I. Definition
A. Sustained elevation of systolic blood pressure (SBP) of 140 mmHg or above, or of diastolic blood pressure (DBP) of 90 mmHg or above, at least three times on two different occasions
B. Includes individuals currently taking antihypertensive pharmacologic agents
II. Incidence/predisposing factors
A. Affects 20% to 30% of African Americans
B. Affects 10% to 15% of whites in the U.S.
C. Affects approximately 60 million Americans
D. Hypertension (HTN) is a leading risk factor for coronary artery disease, stroke, congestive heart failure, renal failure, and retinopathy.
III. Types and theories
A. Primary—referred to as “essential” or “idiopathic”
1. Cause is unknown.
2. Represents 95% of all cases of HTN
3. Onset is usually between ages 25 and 55.
4. Exacerbating factors
a. Obesity
b. Excessive alcohol consumption (more than two drinks a day)
c. Cigarette smoking
d. Use of nonsteroidal anti-inflammatory drugs
5. Theories of etiology include the following:
a. Genetic and environmental factors
c. Sympathetic nervous system hyperactivity
d. High renin-angiotensin activity causing vascular dysfunction
B. Secondary—related to other known causes or disease processes
1. Represents 5% of all cases of HTN
2. Etiology includes the following:
a. Estrogen use (via oral contraceptives or hormone replacement therapy)
b. Renal disease
c. Pregnancy
d. Endocrine disorders, such as pheochromocytoma
C. Isolated systolic HTN—common with aging
1. Poorly understood
2. May account for 65% to 75% of HTN in the elderly
3. SBP greater than 160 mmHg and DBP less than 90 mmHg
4. Effectively treated with diuretics and long-acting calcium channel blockers, among others
IV. Subjective and physical examination findings
A. Often none; known as the “silent killer”
B. Elevated blood pressure (140/90 mmHg or higher)
C. May complain of classic suboccipital “pulsating” headache, usually in the early morning and resolving throughout the day
D. May complain of epistaxis, light-headedness, and visual disturbances, among others
E. S4 heart sound may be present, related to left ventricular hypertrophy.
F. Retinal changes are present with severe, chronic disease.
G. Rare findings, such as hematuria
V. Diagnostics/laboratory testing
A. Laboratory data are usually unremarkable with uncomplicated disease.
B. Consider ordering the following:
1. CBC and electrolytes with hemoglobin levels (establish baseline)
2. Urinalysis
3. Blood urea nitrogen and creatinine concentrations
4. Fasting glucose level
5. Lipid panel
6. Electrocardiogram (Establish baseline, and rule out arrhythmias.)
7. Chest x-ray (Rule out cardiomegaly, for example.)
8. Echocardiogram (if left ventricular hypertrophy is suspected)
9. Angiotensin-converting enzyme (ACE) inhibitor (Captopril) stimulation test (if indicated, to rule out renovascular HTN)
10. Overnight 1-mg dexamethasone suppression test (if indicated to rule out Cushing’s syndrome)
11. Aldosterone level (if indicated, to rule out aldosteronism)
12. Plasma catecholamine level (if indicated, to rule out pheochromocytoma)
VII. Follow-up recommendations for initial hypertensive measurements
| *If systolic and diastolic categories are different, follow recommendations for shorter follow-up (e.g., 160/86 mmHg should be evaluated and referred to a source of care within 1 month). | ||
| †Modify the scheduling of follow-up according to reliable information about past blood pressure measurements, other cardiovascular risk factors, or target organ disease. | ||
| ‡Provide advice about lifestyle modifications. | ||
| Initial blood pressure, mmHg* | ||
|---|---|---|
| Systolic | Diastolic | Follow-up recommended† |
| Less than 120 | Less than 80 | Recheck in 2 years. |
| 120-139 | 80-89 | Recheck in 1 year. † |
| 140-159 | 90-99 | Confirm within 1-2 months. ‡ |
| 160-179 | 100-109 | Evaluate or refer to source of care within 1 month. |
| 180 or greater | 110 or greater | Evaluate or refer to source of care immediately or within 1 week, depending on clinical situation. |
VIII. Management
Get Clinical Tree app for offline access

A. Principle—in sequential order
1. Analyze baseline studies.
2. See algorithm for the treatment of HTN (Figure 9-1).
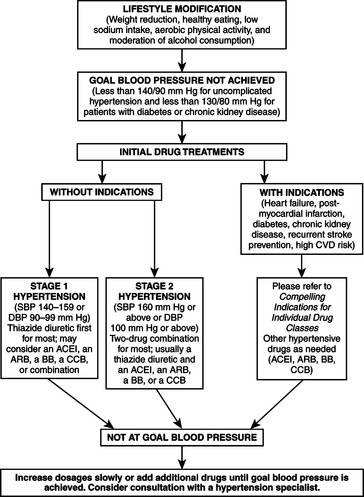 |
| FIGURE 9-1Algorithm for treatment of hypertension. DBP, Diastolic blood pressure; SBP, systolic blood pressure; ACEI, ACE inhibitor; A2RA, angiotensin II receptor agonist; B, beta blocker; CCB, calcium channel blocker.(From National Institutes of Health: Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, Bethesda, Md, NIH, 2003. Publication #03-5231.)NIH |
3. Use nonpharmacologic strategies.
4. Employ pharmacologic measures.
B. Nonpharmacologic strategies
1. Restriction of dietary sodium (no more than 100 mmol per day—2.4 g sodium or 6 g salt)
2. Weight loss, if overweight
4. Exercise (aerobic exercise 30-45 minutes each day on most days of the week)
5. Stress management planning
6. Reduction or elimination of alcohol consumption (fewer than two drinks daily for men, or one drink daily for women and lighter-weight persons)
7. Smoking cessation
8. Maintenance of adequate potassium, calcium, and magnesium intake
C. Pharmacologic measures




1. Based on degree of blood pressure elevation and/or the presence of end-organ damage, cardiovascular disease, or other risk factors
2. Goal of therapy—to prescribe the least number of medications possible at the lowest dosage to attain acceptable blood pressure, thereby decreasing cardiovascular and renal morbidity and mortality
3. Special considerations
a. Neither age nor gender usually affects agent responsiveness.
b. Thiazide-type diuretics are usually recommended for first-line treatment.
c. Beta blockers, ACE inhibitors, adrenergic receptor blockers, and calcium channel blockers are also useful alone or in combination therapy.
d. Table 9-3 may be helpful to the clinician in making prudent pharmacologic choices.
| Indication | Initial drug options |
|---|---|
| Diabetes | Diuretics, beta blockers, ACE inhibitors, angiotensin-receptor blockers, calcium channel blockers |
| Chronic kidney disease | ACE inhibitors, angiotensin-receptor blockers |
| Recurrent stroke prevention | Diuretics, ACE inhibitors |
| High cardiovascular disease (CVD) risk | Diuretics, beta blockers, ACE inhibitors, calcium channel blockers |
| Heart failure | Diuretics, beta blockers, ACE inhibitors, angiotensin-receptor blockers, aldosterone antagonist |
| Post myocardial infarction | Beta blockers, ACE inhibitors, aldosterone antagonist |
4. Refer to examples of commonly prescribed preparations in Table 9-4.
| Oral hypertensive drugs | |||
|---|---|---|---|
| Drug | Trade name | Dose | Frequency, days |
| Thiazide diuretics | |||
| Chlorothiazide | Diuril | 125-500 | 1-2 |
| Chlorthalidone | Generic | 12.5-25 | 1 |
| Hydrochlorothiazide | Microzide, HydroDIURIL | 12.5-50 | |
| Indapamide | Lozol | 1.25-2.5 | 1 |
| Polythiazide | Renese | 2-4 | 1 |
| Metolazone | Mykrox | 0.5-1 | 1 |
| Zaroxolyn | 2.5-5 | 1 | |
| Loop diuretics | |||
| Bumetanide | Bumex | 0.5-2 | 2 |
| Furosemide | Lasix | 20-80 | 2 |
| Torsemide | Demadex | 2.5-10 | 1 |
| Potassium-sparing diuretics | |||
| Amiloride | Midamor | 5-10 | 1-2 |
| Triamterene | Dyrenium | 50-100 | 1-2 |
| Aldosterone receptor blockers | |||
| Eplerenone | Inspra | 50-100 | 1 |
| Spironolactone | Aldactone | 25-50 | 1 |
| Beta blockers | |||
| Acebutolol | Sectral | 200-800 | 2 |
| Atenolol | Tenormin | 25-100 | 1 |
| Betaxolol | Kerlone | 5-20 | 1 |
| Bisoprolol | Zebeta | 2.5-10 | 1 |
| Metoprolol | Lopressor | 50-100 | 1-2 |
| Metoprolol extended-release | Toprol XL | 50-100 | 1 |
| Nadolol | Corgard | 40-120 | 1 |
| Penbutolol | Levatol | 10-40 | 1 |
| Pindolol | Generic | 10-40 | 2 |
| Propranolol | Inderal | 40-160 | 2 |
| Propranolol long-acting | Inderal LA | 60-180 | 1 |
| Timolol | Blocadren | 20-40 | 2 |
| Combined alpha and beta blockers | |||
| Carvedilol | Coreg | 12.5-50 | 2 |
| Labetalol | Normodyne, Trandate | 200-800 | 2 |
| ACE inhibitors | |||
| Benazepril | Lotensin | 10-40 | 1 |
| Captopril | Capoten | 25-100 | 2 |
| Drug | Trade name | Dose | Frequency,days |
| Enalapril | Vasotec | 5-40 | 1-2 |
| Fosinopril | Monopril | 10-40 | 1 |
| Lisinopril | Prinivil, Zestril | 10-40 | 1 |
| Moexipril | Univasc | 7.5-30 | 1 |
| Perindopril | Aceon | 4-8 | 1 |
| Quinapril | Accupril | 10-80 | 1 |
| Ramipril | Altace | 2.5-20 | 1 |
| Trandolapril | Mavik | 1-4 | 1 |
| Angiotensin II antagonists | |||
| Candesartan | Atacand | 8-32 | 1 |
| Eprosartan | Teveten | 400-800 | 1-2 |
| Irbesartan | Avapro | 150-300 | 1 |
| Losartan | Cozaar | 25-100 | 1-2 |
| Olmesartan | Benicar | 20-40 | 1 |
| Telmisartan | Micardis | 20-80 | 1 |
| Valsartan | Diovan | 80-320 | 1-2 |
| Calcium channel blockers | |||
| Amlodipine | Norvasc | 2.5-10 | 1 |
| Diltiazem | Cardizem CD, Dilacor XR,Tiazac | 180-420 | 1 |
| Diltiazem extended release | Cardizem LA | 120-540 | 1 |
| Felodipine | Plendil | 2.5-20 | 1 |
| Isradipine | Dynacirc CR | 2.5-10 | 2 |
| Nicardipine sustained release | Cardene SR | 60-120 | 2 |
| Nifedipine long-acting | Adalat CC, Procardia XL | 30-60 | 1 |
| Nisoldipine | Sular | 10-40 | 1 |
| Verapamil | Covera HS, Verelan PM | 120-360 | 1 |
| Verapamil immediate release | Calan,Isoptin | 80-320 | 2 |
| Verapamil long acting | Calan SR, Isoptin SR | 120-480 | 1-2 |
| Alpha1 blockers | |||
| Doxazosin | Cardura | 1-16 | 1 |
| Prazosin | Minipress | 2-20 | 2-3 |
| Terazosin | Hytrin | 1-20 | 1-2 |
| Central alpha2 agonists and other centrally acting drugs | |||
| Clonidine | Catapres | 0.1-0.8 | 2 |
| Clonidine patch | Catapres-TTS | 0.1-0.3 | 1 weekly |
| Methyldopa | Aldomet | 250-1000 | 2 |
| Reserpine | Generic | 0.1-0.25 | 1 |
| Guanfacine | Tenex | 0.5-2 | 1 |
| Direct vasodilators | |||
| Hydralazine | Apresoline | 25-100 | 2 |
| Minoxidil | Loniten | 2.5-80 | 1-2 |
| Combination drugs for hypertension | |||
| Drug | Trade name | Dose combinations, mg | |
| ACE inhibitors and calcium channel blockers | |||
| Amlodipine-Benazepril | Lotrel | 2.5/10, 5/10, 5/20, 10/20 | |
| Hydrochloride | |||
| Enalapril-Felodipine | Lexxel | 5/5 | |
| Trandolapril-Verapamil | Tarka | 2/180, 1/240, 2/240, 4/240 | |
| ACE inhibitors and diuretics | |||
| Benazepril-Hydrochlorothiazide | Lotensin HCT | 5/6.25, 10/12.5, 20/12.5, 20/25 | |
| Captopril-Hydrochlorothiazide | Capozide | 25/15, 25/25, 50/15, 50/25 | |
| Enalapril-Hydrochlorothiazide | Vaseretic | 5/12.5, 10/25 | |
| Fosinopril-Hydrochlorothiazide | Monopril/HCT | 10/12.5, 20/12.5 | |
| Lisinopril-Hydrochlorothiazide | Prinzide, Zestoretic | 10/12.5, 20/12.5, 20/25 | |
| Moexipril-Hydrochlorothiazide | Uniretic | 7.5/12.5, 15/25 | |
| Quinapril-Hydrochlorothiazide | Accuretic | 10/12.5, 20/12.5, 20/25 | |
| Angiotensin receptor blockers and diuretics | |||
| Candesartan-Hydrochlorothiazide | Atacand | 16/12.5, 32/12.5 | |
| Eprosartan-Hydrochlorothiazide | Teveten-HCT | 600/12.5, 600/25 | |
| Irbesartan-Hydrochlorothiazide | Avalide | 150/12.5, 300/12.5 | |
| Losartan-Hydrochlorothiazide | Hyzaar | 50/12.5, 100/25 | |
| Olmesartan Medoxomil- | Benicar-HCT | 20/12.5, 40/12.5, | |
| Hydrochlorothiazide | 40/25 | ||
| Telmisartan-Hydrochlorothiazide | Micardis-HCT | 40/12.5, 80/12.5 | |
| Valsartan-Hydrochlorothiazide | Diovan-HCT | 80/12.5, 160/12.5, 160/25 | |
| Beta blockers and diuretics | |||
| Atenolol-Chlorthalidone | Tenoretic | 50/25, 100/25 | |
| Bisoprolol-Hydrochlorothiazide | Ziac | 2.5/6.25, 5/6.25, 10/6.25 | |
| Metoprolol-Hydrochlorothiazide | Lopressor HCT | 50/25, 100/25 | |
| Nadolol-Bendroflumethiazide | Corzide | 40/5, 80/5 | |
| Propranolol LA-Hydrochlorothiazide | Inderide LA | 40/25, 80/25 | |
| Timolol-Hydrochlorothiazide | Timolide | 10/25 | |
| Centrally acting drugs and diuretics | |||
| Methyldopa-Hydrochlorothiazide | Aldoril | 250/15, 250/25, 500/30, 500/50 | |
| Reserpine-Chlorthalidone | Demi-Regroton, Regroton | 0.125/25, 0.25/50 | |
| Reserpine-Chlorothiazide | Diupres | 0.125/250, 0.25/500 | |
| Reserpine-Hydrochlorothiazide | Hydropres | 0.125/25, 0.125/50 | |
| Double diuretics | |||
| Amiloride-Hydrochlorothiazide | Moduretic | 5/50 | |
| Spironolactone-Hydrochlorothiazide | Aldactazide | 25/25, 50/50 | |
| Triamterene-Hydrochlorothiazide | Dyazide, Maxzide | 37.5/25, 75/50 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
