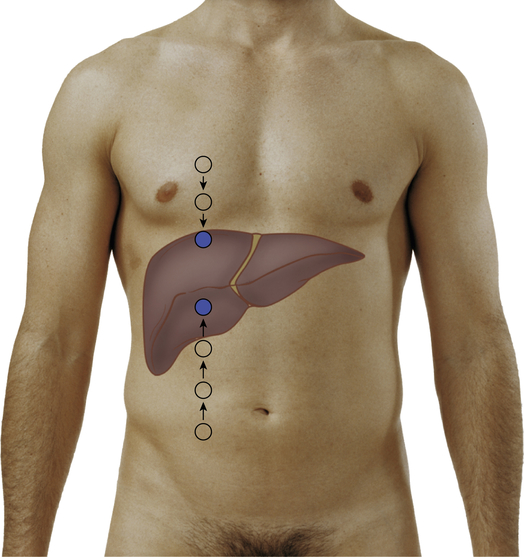
Percussion Notes of the Abdomen To determine lower liver border, percuss upward at right midclavicular line, as shown in figure on p. 138, and mark with a pen where tympany changes to dullness. To determine upper liver border, percuss downward at right midclavicular line from an area of lung resonance, and mark change to dullness. Measure the distance between marks to estimate vertical span. Place left hand under patient at eleventh and twelfth ribs, lifting to elevate liver toward abdominal wall. Place right hand on abdomen, fingers extended toward head with tips on right midclavicular line below level of liver dullness, as shown in figure at right. Alternatively, place right hand parallel to right costal margin, as shown in bottom figure at right. Press right hand gently but deeply in and up. Ask patient to breathe comfortably a few times and then take a deep breath. Feel for liver edge as diaphragm pushes it down. If palpable, repeat maneuver medially and laterally to costal margin. Still standing on right side, reach across patient with left hand, place it beneath patient over left costovertebral angle (CVA), and lift spleen anteriorly toward abdominal wall. As shown in figure at right, place right hand on abdomen below left costal margin and—using findings from percussion—gently press fingertips inward toward spleen while asking patient to take a deep breath. Feel for spleen as it moves downward toward fingers. Repeat with patient lying on right side, as shown in bottom figure at right, with hips and knees flexed. Press inward with left hand while using fingertips of right hand to feel edge of spleen.
Abdomen
Examination
Technique
Findings
Inspect abdomen
EXPECTED: Usual color variations, such as paleness or tanning lines. Fine venous network (venous return toward head above umbilicus, toward feet below umbilicus).
UNEXPECTED: Generalized color changes, such as jaundice or cyanosis. Glistening, taut appearance. Bluish periumbilical discoloration, bruises, other localized discoloration. Striae, lesions or nodules, a pearl-like enlarged umbilical node, scars.
EXPECTED: Flat, rounded, or scaphoid. Contralateral areas symmetric. Maximum height of convexity at umbilicus. Abdomen remains smooth and symmetric while patient holds breath.
UNEXPECTED: Umbilicus displaced upward, downward, or laterally or is inflamed, swollen, or bulging. Any distention (symmetric or asymmetric), bulges, or masses while breathing comfortably or holding breath.
EXPECTED: Smooth, even motion with respiration. Female patients mostly costal movement; male patients mostly abdominal. Pulsations often visible in upper midline in thin adults.
UNEXPECTED: Limited motion with respiration in male adults. Rippling movement (peristalsis) or marked pulsations.
