURES
Appointments6
Correspondence7
Filing12
Scheduling Admissions, diagnostic tests, and Procedures13
Bookkeeping Procedures14
Banking Procedures14
Collecting co-Payments and completing charge slips16
Entering charges in the Patient Account17
Petty cash19
Preparing reports20
Billing and collections20
Insurance Billing22
Preparing the insurance claim Form25
Resubmission of denied claims32
TELEPHONES
The telephone is often the first point of contact with a patient. Managing the telephone is one of the most important jobs in the medical office. Remember, a first impression, even on the telephone, happens only once.
INCOMING TELEPHONE CALLS
Incoming calls can be routed either to the proper person electronically or through the person who answers the phone.
Find out if the office wants you to pick up a ringing telephone or if the person assigned to answer the telephone should respond.
The medical assistant (MA) can handle some calls. Others must be routed to a physician or other licensed professional. If the physician is with a patient, take a message, making certain to record all needed information. Let the caller know approximately when the physician will return the call.
Calls are referred to a physician for the following reasons:
• To provide a patient with test results
• To receive a report of satisfactory or unsatisfactory progress from a patient
• To receive a call from another physician To answer medical questions from a patient
In some practices, requests for prescription renewals are also routed to a physician. In other offices, the MA may take a message, obtain a physician’s approval, and then “call in” the new prescription to the pharmacy.
“DO-NOTS” REGARDING INCOMING CALLS
• Do not interrupt a physician who is with a patient unless the call is from another physician. If the physician is in the middle of a procedure, do not interrupt; explain the situation to the physician who is calling and ask when the call can be returned.
• Do not place another physician on hold except for the purpose of transferring the call.
• Do not discuss a telephone call with a physician in front of a patient; speak to the physician over the telephone rather than over the open intercom. You may also give the physician a message slip.
If an emergency call comes in, follow the office policy for handling emergency calls, which may include the following:
• Remain calm.
• Never place the caller on hold.
• If possible, ask a physician or other licensed professional to take the call immediately. (Write a note and ask someone to take it to the physician, or have someone page the physician on another line.)
• Record all pertinent information about the caller and the person experiencing the emergency (e.g., name, telephone number, and address from which the call is coming).
• If you are alone, tell the person to go to a hospital emergency room. If the person does not have transportation or is too ill to drive, instruct the patient to call an ambulance (usually 9-1-1) or you call the ambulance.
• If you must call 9-1-1, use a different telephone if possible to avoid placing the emergency call on hold.
• If you called 9-1-1, continue to speak to the individual until you hear the emergency response team arrive.
• If the emergency is a poisoning, refer the caller to the local poison control hot line or call the poison hot line yourself.
• Document the exact date and time of the call, the instructions you gave, and your initials.
Problem calls include those from a person who refuses to give information about the purpose of the call, calls with complaints, and calls from a patient who has special problems.
If the caller refuses to give information about the purpose of the call:
• Ask if the person is an established patient to verify whether you should be giving any information to them at all.
• Explain that you need a name, telephone number, and purpose of the call so that you can ensure the proper person responds to the caller.
• Instruct the caller to write a letter if he or she does not wish to leave the necessary information for a return call.
• If the caller persists in refusing, it may be because she or he is embarrassed or unsure how to articulate what is really wrong. Write on the message note to the physician that the patient refused to state the reason for the call.
For the caller with a complaint or a patient with a special problem:
• Listen carefully, and be patient.
Appointment scheduling and appointment flow are factors in patient satisfaction. If you are asked to make appointments, either for patients in the office or over the telephone, determine the following:
• Time allotted for different types of visits (e.g., new patient, established patients, follow-up visits)
• Information needed from the patient who is making the appointment
• Particular preparation instructions for patients scheduling certain types of appointments (e.g., fasting laboratory tests)
• Type of appointment scheduling system the office uses (e.g., appointment book, computer) and whether the office “double-books”
DAILY APPOINTMENT SCHEDULE
If you are checking in patients when they arrive, remember that the daily appointment schedule is the office’s official, legal record. Any necessary changes (e.g., cancellations, no-shows, add-ins) should be made in red ink. Patient sign-in logs should be designed to ensure privacy; either individual sign-in sheets or peel-off labels are best.
SICK AND URGENT VISITS
Sometimes physicians will see patients who need urgent appointments. Determine whether urgent visits are worked into the schedule of the patient’s primary physician or if one physician is assigned to handle each day’s urgent visits.
Refer to the office’s procedures manual to determine what questions to ask to determine how serious the problem is and what type of appointment to offer. Know what are considered urgent symptoms at your facility.
CORRESPONDENCE
Medical offices generate a lot of correspondence, and preparing letters and envelopes may be your responsibility.
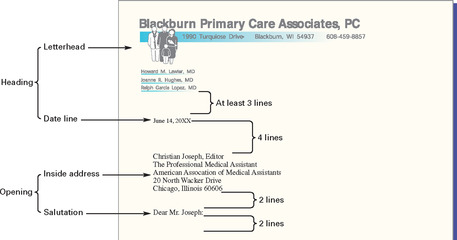
SECTIONS OF THE BUSINESS LETTER
The business letter has the following four sections:
1. Heading: Sender’s name and address
2. Opening: Date the letter is written, to whom the letter is being sent, and the greeting
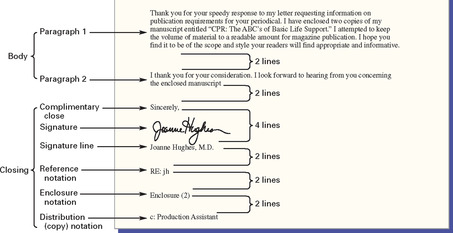
3. Body: Substance of the letter
4. Closing: Complimentary salutation, signature, signature line, and any reference notations (If you are keying letters from dictation or from a physician’s notes, the physician’s initials should be capitalized, followed by a backslash, and then your initials in lowercase.)
THINGS TO FIND OUT
If you are asked to prepare correspondence, find out the following:
• Where the office stationery supply (e.g., letterheads, envelopes) is stored and what letter format to use (e.g., block, modified block, semiblock, simplified)
• What complementary closing to use (e.g., sincerely, cordially, with best regards)
Ask the office manager or MA who is working with you as a mentor to see two or three old letters to follow as examples. Many offices use form letters or templates, which are filed in the computer and which require that only the patient’s name and other information (e.g., appointment date and time or outstanding amount of a bill) be inserted before mailing.
 |
 |
Block or full-block format— All lines are justified left and are ragged right.
Modified block format— The complimentary closing and signature line begin at a tab stop in the center or to the right of the center. All other lines are justified left and ragged right.
Semiblock format— Same as the modified block format, but the paragraphs are indented five spaces.
Simplified format— A subject line is typed in all capital letters and replaces the complimentary closing; the signature line is replaced by an all-capital-letter signature, five lines below the letter’s body.
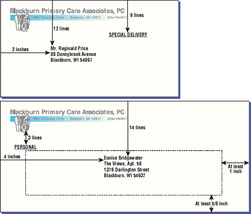
ENVELOPE
The envelope should have the return address in the upper left-hand corner. The name and address of the person to whom the letter is being sent should be centered, using all capital letters and no punctuation (except for a hyphen between the first five numbers and the last four numbers of the zip code + 4).
Any special instructions should be placed where they will not interfere with the postal service’s optical scanning equipment. The following figure shows examples of properly formatted envelopes.
The patient medical record is a legal document that records the care received or not received by a patient and must be maintained with care. Proper filing— whether the filing system is paper charts or electronic— is of utmost importance.
FILING RULES
Medical records are generally filed either alphabetically or by a numerical coding system. In a paper-based system, guides are used to separate folders into sections, and outguides are used to indicate where a file has been removed.
ALPHABETIC FILING
• Alphabetic filing uses legal names as the basis for determining where a file goes.
• The last name is the first filing unit (e.g., all Smith files are filed together, all Walker files are together).
• The first name becomes the second filing unit (e.g., Alan Walker is filed before Brittany Walker).
• The middle name is the third filing unit. The record of a patient with no middle name is filed before the record of a patient with the same last and first names and also a middle name.
• Hyphenated last names are filed under the first of the two last names; if last names are not hyphenated, the final name is considered the last name.
• Abbreviations are filed as if spelled out. Prefixes such as Mac-, Mc-, De, Van, and so on are usually considered to be part of the last name for filing purposes. Find out exactly how they are treated in any particular office.
• Each patient is given a unique identification number, and confidentiality is preserved.
• Numerical filing can be either consecutive or nonconsecutive (also called terminal digit filing).
• An alphabetical cross-reference system by which to locate a patient’s identification number should be set up.
LOCATING A FILE IN A PAPER-BASED FILING SYSTEM
The patient record (in a file folder) has to be located when the patient comes in for an office visit or when the patient calls the office with a question. The file should be located according to the office guidelines for filing.
If you remove a patient file from its location, place an outguide into where the record file was removed. Promptly return the file after it has been used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree