- Structure and function of cholesterol and triglyceride (TG)
- Blood transport of lipids (including cholesterol and TG)
- Distinction between total cholesterol, LDL-cholesterol and HDL-cholesterol
- Factors to be considered before sampling blood for lipids
- Significance of serum lipids for atherosclerosis
- Serum cholesterol and risk of cardiovascular disease
- Defining those who require cholesterol testing
- Target (healthy) serum cholesterol concentration
The principle use of this blood test is to help assess an individual’s overall risk of the cardiovascular diseases that result from atherosclerosis. The most significant of these is coronary heart disease (CHD), which affects an estimated 2.7 million in the UK and currently accounts for close to 88 000 deaths in the UK each year1. Despite 50% reduction in annual CHD deaths over the past 20 years, it remains second only to cancer (all types) as the leading cause of death in the UK1. There is overwhelming evidence that too much cholesterol and/or triglyceride in the blood increases the risk of CHD and all other atherosclerosis related cardiovascular diseases. The higher the level the greater is this risk. The test is used not only to assess risk but also to monitor the effectiveness of therapy (drugs, most commonly statins, and dietary manipulation) aimed at reducing the amount of cholesterol and triglyceride in blood.
Normal physiology
What are cholesterol and triglycerides?
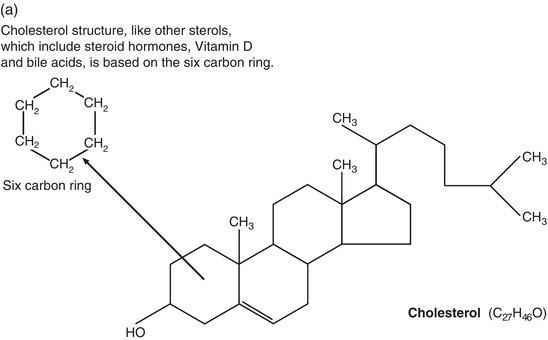
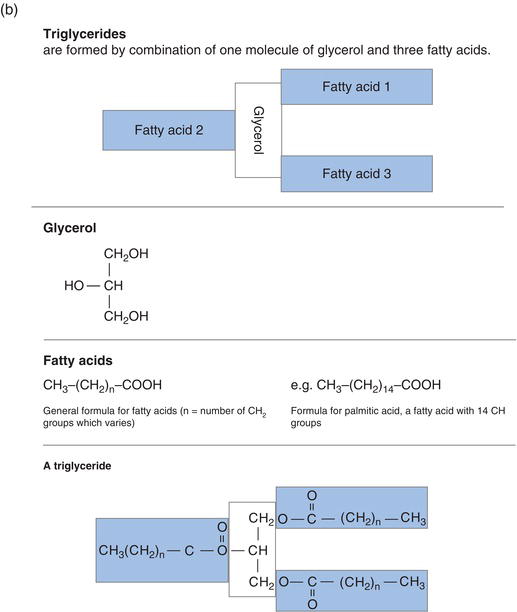
Apart from inorganic elements such as sodium, potassium, calcium etc., there are four broad classes of chemical present in the human body and the food we eat. They are: proteins, carbohydrates, nucleic acids and lipids (or fats). Although structurally dissimilar (Figure 8.1), cholesterol and triglycerides are lipids.
They are provided in a normal diet, both being present in meat and dairy products. Eggs are a particularly rich source of cholesterol. In addition to dietary sources, cholesterol and triglyceride are synthesised in the body, principally the liver (both cholesterol and triglyceride) and adipose or fat tissue (triglycerides only).
Function of cholesterol and triglycerides
In common with all lipids, cholesterol and triglycerides are essential components of cell membranes. Their function is however not confined to cell structure. In the liver, cholesterol is converted to bile acids and bile salts, which are excreted from the liver, via the gall bladder, to the intestinal tract in the digestive juice, bile. The presence of bile acids and salts in bile is essential for absorption of dietary fats. Cholesterol is the raw material from which steroid hormones are synthesised; examples include cortisol in the adrenal glands, progesterone in the ovaries and testosterone in the testis. Vitamin D is synthesised in the skin from a cholesterol derived compound.
Triglyceride is the principal fat present in adipose (fat) tissue and as such its main function is energy storage; triglycerides provide an alternative energy source to glucose, during fasting and starvation when glucose is in short supply. During these periods of relative glucose depletion, triglyceride present in adipose cells is broken down to its constituent parts by an enzyme called lipase; the process is called lipolysis. The free fatty acids that result from lipolysis are transported in blood to cells around the body, where they are oxidised (burnt) providing chemical energy. Meanwhile the other product of lipolysis, glycerol, is converted to glucose in the liver.
Blood transport of cholesterol and triglyceride
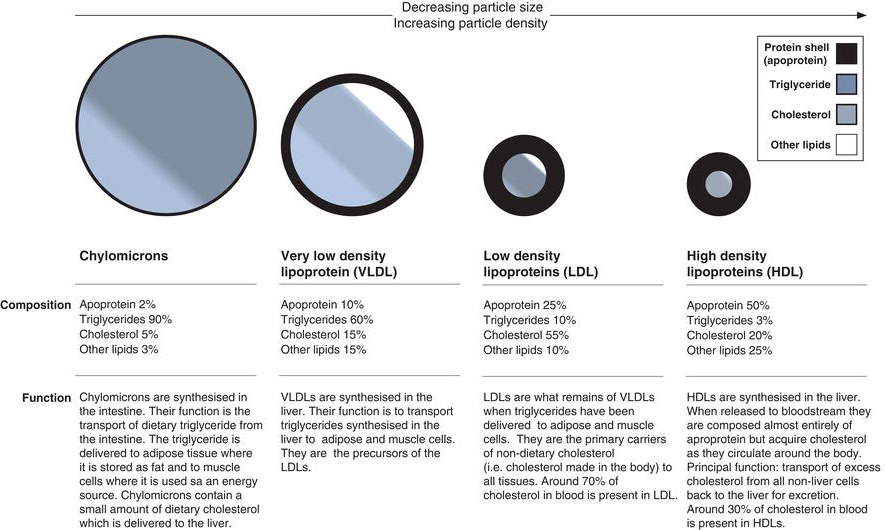
Like all lipids, cholesterol and triglyceride are insoluble in water. This poses a difficulty for their transport in blood plasma, which is a water-based (aqueous) solution of chemicals. To overcome this difficulty lipids, including cholesterol and triglycerides, are packaged in a water-soluble protein shell called an apoprotein. The total package, lipids plus apoprotein is called a lipoprotein. There are four main types of lipoprotein in blood, each with differing proportions of cholesterol, triglyceride and apoprotein (Figure 8.2). They are defined by their relative density and particle size and are known as:
- Chylomicrons (lowest density, largest particle).
- Very low density lipoproteins (VLDLs).
- Low density lipoproteins (LDLs).
- High density lipoproteins (HDLs).
Around 70% of the cholesterol in blood is present in LDL and most of the remainder is present in HDL. By contrast most of the triglyceride in blood is contained within VLDL. As will become clear, the distinction between LDL-cholesterol and HDL-cholesterol is clinically important.
Laboratory measurement of plasma/serum cholesterol and triglyceride
Patient preparation
The concentration of cholesterol and triglyceride in blood is affected by diet, smoking, alcohol intake, inter-current illness and even changes in posture. It is important that where possible blood is sampled under standard conditions to minimise some of these effects.
- The patients normal diet should be followed in the two to three weeks prior to testing.
- There is a transient and quantitatively unpredictable rise in blood triglyceride level immediately after a meal, making interpretation difficult. For this reason blood for triglyceride estimation must be sampled only after an overnight fast of 12–14 hours. Fasting is not necessary if total cholesterol only is of interest but is necessary if LDL-cholesterol is requested because serum triglyceride is required for calculation of serum LDL-cholesterol concentration (explained further).
- The test should be deferred for three months if the patient has suffered major illness (e.g. myocardial infarction) or major surgery unless blood can be sampled within 12 hours of such an event. The test should be deferred for two to three weeks after minor illness.
- The patient should be well rested and seated for five to ten minutes before blood collection.
- Use of a tourniquet for more than a minute or so before blood collection can cause erroneous results. If possible avoid the use of tourniquet for this test.
- Interpretation of results is not possible if blood is sampled during lipid infusion (e.g. intraplipid).
Sample requirement
Around 5 ml of venous blood is required. The test may be performed on either plasma or serum. If local policy is to use serum then blood must be collected into a plain chemistry tube (i.e. without anticoagulant). If local policy is to use plasma then blood must be collected into a tube containing an anticoagulant (EDTA or heparin) which prevents blood from clotting.
In the laboratory
Three measurements are made in the laboratory:
- Serum or plasma concentration of total cholesterol (i.e. cholesterol contained in LDL, HDL and VLDL).
- Serum or plasma concentration of HDL-cholesterol (i.e. only the cholesterol contained in HDL).
- Serum or plasma concentration of triglycerides (i.e. triglyceride contained in VLDL, LDL and HDL).
The concentration of serum or plasma LDL-cholesterol is technically difficult to measure and in most laboratories is calculated using the results of analysis in the following well validated equation:
LDL-cholesterol = Total cholesterol − HDL-cholesterol − (Triglyceride/2.2)
Interpretation
Reference range – fasting triglycerides
0.45–1.80 mmol/L
Total cholesterol, HDL cholesterol and LDL cholesterol
Unlike most other blood tests the concept of a normal or reference range is not appropriate for cholesterol testing. This is because a large proportion of apparently healthy individuals from which a reference range would normally be constructed have cholesterol levels (total cholesterol, LDL-cholesterol and HDL-cholesterol) that are associated with increased risk of cardiovascular disease. In other words it is ‘normal’ to have an unhealthy amount of cholesterol in blood. Rather than a reference range, the concept of target values is used to interpret cholesterol results. Target values will be discussed a little later but for now it would be helpful to record some data about serum cholesterol concentration in the UK population.
- The mean plasma/serum total cholesterol for adults (>16 years) is 5.2 mmol/L for men and 5.4 mmol/L for women. The equivalent figures for those aged 45–65 years who have highest levels are: 5.8 mmol/L for men and 6.0 mmol/L for women2.
- The National Service Framework target for cardiovascular disease prevention is plasma/serum total cholesterol <5.0 mmol/L3.
- Around 60% of adults have total cholesterol >5.0 mmol/L2.
Terms used in interpretation
Hyperlipidaemia | raised concentration of lipids in blood, i.e. total cholesterol >5.0 mmol/L and/or triglyceride >1.8 mmol/L. |
Hypercholesterolaemia | raised concentration of total cholesterol, i.e. >5.0 mmol/L. |
Hypertriglyceridaemia | raised blood concentration of triglyceride, i.e. >1.80 mmol/L. |
Consequences of raised cholesterol or triglyceride cardiovascular disease
As concentration of plasma/serum total cholesterol rises so too does the risk of those cardiovascular diseases that result from the restricted blood flow through arteries diseased by atherosclerosis, and associated thrombotic (blood clotting) consequences. Atherosclerosis may affect any artery, but the most commonly affected are the coronary arteries. The result is coronary heart disease, the most common cardiovascular disease.
