A
Activated clotting time
Also called: (ACT); Activated Coagulation Time
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other venipuncture procedures (see Chapter 2), with the following additional measures.
During the test
Posttest
 Nursing response to critical values
Nursing response to critical values
The nurse keeps protamine sulfate on hand for use in case of hemorrhage. The action of protamine sulfate is to neutralize heparin, usually within 5 minutes after it is administered. If prescribed, this medication in its undiluted state is injected very slowly, intravenously. When protamine sulfate is administered, the nurse monitors the vital signs because if it is administered too rapidly, this medication can result in severe hypotension, bradycardia, and dyspnea. Thereafter, ACT values are monitored because of a potential heparin rebound effect that can occur several hours later. Protamine sulfate would lower the ACT value; a heparin rebound effect would again raise the ACT value.
Activated partial thromboplastin time
Also called: (APTT); Partial Thromboplastin Time (PTT)
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other venipuncture procedures (see Chapter 2), with the following additional measures.
Pretest
Posttest
 Nursing response to critical values
Nursing response to critical values
The nurse assesses the patient for spontaneous bleeding, oozing of blood, bruising, and petechiae. The nurse observes the skin, mucus membranes, and gingiva of the oral cavity, and the urine and stool for manifestations of bleeding. The vital signs are taken, observing for hypotension and tachycardia. The nurse asks the patient if he or she has a headache because this can be an early sign of an intracranial bleeding episode. Until the physician is contacted, the nurse must withhold the next dose of heparin.
Adrenocorticotropic hormone, plasma
Also called: (ACTH); Corticotropin
Basics the nurse needs to know
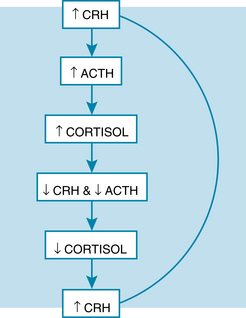
A negative feedback mechanism also regulates the hypothalamic-pituitary-adrenal hormonal responses. As the cortisol level increases in the plasma, it inhibits both ACTH secretion by the pituitary gland and CRH secretion by the hypothalamus (Figure 10). The nurse needs to be aware of the feedback inhibition of CRH and ACTH, which occurs with exogenous administration of glucocorticoids.
How the test is done
A venipuncture is done with chilled syringe and blood placed on ice and sent immediately to the lab.
Interfering factors
Adrenocorticotropic hormone stimulation test
Basics the nurse needs to know
ACTH is secreted by the pituitary gland. Its target organ is the adrenal cortex, where it stimulates the secretion of glucocorticoids, aldosterone, and androgens. Synthetic ACTH, known as cosyntropin (Cortrosyn), normally has the same effect. It causes an increase in adrenal cortex hormones. A normal response excludes the diagnosis of primary adrenocorticoid insufficiency, because the gland was able to respond. A normal response will also rule out complete ACTH deficiency (secondary adrenocorticoid failure) because complete lack of ACTH causes adrenal atrophy, and the gland is unable to respond.
Alanine aminotransferase
Also called: (ALT); Glutamic-Pyruvic Transaminase (SGPT)
Albumin, urinary
Also called: Protein Screen; Urine Screen for Albumin; Urinary Albumin, 24-hour collection
Purpose of the test
Urinary excretion of albumin is evaluated to assess renal function and to determine effectiveness of therapy in the management of urinary disease. Studies have shown that albumin in urine also can be used as a predictor of complications associated with diabetes mellitus.
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other urine collection procedures (see Chapter 2), with the following additional measures.
Posttest
Aldosterone, serum
Purpose of the test
The aldosterone level is used in the workup for hypertension and in the diagnosis of aldosteronism.
Basics the nurse needs to know
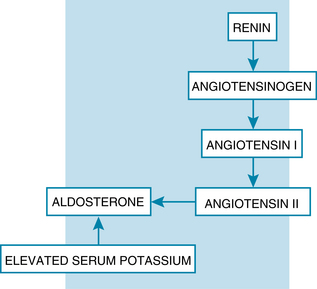
Aldosterone is a mineralocorticoid produced by the adrenal cortex and controlled primarily by the renin-angiotensin system. Renin secreted by the kidneys acts on angiotensinogen to convert it to angiotensin I. Later, angiotensin I is converted to angiotensin II. Angiotensin II stimulates the adrenal cortex to produce and secrete aldosterone. The aldosterone acts on the renal tubules to (1) increase sodium retention and thus increase fluid retention, which increases plasma fluid volume and blood pressure, and (2) to increase potassium excretion in urine (Figure 11).
REFERENCE VALUES*
Child
1 week-1 year: 1-160 ng/dL or SI: 0.03-4.43 nmol/L
1-3 years: 5-60 ng/dL or SI: 0.14-1.7 nmol/L
3-11 years: <5-80 ng/dL or SI: <0.14-2.22 nmol/L
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other venipuncture procedures (see Chapter 2), with the following additional measures.
During the test
Aldosterone, urinary
Basics the nurse needs to know
Aldosterone is a mineralocorticoid produced by the adrenal cortex. Its synthesis and release are controlled primarily by the renin-angiotensin system. Aldosterone acts on the renal tubules to resorb greater quantities of sodium, and therefore water, and increases the excretion of potassium into the urine. Elevated levels of urinary aldosterone may be caused by excess secretion of aldosterone by the adrenal glands, excessive secretion of renin, or conditions that result in decreased kidney perfusion.
How the test is done
Unlike serum aldosterone levels, positioning does not affect urinary aldosterone levels.
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other 24-hour urine collection procedures (see Chapter 2), with the following additional measures.
Pretest
During the test
Alkaline phosphatase
Basics the nurse needs to know
The ALP level will rise with increased activity from liver disease, biliary tract obstruction, or bone disease. In serious or advanced liver or bone disease, the ALP value can rise dramatically to 10 to 12 times the normal value. Additional transaminase enzyme tests can help identify the source of the ALP elevation. When the cause of an elevated ALP arises from liver disease, the alanine aminotransferase (ALT) and aspartate aminotransferase (AST) test results are also mildly elevated. With an elevated ALP result that is caused by bone disease, however, there is no associated elevation of the ALT or AST levels.
Allergy tests, skin
Also called: Skin prick or skin puncture test, Intradermal skin test
Basics the nurse needs to know
Allergens are substances in the environment that have the potential to cause an allergic reaction when they enter the body or touch the skin of a sensitized person (Box 4). Sensitization means that specific IgE antibodies are present, but an allergic reaction depends on other variables such as whether the individual comes in contact with that specific allergen. If an allergic reaction starts, there is a rapid release of Immunoglobin E (IgE) antibody and histamine from the mast cells and symptoms emerge. This response will continue until all allergens are destroyed by the IgE antibody and cleared from the body. Allergy skin testing is a very effective method to identify which allergen is the cause of the sensitivity reaction. There are several methods of skin testing available. The two methods discussed in this section are the skin prick method and the intradermal method. Each of these tests uses very small doses of antigens that are introduced into the skin; then the examiner measures the amount of allergic response. In addition, the patch skin test can be done by placing suspected allergens on the skin surface and measuring the allergic response from the contact. (See Patch Test on p. 480). Additionally, allergy testing may be done on a specimen of blood; it involves a quantitative measure of the IgE antibody response to specific allergens. (See Immunoglobin E Antibody on p. 394).
The skin prick method is preferred for the initial testing of the skin. It is safer because it causes fewer systemic reactions. This method can screen for a number of suspected allergens at the same time. The intradermal test method is more sensitive and accurate than the skin prick method. It is used in follow-up when a previously negative result occurs with the less sensitive skin prick method. It is also often used to test for an allergy to particular medications and for an allergy to insect venom, such as bee or wasp stings. There is a potential for a systemic reaction to the allergen that includes risk of anaphylaxis.
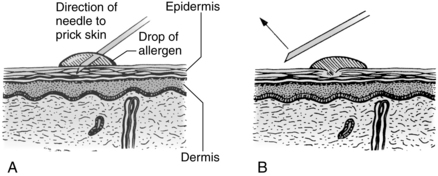
How the test is done
Skin prick method: A drop of commercially prepared antigen solution is placed on the test stylus device. The stylus device is pushed down gently to prick the skin and allow the allergen to barely penetrate the epidermis. The stylus may have a single point for single allergen testing, or it may be a multitest device with up to 10 points to test the corresponding number of different allergens. Alternatively, a droplet of allergen is placed on the skin and a very small sterile needle is used (Figure 12).
Interfering factors
NURSING CARE
Pretest
During the test
Alpha-fetoprotein
Also called: (AFP), α-fetoprotein; fetoprotein
Basics the nurse needs to know
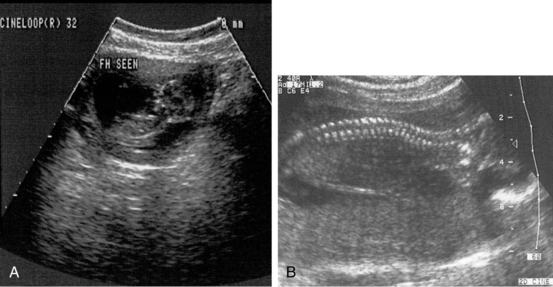
The gestational age is best measured by ultrasound. Often, however, the calculation is based on the mother’s estimate of when her last menstrual period occurred and this may not be precise. Because of the possibility of error, a positive screening test result is considered only suggestive of an abnormality in the fetus. Additional evaluation by ultrasound is recommended, and based on the results of the pregnancy ultrasound, amniocentesis may be needed. With a follow-up pregnancy ultrasound, the examination focus is on the fetal spine and cranium. With amniocentesis, the analysis of the amniotic fluid would provide accurate information about the condition of the fetus. Normal findings of these additional tests demonstrate that no neural tube defect exists (Figure 13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree