Kathleen F. Jett
Safe medication use
THE LIVED EXPERIENCE
It is so hard to keep track of my medications. I try arranging them in little cups to take with each meal, but then there are the ones that I take at odd times. Those are the easiest to forget. I get really confused and think sometimes I have taken them twice and then think I must be going crazy. I really wish I didn’t have to take so many pills, but I’m not sure what would happen if I stopped any of them. I don’t even know why I’m taking most of them.
Geraldo, hypertensive, diabetic, and having cardiac problems
Learning objectives
Upon completion of this chapter, the reader will be able to:
• Explain age-related pharmacokinetic changes.
• Discuss potential use of chronotherapy.
• Describe drug use patterns and their implications for the older adult.
• Explain the roles of elder, caregiver, and social network in reducing medication misuse.
• List interventions that can help promote medication adherence by the elder.
• Identify diagnoses or symptoms for which psychotropic drugs are prescribed.
• Discuss issues concerning psychotropic medication management in the older population.
• Develop a nursing care plan for patients prescribed psychoactive medications.
Glossary
Adverse reaction A harmful, unintended reaction to a drug.
Bioavailability The amount of drug that becomes available to effect changes in target tissues.
Biotransformation A series of chemical alterations of a drug occurring in the body.
Half-life The time it takes after administration to inactivate half of a drug.
Iatrogenic A result of something that is done or given to a person in the context of providing care.
Regimen A scheduled plan for the taking of medications, such as twice a day, with food, etc.
Side effect A consequence of a drug or procedure other than that for which it is used (e.g., dry mouth).
Target tissue Tissue or organ intended to receive the greatest concentration of a drug or to be most affected by the drug.
Therapeutic window The range of the plasma concentration of a drug within which it is safe and effective.
![]() evolve.elsevier.com/Ebersole/gerontological
evolve.elsevier.com/Ebersole/gerontological
In the United States, persons 65 years of age and older are the largest users of prescription and over-the-counter (OTC) medications; with the number of medications taken increasing with age. Making up only 13% of the population, they consume 33% of the prescribed medications or a range somewhere between 0 and 13 prescription drugs per person, and about 40% of OTC medications or other supplements such as herbs (Steinman et al., 2006; Gallagher et al., 2007; Brandt, 2010). Ninety percent of the persons at least 65 years of age take at least 1 drug a week, over 40% take at least 5, and 12% use at least 10 different drugs every week. Residents of long-term care facilities take the most medications of all, typically 7 to 8 different ones (Ruscin, 2009; Brandt, 2010). Elders accumulate prescriptions as they accumulate chronic diseases and number of health care providers (Green et al., 2007).
Unfortunately, the number of adverse drug reactions increases with the number of medications used. Adverse drug reactions (ADRs) have been found to be a notable cause for hospitalization as well as a cause of iatrogenic mortality and morbidity for those already hospitalized. This has been found to occur not only in the United States but in countries across the globe.
How elders use their prescribed medicines and other bioactive products depends on many factors related to the person’s own unique characteristics, situations, beliefs, understanding about illness, functional and cognitive status, perception of the necessity of the drugs, severity of symptoms, reactions to the medications, finances, access, and alternatives, and the compatibility of such products with their lifestyle. From the perspective of Maslow’s Hierarchy of Needs, drugs impinge on all levels. When used appropriately, prescription medications can afford basic survival or even enhance one’s quality of life and help achieve self-actualization for those with chronic conditions and disabilities. When they are used inappropriately, they threaten even the most basic level of physiological stability. Yet, at times, even when drugs are used appropriately, they may adversely affect the elder’s health and well-being.
Gerontological nurses have a responsibility to help minimize the risks and maximize the safety of medication use in the persons who receive their care. A review of the changes in pharmacokinetics, pharmacodynamics, and issues in drug use are presented in this chapter. The final section deals with the use of psychotropic agents. These are frequently prescribed to frail elders with the potential for both great benefit and significant risk and require special attention.
Pharmacokinetics
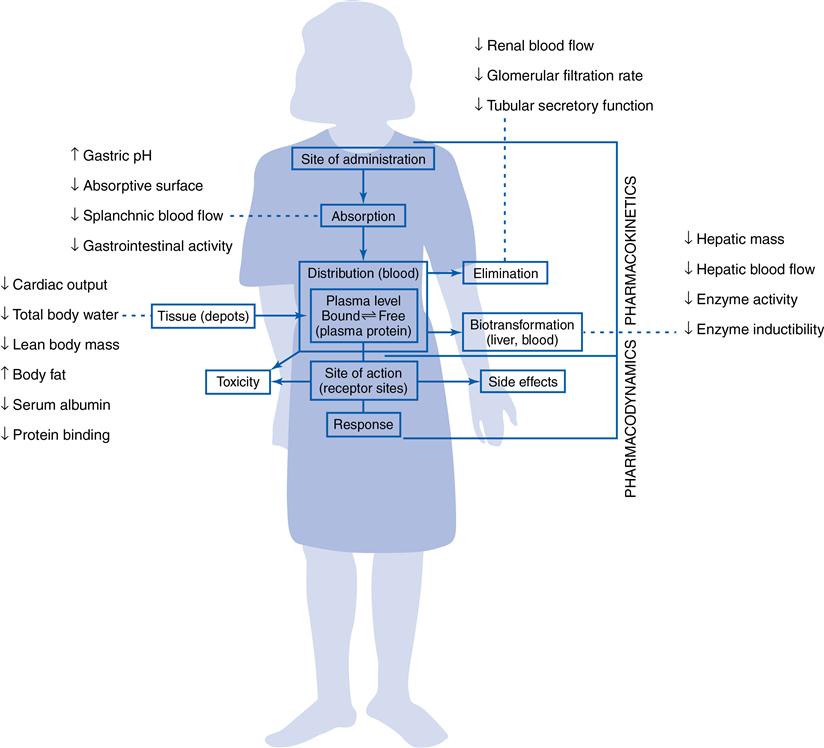
The term pharmacokinetics refers to the movement of a drug in the body from the point of administration as it is absorbed, distributed, metabolized, and finally, excreted. There is no conclusive evidence of an appreciable change in overall pharmacokinetics with aging; however, there are several changes with aging (see Chapter 5) that may have an effect (Figure 8-1). This chapter is not intended to replace a pharmacology text, but to supplement it for the key points of intersection between safe medication use and the aging process.
Absorption
For a drug to be effective it must be absorbed into the blood stream. The amount of time between the administration of the drug and its absorption depends on a number of factors, including the route of introduction (i.e., intravenous, oral, parenteral, transdermal, or rectal), bioavailability, and the amount of drug that passes into the body. The drug is delivered immediately to the blood stream with administration by intravenous route, and quickly with parenteral and transdermal routes and through mucous membranes such as the rectum and the oral mucosa. Orally administered drugs are absorbed the most slowly through the gastrointestinal tract.
Several normal age-related physiological changes have implications for differences in both the prescribing and the administration of medications for older adults (Table 8-1). The commonly seen increased gastric pH will retard the action of acid-dependent drugs. Delayed stomach emptying may diminish or negate the effectiveness of short-lived drugs that could become inactivated before reaching the small intestine. The absorption of some enteric-coated medications, such as enteric-coated aspirin, which are specifically meant to bypass stomach absorption, may be delayed so long that their action begins in the stomach and may produce gastric irritation or nausea. Absorption is also influenced by changes in gastrointestinal motility. If there is increased motility in the small intestine, drug effect is diminished because of shortened contact time and therefore decreased absorption and effectiveness. Conversely, slowed intestinal motility can increase the contact time and therefore the amount absorbed and the drug’s effect. This increases the risk for adverse reactions or unpredictable effects.
TABLE 8-1
Interaction of Aging and Drug Response, Select Medications
| Class | Drug | Effect of Aging |
| Analgesic | Morphine | ↑ analgesia |
| Anticoagulant | Warfarin (Coumadin) | ↑ blood time |
| Bronchodilator | Albuterol | ↓ bronchodilation |
| Cardiovascular agents | ACE IIs Enalapril Diltiazem Verapamil | ↑ BP reduction ↑ BP reduction ↑ acute reduction in BP ↑ acute reduction in BP |
| Diuretic | Furosemide (Lasix) | ↓ maximum response |
| Other | Levodopa | ↑ side effects |
From Ruscin JM: Drug therapy in the elderly. In The Merck manual for health professionals – Epub. Last updated September 2009. Available at http://www.merckmanuals.com/professional/geriatrics/drug_therapy_in_the_elderly/drug-related_problems_in_the_elderly.html#v1133742.
Many medications commonly taken by older adults can also affect the absorption of other drugs. Antispasmodic drugs slow gastric and intestinal motility. In some instances the ingested drug’s action may be useful, but when there are other medications involved, it is necessary to consider the problem of drug absorption alterations due to drug-drug interaction. Antacids or iron preparations affect the availability of some drugs for absorption by binding the drug with elements and forming chemical compounds. Drug-food interactions may either decrease or increase the amount absorbed. For example when a bisphosphonate such as Fosamax is taken with food of any kind, the absorption is reduced to only a few milligrams, and therefore the drug has no effect on the target organ, the bones; if thyroxin is taken at the same time as any compounds such as calcium or magnesium, it is inactivated.
Distribution
When a drug is absorbed it must be transported to the receptor site on the target organ to have any effect. Distribution depends on the availability of plasma protein in the form of lipoproteins, globulins, and especially albumin. As drugs are absorbed, they bind with the protein and are distributed throughout the body. Normally, a predictable percentage of the absorbed drug is inactivated as it is bound to the protein. The remaining free drug is available in the blood stream and has therapeutic effect when an effective concentration is reached in the plasma. Many older adults have an insignificant reduction in the serum albumin level. In others, especially those with prolonged illness or malnutrition (such as residents in skilled nursing facilities), the serum albumin may become dramatically diminished. When this occurs, toxic levels of available free drug may accumulate unpredictably, especially of highly protein-bound medications with narrow therapeutic windows, such as phenytoin and warfarin (Ruscin, 2009).
Potential alterations of drug distribution in late life are related to changes in body composition, particularly decreased lean body mass, increased body fat, and decreased total body water (see Figure 8-1). Decreased body water leads to higher serum levels of water-soluble drugs, such as lithium, digoxin, ethanol, and aminoglycosides. Increased serum levels increase the risk for toxicity. Adipose tissue nearly doubles in older men and increases by one half in older women; therefore drugs that are highly lipid-soluble are stored in the fatty tissue, extending and possibly elevating the drug effect (Masoro & Austed, 2003). This affects drugs such as lorazepam, diazepam, chlorpromazine, phenobarbital, and haloperidol (Haldol).
Metabolism
Biotransformation or metabolism, is the process by which the body modifies the chemical structure of the drug. Through this process the compound is converted to a metabolite that is later more easily excreted. A drug will continue to exert a therapeutic effect as long as it remains in either its original state or as an active metabolite. Active metabolites retain the ability to have a therapeutic effect, as well as the same or a greater chance of causing adverse effects. For example, the metabolites of acetaminophen (Tylenol) can cause liver damage with higher dosages (> 4 g/24 hr or more than four extra-strength products). The duration of drug action is determined by the metabolic rate and is measured in terms of half-life, or how long the drug remains active in the body.
A number of enzymes play an active part in drug metabolism. Among these are a group known as the cytochrome P450 (CYP450) monooxygenase system. The system is made up of about 50 isoforms, each of which has the potential to metabolize a drug by adding or subtracting part of the drug molecule. When this occurs the drug can be dramatically changed from its original state or even its intended effect. While age does not appear to affect the functioning of the CYP450 system, we now know that genetics have a great effect (Box 8-1).
The liver is the primary site of drug metabolism. With aging, the liver’s activity, mass, volume, and blood flow are reduced and hepatic clearance may decrease by up to 30% to 40% (Ruscin, 2009). These changes result in a potential decrease in the liver’s ability to metabolize drugs such as benzodiazepines (e.g., the tranquilizer lorazepam [Ativan]) (Table 8-2). These changes result in a significant increase in the half-life of these drugs. For example, the half-life of diazepam (Valium) in a younger adult is about 37 hours, but in an older adult extends to as long as 82 hours. If the dose and timing are not adjusted, the drug can accumulate, and the administration of a single dose can have significantly more effects (and longer) than in a younger person. Except in the rarest of circumstances Valium should not be used because of this (American Geriatrics Society [AGS], 2012).
TABLE 8-2
Drugs to Watch: Examples of Commonly Used Medications Affected by Normal Changes with Aging
| Class or category | Affected by Decreased Hepatic Metabolism | Affected By Decreased Renal Excretion |
| Analgesic/antiinflamatory | Ibuprofen (Advil) Naproxen (Aleve) Morphine | |
| Antibiotics | Cipro | |
| Macrobid | ||
| Cardiovascular | Amlodipine (Norvasc) | Captopril (Capoten) |
| Diltiazem (Cardizem) | Digoxin (Lanoxin) | |
| Verapamil (Calan) | Enalapril (Vasotec) | |
| Lisinopril (Zestril) | ||
| Diuretics | Furosemide (Lasix) | |
| HCTZ | ||
| Others | Levodopa | Glyburide |
| Ranitidine (Axid) | ||
| Psychoactive drugs | Alprazolam (Xanax) | Risperidone |
| Diazepam (Valium) | ||
| Trazadone |
From Ruscin JM: Drug therapy in the elderly. In The Merck manual for health professionals – Epub. Last updated September 2009. Available at http://www.merckmanuals.com/professional/geriatrics/drug_therapy_in_the_elderly/drug-related_problems_in_the_elderly.html#v1133742.
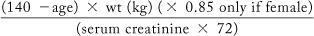
Excretion
Drugs and their metabolites are excreted in sweat, saliva, and other secretions but primarily through the kidneys. However, because kidney function declines significantly in aging (up to 50% decrease by the time one is 80 years of age), so does the ability to excrete or eliminate drugs in a timely manner (see Table 8-2). The considerably decreased glomerular filtration rate leads to prolongation of the half-life of drugs, or the amount of time required to eliminate the drug, again presenting opportunities for accumulation and increasing the potential for toxicity or other adverse events. Although renal function is highly individualized and cannot be estimated by the serum creatinine level, we approximate it by calculating the creatinine clearance (see equation). Reductions in dosages for drugs excreted by the kidneys (e.g., allopurinol, vancomycin) are needed when the creatinine clearance is reduced. Reductions in dosages may also be needed when the patient is very ill or dehydrated.
Estimated creatinine clearance (the Cockcroft-Gault equation):
For alternative calculations, see http://nkdep.nih.gov/professionals/gfr_calculators.
Pharmacodynamics
Pharmacodynamics refers to the interaction between a drug and the body (see Figure 8-1). The older the person gets, the more likely there will be an altered or unreliable response of the body to the drug. Although it is not always possible to explain the change in response, several mechanisms are known. For example, the aging process causes a decreased response to beta-adrenergic receptor stimulators and blockers; decreased baroreceptor sensitivity; and increased sensitivity to a number of medications, especially anticholinergics, benzodiazepines, narcotic analgesics, warfarin (Coumadin), and the cardiac drugs diltiazem and verapamil (Briggs, 2005). If food-drug interactions occur, the problems are worsened. For example, drinking grapefruit juice at the same time as one takes a “statin” such as Lipitor or any number of antibiotics may cause an unreliable response. There is also a growing body of knowledge about the interaction of herbal preparations and currently prescribed medications (Table 8-3). For example, ginkgo biloba is commonly thought to enhance cognitive function. However, it will increase the potential for bleeding when an anticoagulant such as Coumadin is used at the same time (Youngkin, 2012). In addition to the expected dry mouth, drugs with anticholinergic properties can cause confusion, constipation, blurred vision, orthostatic hypotension, urinary retention, or heat stroke, even at low doses (Ruscin, 2009). The use of benzodiazepines is associated with an increased risk for accidental injury, and they are on the “do-not-use” list for older adults (AGS, 2012).
TABLE 8-3
Selected Herb-Medication and Herb-Disease Interactions
| Herb | Medication | Complication | Nursing Action |
| Chamomile | Warfarin | May increase risk of bleeding | Advise to avoid teas and other products which contain the product |
| Garlic | Warfarin or any anticoagulant or antiplatelet drug | Risk of bleeding increases | Advise client not to take without provider approval |
| NSAIDs | |||
| Anticlotting drugs such as streptokinase and urokinase | May decrease effect | Advise against use | |
| Antihypertensives | May increase antihypertensive effect | Monitor BP | |
| Antihyperglycemic drugs | Serum glucose control may improve, lowering the amount of medication needed | Monitor blood glucose levels | |
| Ginkgo | Aspirin Heparin and warfarin | Risk of bleeding increases | Teach client not to take without approval of provider |
| Antihyperglycemic drugs | May alter blood glucose levels | Monitor blood glucose closely | |
| Antihypertensives Nifedipine | May cause increased effect | Monitor blood pressure | |
| Ginseng | Antihyperglycemic drugs | May intensify effect | Monitor for hypoglycemia |
| Anticoagulants and antiplatelet drugs | May increase bleeding | Advise use with caution | |
| Corticosteroids | May interfere with action | Advise against use | |
| Digoxin | May increase blood level | Advise against use | |
| Green tea | Warfarin | May alter anticoagulant effects | Advise against use |
| Hawthorn | Digoxin | May cause a loss of potassium, leading to drug toxicity | Monitor blood levels |
| Beta blockers and other drugs lowering blood pressure and improving blood flow | May be additive in effects | Monitor blood pressure meticulously; advise that this concern extends to erectile dysfunction drugs also | |
| St. John’s wort | HMG-CoA reductase inhibitors (e.g., Lipitor, simvistatin) | May decrease plasma concentrations of these drugs | Monitor levels of lipids |
| Digoxin | Decreases the effects of the drug | Advise against use | |
| Alprazolam (Xanax) | May decrease effect of drug | Advise against use | |
| Efavirenz and other anti-HIVs | May decrease drug level | Advise against use | |
| Photosensitizing drugs (e.g., NSAIDs, some antibiotics) | Increased photosensitivity | Advise sun block use | |
| Tramadol | May increase risk of serotonin syndrome | Advise against use | |
| Olanzapine (Zyprexa) | May cause serotonin syndrome | Advise against use | |
| SSRIs (e.g., Xoloft) | Excessive sedation | Advise against use | |
| Albuterol | Decreases effect | Monitor drug effects | |
| Warfarin (Coumadin) | May decrease anticoagulant effect | Advise against use | |
| Amlodipine | Lowers efficacy of calcium channel | Advise against use |
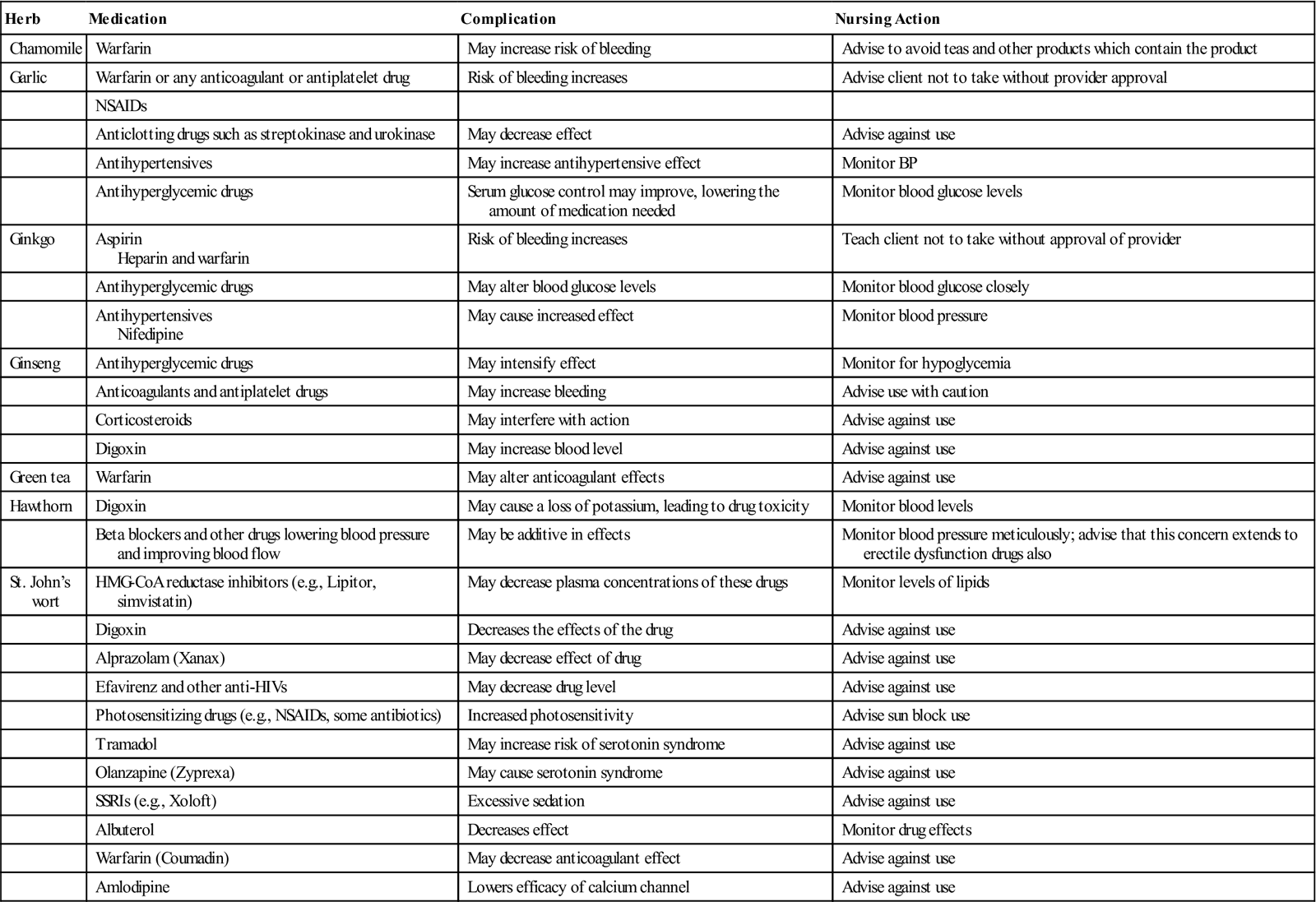
From Basch E, Ulbricht C: Natural standard herb & supplement handbook: the clinical bottom line, St. Louis, 2005, Mosby; Jellin JM, editor: Natural medicines comprehensive database (2006). Available at www.naturaldatabase.com/; NDH pocket guide to drug interactions, Philadelphia, 2002, Lippincott, Williams & Wilkins; Yoon SL, Schaffer SD: Herbal, prescribed, and over-the-counter drug use in older women: prevalence of drug interactions, Geriatr Nurs 27(2):118-129, 2006; Merck Sharp & Dohme Corp: Some possible dietary supplement-drug interactions. In The Merck manual for health care professionals (2011). Available at http://www.merckmanuals.com/media/professional/pdf/Table_331-1.pdf.
Chronopharmacology
Another factor that affects both pharmacokinetics and pharmacodynamics are the normal biorhythms of the body. The relationship of biological rhythms to variations in the body’s response to drugs is known as chronopharmacology. Although it has not yet been explored in aging, chronopharmacology is a developing science that may lead to more effective drug therapy (Ohdo, 2010). The best time to administer medications is now being considered in light of the biorhythms of various physiological processes. For example, if a cortisone tablet (e.g., from a Medrol dose pak) is taken in the morning it suppresses the adrenocortical system very little. If the same dose were given divided over the day, unwanted effects of the drug will occur from suppression of the hypothalamus-pituitary-adrenal axis.
As noted earlier, absorption depends on gastric acid pH, the level of motility of the gastrointestinal tract, and blood flow. All have been shown to have biorhythmical variations. Distribution of protein-bound drugs depends on albumin and glycoproteins produced by the liver. During the day, albumin levels are high, but they are low in the early morning. Drug metabolism is also biorhythmical due to changes in the liver over the course of the day. Renal elimination depends on kidney perfusion, glomerular filtration, and urine acidity and has shown rhythmic variation. The brain, the heart, and blood cells have also been found to have varied rhythmicity, resulting in a cyclical response for beta blockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, nitrates, and other, similar drugs. Table 8-4 shows some of the rhythmical influences on diseases and physiological processes.
TABLE 8-4
Rhythmical Influences on Disease and Physiological Processes
| Disease or Process | Rhythmical Influence |
| Allergic rhinitis | Symptoms worse in the morning |
| Arterial blood pressure | Circadian surge—morning hours |
| Asthma | Greatest respiratory distress overnight (during sleeping) |
| Symptoms peak in early morning (4 to 5 AM) | |
| Blood plasma | Plasma volume falls at night, thus hematocrit increases |
| Cancer | Tumor cells proliferate when normal cell miosis is low |
| Cardiac disease | Angina, myocardial infarction, thrombolytic stroke occur in the first 4 hours after waking (peak 9 AM) (through 10 PM) |
| (Prinzmetal’s angina—during sleep) | |
| Catecholamines | Increase in early morning |
| Fibrinolytic activity | Increase in early morning |
| Platelet activation | May result from abnormality in circadian rhythm, which affects cortisol levels, body temperature, sleep-wake cycle |
| Gastric system | Gastric acid secretion peaks every morning (2 to 4 AM); circannual variability—incidence of gastric ulcers greater in winter |
| Osteoarthritis | Pain more severe in morning |
| Potassium excretion | Lowest in morning; highest in late afternoon |
| Rheumatoid arthritis | Pain more severe in late afternoon |
| Systemic insulin | Highest in afternoon |
As more is learned about chronotherapeutics, the potential for decreasing individual doses of medications and/or the frequency of administration is present. As we are able to do so we will be able to significantly decrease the potential for adverse drug events while maximizing therapeutic effects.
Medication-related problems and older adults
Polypharmacy
Although there is controversy about how many drugs are “too many,” polypharmacy is the term used to indicate multiple drug use, and usually this implies the use of some drugs that are duplicated or unnecessary (Figure 8-2). Junius-Walker and colleagues (2007) define polypharmacy as taking more than five medications at the same time. In their study of German elders, the average number of prescribed medications was 3.7 and the average number of over-the-counter (OTC) bioactive products was 1.4. They also found that almost 27% of those surveyed took over five medications; and, as the number increased, so did the likelihood of inclusion of inappropriate medications (ineffective, duplicative, or not indicated). Polypharmacy may occur “accidentally” if an existing drug regimen is not considered when new medications are prescribed or any number of the thousands of OTC preparations and supplements are added to the prescribed medications. The two major concerns with polypharmacy are the increased risk for drug interactions and the increased risk for adverse events. Adverse events include adverse drug interactions and reactions, adverse drug withdrawal, and therapeutic failures.
Drug interactions
The more medications a person takes, the greater the possibility that one or more of them will interact with each other, with an herbal product, with a nutritional supplement, with food, or with alcohol. When two or more medications or foods are taken together or close together, the drugs may potentiate one another, or make one or both either more or less effective.
An interaction may result in altered pharmacokinetic activity, that is, alterations in the absorption, distribution, metabolism, or excretion of one or any of the medications. Absorption can be delayed by drugs exerting an anticholinergic effect. Tricyclic antidepressants act in this manner to decrease gastrointestinal motility and interfere with the absorption of other drugs. More than one drug may compete to simultaneously occupy the necessary binding receptors, preventing one or the other from reliably reaching the target organs and creating a varied bioavailability of one or both.
Interference with enzyme activity may alter metabolism and cause drug deficiencies or toxic and adverse responses from altered renal tubular function. Outside the body, interactions can occur any time that two medications or foods are mixed together before administration. For example, when delivering medications through a feeding tube, giving each one separately takes more time than is usually feasible. In haste the nurse may crush and deliver all of them simultaneously. The appropriate administration requires that the nurse know not only which medications are “crushable” but also which can be administered together. For example, Fosamax and the other bisphosphonates must be taken with a full glass of water 1 hour before any other medication, beverage, or food is ingested.
In pharmacodynamic interactions, one drug alters the patient’s response to another drug without changing the pharmacokinetic properties. This can be especially dangerous for older adults when two or more drugs with the same effect are additive, that is, together they are more potent than each one taken separately. Unless attention is paid to what the overall drug list includes, when each drug is administered, and what other products are taken, a harmful situation of polypharmacy will occur. The nurse decreases the likelihood of this happening by monitoring the medications he or she administers and by encouraging the persons under their care to do the same. Although there is much that is unknown about the use of herbs and other bioactive substances, as studies are completed, the nurse will need to learn more and more about potential adverse reactions and interactions in order to safely manage medications.
Adverse drug reactions
An adverse drug reaction (ADR) or adverse drug event (ADE) is an unwanted pharmacological effect, ranging from a minor annoyance to death and including allergic reactions. These may be iatrogenic, drug-drug, drug-supplement, or drug-disease. It has been estimated that a person taking two different drugs has a 13% chance of having an ADR at some point, compared to 82% of those taking seven or more drugs (Constantiner, 2011). ADRs can sometimes be predicted from the pharmacological action of the drug (e.g., bone marrow depression from cancer chemotherapy; bleeding from Coumadin). Predictable ADRs can also occur when a patient is started on a drug at a dosage that is inappropriately high or one that necessitates laboratory monitoring and adjustment that is not done (e.g., lithium, Coumadin).
ADRs occur in all situations in which one takes or is administered medications. Older adults are four time more likely to be hospitalized for an ADR than younger persons (Ruscin, 2009). Page and Ruscin (2006) found that 31.9% of the elders studied experienced at least one ADR while hospitalized. In a review of several studies of ADRs in nursing homes, Handler and colleagues (2006) found the rate to range from 1.19 to 7.26 per 100 resident months. Atypical antipsychotics, warfarin, antidepressants, and sedative-hypnotics are most commonly associated with preventable ADRs in the nursing home setting, with hypoglycemic agents, nonsteroidal antiinflammatory agents (NSAIDs), and benzodiazepines in the community (Ruscin, 2009). All of these are frequently prescribed to older adults. Because of the large number of medications taken by most older adults in long-term care settings and their frequently altered nutritional and fluid status, the risk for adverse reactions is of special concern to nurses working in this setting. It is estimated that 27% of the ADRs in the community and 42% of those in the nursing home are preventable (AGS, 2012).
ADRs are not always predictable. An older patient who is well controlled on a stable dose of a drug may undergo a change in his or her physiology or environment and the body’s response to the drug may be altered (e.g., levothyroxine [Synthroid]). Changes in diet can also have a profound impact on drug effect. For example, decreased fluid intake can cause lithium toxicity and increased intake of leafy green vegetables will counteract the anticoagulant effects of Coumadin and aspirin (Miller, 2008). Some drugs interfere with the body’s ability to regulate temperature (e.g., antipsychotics, stimulants, anticholinergics) such that hot weather can lead more easily to heat stroke (Ruscin, 2009). Other drugs are photosensitizing, and an increase in sun exposure can lead more quickly to sunburn than expected (e.g., sulfa drugs, antidepressants, and many antipsycotics) (Semla et al., 2008). Older adults who have decreased fluid intake because of illness or because they cannot get to fluids, or who have inadequate intake during hot weather, may quickly become volume depleted and develop increased sensitivity to the orthostatic hypotensive effects of alpha blockers (e.g., phenothiazines, terazosin) or toxicity to antipsychotics (Jett, 2012).
One of the most troublesome ADRs for the older adult is drug-induced delirium and confusion. Polypharmacy with several psychoactive drugs exerting anticholinergic actions is perhaps the greatest precipitator of delirium as an adverse reaction. Too often delirium goes unrecognized as an ADR and instead is viewed as a worsening of preexisting dementia or even new-onset dementia (see Chapter 21). Any time there is a change in the person’s cognitive abilities or mental status, the possibility of drug effect must be thoroughly evaluated. See Box 8-2 for a partial list of drugs with the potential to adversely affect cognitive functioning.