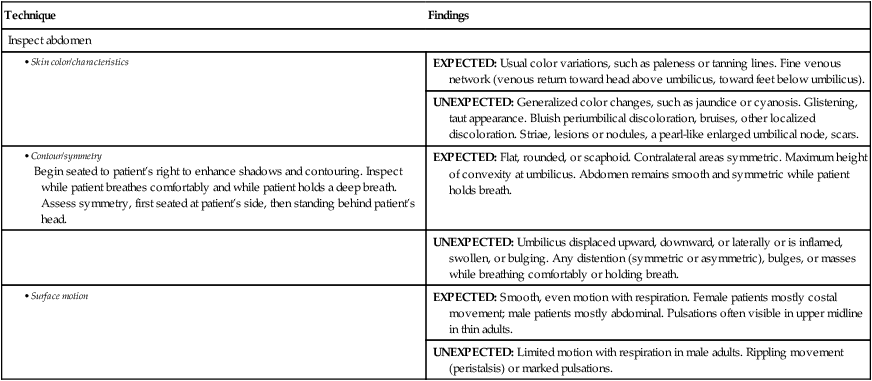
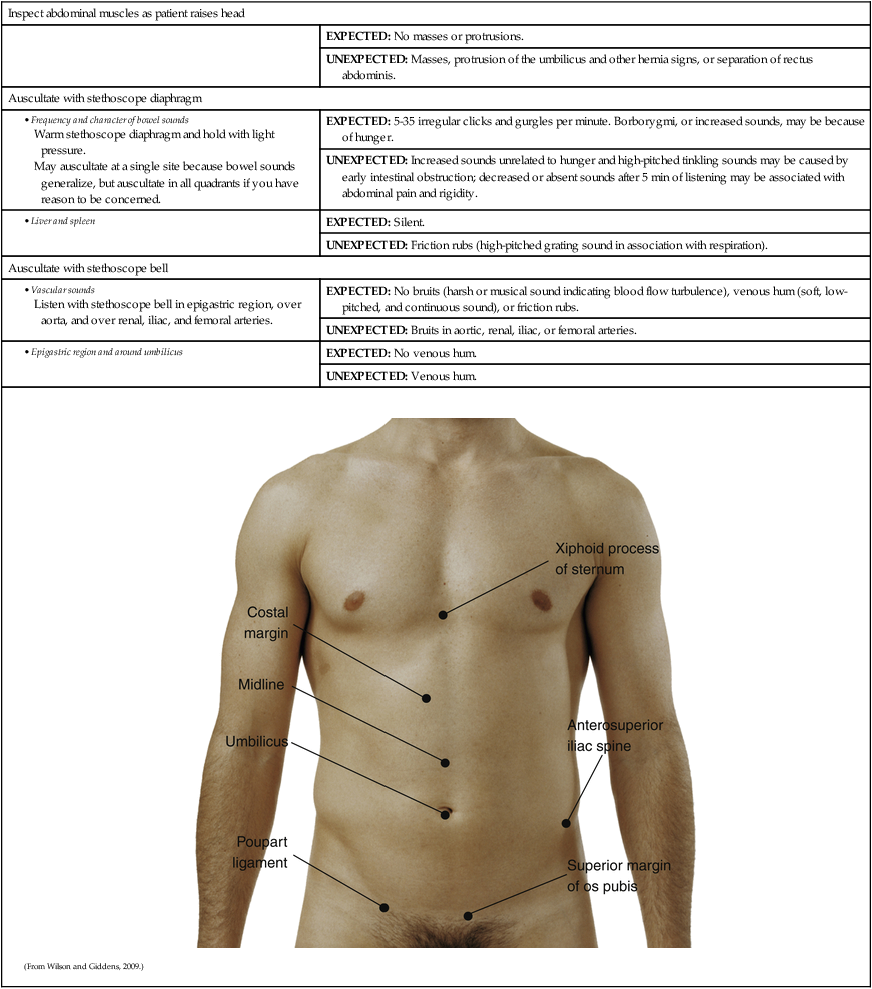
Inspect abdominal muscles as patient raises head
EXPECTED: No masses or protrusions.
UNEXPECTED: Masses, protrusion of the umbilicus and other hernia signs, or separation of rectus abdominis.
Auscultate with stethoscope diaphragm
EXPECTED: 5-35 irregular clicks and gurgles per minute. Borborygmi, or increased sounds, may be because of hunger.
UNEXPECTED: Increased sounds unrelated to hunger and high-pitched tinkling sounds may be caused by early intestinal obstruction; decreased or absent sounds after 5 min of listening may be associated with abdominal pain and rigidity.
EXPECTED: Silent.
UNEXPECTED: Friction rubs (high-pitched grating sound in association with respiration).
Auscultate with stethoscope bell
EXPECTED: No bruits (harsh or musical sound indicating blood flow turbulence), venous hum (soft, low-pitched, and continuous sound), or friction rubs.
UNEXPECTED: Bruits in aortic, renal, iliac, or femoral arteries.
EXPECTED: No venous hum.
UNEXPECTED: Venous hum.
Note
Description
Location
Tympany
Musical note of higher pitch than resonance
Over air-filled viscera
Hyperresonance
Pitch lies between tympany and resonance
Base of left lung
Resonance
Sustained note of moderate pitch
Over lung tissue and sometimes over abdomen
Dullness
Short, high-pitched note with little resonance
Over solid organs adjacent to air-filled structures
Technique
Findings
Percuss abdomen
Note: Percussion can be done independently or concurrently with palpation.
EXPECTED: Tympany predominant. Dullness over organs and solid masses. Dullness in suprapubic area from distended bladder. See table on p. 136 for percussion notes.
UNEXPECTED: Dullness predominant.
EXPECTED: Lower border usually begins at or slightly below costal margin. Upper border usually begins at fifth to seventh intercostal space. Span generally ranges from 6 to 12 cm in adults.
UNEXPECTED: Lower liver border >2-3 cm below costal margin. Upper liver border above the fifth or below the seventh intercostal space. Span <6 cm or >12 cm.
EXPECTED: Small area of dullness from sixth to tenth rib. Tympany before and after deep breath.
UNEXPECTED: Large area of dullness (check for full stomach or feces-filled intestine). Tone change from tympany to dullness with inspiration.
EXPECTED: Tympany of gastric air bubble (lower than intestine tympany).
UNEXPECTED: Dullness.
Lightly palpate abdomen
Stand at patient’s right side. Systematically palpate all quadrants, avoiding areas previously identified as problem spots. With palmar surface of fingers, depress abdominal wall up to 1 cm with light, even circular motion.
EXPECTED: Abdomen smooth with consistent softness. Possible tension from palpating too deeply, cold hands, or ticklishness.
UNEXPECTED: Muscular tension or resistance, tenderness, or masses. If resistance is present, place pillow under patient’s knees and ask patient to breathe slowly through mouth. Feel for relaxation of rectus abdominis muscles on expiration. Continuing tension signals involuntary response to localized or generalized rigidity.
Palpate abdomen with moderate pressure
Using same hand position as above, palpate all quadrants again, this time with moderate pressure.
EXPECTED: Soft, nontender
UNEXPECTED: Tenderness.
Deeply palpate abdomen
With same hand position as above, repeat palpation in all quadrants or regions, pressing deeply and evenly into abdominal wall. Move fingers back and forth over abdominal contents. Use bimanual technique—exerting pressure with top hand and concentrating on sensation with bottom hand, as shown in figure below—if obesity or muscular resistance makes deep palpation difficult. To help determine whether masses are superficial or intraabdominal, have patient lift head from examining table to contract abdominal muscles and obscure intraabdominal masses. 
EXPECTED: Possible sensation of abdominal wall sliding back and forth. Possible awareness of borders of rectus abdominis muscles, aorta, and portions of colon. Possible tenderness over cecum, sigmoid colon, and aorta and in midline near xiphoid process.
UNEXPECTED: Bulges, masses, tenderness unrelated to deep palpation of cecum, sigmoid colon, aorta, xiphoid process. Note location, size, shape, consistency, tenderness, pulsation, mobility, movement (with respiration) of any masses.
EXPECTED: Umbilical ring circular and free of irregularities. Umbilicus either slightly inverted or everted.
UNEXPECTED: Bulges, nodules, granulation. Protruding umbilicus.
EXPECTED: Usually liver is not palpable. If felt, liver edge should be firm, smooth, even.
UNEXPECTED: Tenderness, nodules, or irregularity. 

EXPECTED: Gallbladder not palpable.
UNEXPECTED: Palpable, tender. If tender (possible cholecystitis), palpate deeply during inspiration and observe for pain (Murphy sign).
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Abdomen
Get Clinical Tree app for offline access