Coronary heart disease
Coronary heart disease (CHD) (alternative name ischaemic heart disease) is caused by atherosclerosis in the coronary arteries that supply oxygenated blood to heart muscle (the myocardium). The focal thickening and hardening of the normally elastic walls of coronary arteries that characterises atherosclerosis progressively reduces the internal diameter of the artery, restricting blood flow and therefore oxygen delivery to the cells of which the myocardium is composed. The portion of myocardium affected becomes relatively deficient of oxygen (ischaemic). The first clinical manifestation of this relative oxygen deficit is usually angina pectoris or stable angina, intermittent attacks of chest pain or discomfort precipitated by increased heart rate due to exercise or some other stress. The pain subsides as rest and return of resting heart rate reduces the increased oxygen demand of myocardium.
Atherosclerosis predisposes to the inappropriate activation of the clotting cascade and formation of a blood clot (thrombus) within blood vessels at the site of atherosclerosis. This further occludes or totally occludes blood flow through the artery, effectively starving myocardial cells of the nutrients and oxygen required for survival. The clinical consequence of this is either unstable angina that is chest pain at rest or myocardial infarction (heart attack). The two conditions are referred to as acute coronary syndromes. A diagnosis of unstable angina implies high risk of future myocardial infarction. Myocardial infarction implies tissue necrosis (cell death), that is permanent damage to heart muscle as a result of ischaemia. The damage to the heart may result in sudden death if it causes lethal abnormal rhythms (e.g. ventricular fibrillation).
Stable angina, unstable angina, myocardial infarction and sudden death represent the most common manifestations of CHD in order of severity. They do not necessarily present in this ordered sequence and myocardial infarction or sudden death may be the first indication of coronary disease.
Other cardiovascular disease
Other sites less commonly affected by atherosclerosis include:
- Peripheral arteries that supply oxygenated blood to the limbs.
- Cerebral arteries which supply oxygenated blood to the brain.
- Abdominal aorta, lower half of the main blood vessel (aorta) that delivers oxygenated blood to the body.
Peripheral arterial disease usually affects the legs. Reduced oxygen delivery (consequent on reduced blood flow) to leg causes calf muscle pain on exercise, which is relieved by rest (intermittent claudication). The most severe presentation occurs if a thrombus forms at the site of atherosclerosis, totally occluding blood flow through the affected artery. Without urgent treatment to restore blood flow, resulting acute ischaemia can lead to necrosis, gangrene and necessity for amputation.
Reduced blood flow through cerebral arteries partially occluded by atherosclerosis is a common cause of transient ischaemic attacks (mini-strokes). Occlusion of cerebral arteries by a thrombus formed at the site of atherosclerosis is the most common cause of cerebrovascular accident (stroke), which can result in permanent disability or death.
Atherosclerosis in the abdominal aorta contributes to the weakening of the wall of this large vessel that results in dangerous dilation (aneurysm). This can be asymptomatic or cause abdominal pain. Without surgical repair to the vessel, progressive dilation can lead to catastrophic rupture of the aneurysm, massive haemorrhage and sudden death.
Blood lipids and cardiovascular disease
Atherosclerosis, the underlying pathology of CHD and other cardiovascular disease outlined already, is a complex and as yet not fully understood phenomenon which begins many years before symptoms develop. It is clear however that there are well defined risk factors (Table 8.1) which predispose people to atherosclerosis and subsequent cardiovascular disease. Some, like cholesterol and triglyceride, are modifiable, and some are not.
All risk factors must be taken into account to make the most reliable assessment of an individual’s overall risk of CHD.
To understand how the lipids in blood, particularly cholesterol, contribute to CHD and other cardiovascular disease it is necessary to examine in a little more detail what is known about the process of atheroma formation, which leads to atherosclerosis and thrombosis.
Atheroma formation begins with damage to the endothelium that lines the internal surface of arteries, allowing entry of cholesterol-rich LDL particles present in blood. The damage attracts protective cells called macrophages which take up the LDL particles; LDL accumulates in these cells. At this early stage the only evidence of atheroma is a barely visible raised yellowish patch on the internal surface of the artery, known as a fatty streak. Development of the fatty streak to the more ominous and complex fatty plaque that protrudes into the lumen of the artery is thought to involve an inflammatory reaction initiated by the death of the cells engorged with LDL-cholesterol. The normal smooth muscle cells of which arterial walls are composed migrate into the plaque, proliferate and synthesise fibrous proteins like collagen, which renders the growing plaque hard. The atherosclerotic plaque has a lipid rich centre surrounded by a dynamic fibrous cap composed of collagen protein and pro-inflammatory cells. The strength and stability of the cap is of great pathological significance because this determines if thrombosis occurs. A thin and fragile cap may rupture exposing the platelets in blood flowing through the vessel to substances beneath the cap that promote platelet aggregation and activation at the site of the ruptured plaque. This in turn initiates the clotting cascade with formation of a blood clot (thrombus), which may completely occlude blood flow.
Table 8.1 Major risk factors for coronary heart disease (CHD).
| Increasing age Family history of CHD Diabetes Diabetics have 2–4 times the risk of CHD compared with non-diabetics who in all other respects have a similar risk status Cigarette smoking* Hypertension* Unhealthy bodyweight* Defined as body mass index (BMI) >25 [BMI = weight in kg divided by height in m2 ]. Obesity (BMI >30) is associated with hypertension, increased total and LDL-cholesterol and reduced HDL-cholesterol Unhealthy diet* High fat diet (i.e. fat more than 30% of total calorific intake) High intake of saturated rather than unsaturated fat High intake of trans fats (non-natural fats produced by industrial process) High cholesterol intake Diet devoid of fruit and vegetables, which provide ‘protective’ antioxidant vitamins High salt diet (causes hypertension) Excess alcohol* Although alcohol in moderation (glass of red wine or pint of beer per day) is thought to protect against heart disease, as intake rises above 21 units of alcohol per week so too does risk of CHD; excess alcohol can cause hypertension Lack of exercise* Exercise reduces body weight and increases the amount of ‘protective’ HDL-cholesterol present in blood Unhealthy amount of lipids in blood* Increased plasma/serum total cholesterol concentration Increased plasma/serum LDL-cholesterol concentration Reduced plasma/serum HDL-cholesterol concentration High ratio of plasma/serum total cholesterol : plasma/serum HDL-cholesterol |
* Modifiable risk factors.
In general, stable angina is associated with a stable plaque, whereas acute coronary syndromes (unstable angina and myocardial infarction) are associated with an unstable plaque, plaque rupture and consequent thrombosis.
The growth of atherosclerotic plaques to the point where they can occlude blood flow sufficiently to cause symptoms of cardiovascular disease is very slow, occurring over a period of many years. There is now evidence that by addressing risk factors such as hyperlipidameia it is possible to halt or even reverse plaque progression4.
Research directed at better understanding of the complexities of atherosclerosis continues, but some aspects are clear:
- Accumulation of cholesterol, specifically LDL-cholesterol is an important requirement for atheroma formation.
- The LDL-cholesterol found in atherosclerotic plaques is derived from the blood.
- The higher the concentration of cholesterol in blood the greater is the risk of CHD and other cardiovascular disease.
- It is specifically LDL-cholesterol that is damaging; the higher the LDL the greater is the risk of CHD.
- By contrast, HDL is protective against CHD because it clears the blood of cholesterol. The lower the HDL-cholesterol the greater is the risk of CHD. A high level of HDL-cholesterol is associated with reduced risk of CHD.
- Reducing the concentration of total cholesterol in a patient with raised levels is effective in reducing overall risk of CHD.
- The link between blood triglyceride and CHD is currently less clear. There is evidence that particularly among those who have an increased LDL-cholesterol or a reduced HDL-cholesterol, a raised blood triglyceride increases yet further the risk of CHD.
- There is little evidence however to suggest that reducing raised triglyceride levels decreases the risk of CHD.
It must be emphasised that blood lipid testing determines risk only; results cannot be used to diagnose or definitively predict CHD for a particular individual. Some have a raised LDL-cholesterol and do not suffer CHD and there is no safe level of cholesterol or triglyceride below which one can be guaranteed not to suffer CHD. The best we can say is that the higher the level of LDL-cholesterol, the greater is the risk of CHD; that risk is increased if triglycerides are also raised, and reduced by a high HDL-cholesterol level. The World Health Organisation (WHO) estimates that if everyone had a serum total cholesterol <3.8 mmol/L then the total number of patients suffering CHD would be reduced by 60%5. This gives some notion of the considerable contribution that raised cholesterol makes to overall risk of CHD.
Other effects of raised blood lipids
There are few signs or symptoms to suggest that an individual may have an increased level of cholesterol or triglyceride and the onset of anginal pain or myocardial infarction may be the first indication. Lipid deposits (xanthomata) visible as nodules may form in subcutaneous tissue (most commonly the Achilles tendon) among those with very high levels. Lipid may also accumulate in the cornea. Severe hypertriglyceridaemia is associated with abdominal pain and is a rare cause of acute pancreatitis.
Causes of raised cholesterol and/or triglycerides
Many genetic defects in lipid metabolism have been identified which result in a raised cholesterol, a raised triglyceride or both, so that it is possible to inherit a predisposition to raised blood lipids. This in part explains the observation that CHD runs in families. One of these inherited conditions is extremely common, several are less common and most are extremely rare. All are grouped together in the term primary hyperlipidaemias. A raised cholesterol or triglyceride may arise as a complication of another disease process; this is called secondary hyperlipidaemia. Treatment of the underlying disease often corrects secondary hyperlipidaemia.
Primary hyperlipidaemia
The most common cause of primary hyperlipidaemia is known as ‘polygenic’ hypercholesterolaemia. As its name implies many genes interact to cause raised cholesterol. The condition results in mild to moderate increase in LDL-cholesterol, the actual level depending to a great extent on diet. Triglyceride levels are usually normal. Much higher levels of LDL-cholesterol, often greater than 9.0 mmol/L, characterise a less common inherited condition known as familial hypercholesterolaemia which affects around 1 in 500 in the UK. This single gene defect is associated with high risk of myocardial infarction in early middle age.
Although rare it is possible to inherit a predisposition to raised triglyceride levels. Familial hypertrigylceridaemia is the most common genetic cause of raised triglyceride. Levels are usually very high (>10 mmol/L). Cholesterol levels are usually normal. Risk of CHD is not greatly increased for this group of patients.
Secondary hyperlipidaemias
The most common cause of secondary hyperlipidaemia is diabetes mellitus. Untreated diabetic patients tend to have a mild increase in LDL-cholesterol and moderate to severe increase in triglyceride. This is at least in part the reason why diabetic patients are at high risk of CHD. Other causes of secondary hyperlipidaemia include hypothyroidism, nephrotic syndrome, cholestatic liver disease and alcohol abuse.
National guidelines (recommendations) for prevention of cardiovascular disease6,7
The Joint British Societies guidelines6 recently endorsed by NICE7 identify the following groups of people who require careful monitoring of blood cholesterol and cholesterol lowering drug intervention to reduce blood cholesterol because they are all at equally high risk of future cardiovascular disease:
- Those with a history of atherosclerotic cardiovascular disease (e.g. angina, myocardial infarction, stroke etc.).
- Those with diabetes (Types 1 and 2).
- Those with elevated blood pressure (>160 mmHg systolic or >100 mmHg diastolic).
- Those with hypercholesterolaemia (defined as total cholesterol to HDL cholesterol ratio >6).
- Those without any cardiovascular disease but whose quantified risk of developing it during the next ten years is greater than 20%.
[Note: It is recommended that all adults over the age of 40 who have no history of cardiovascular disease be assessed in primary care every five years using the latest Joint British Societies risk charts to quantify their ten year risk of cardiovascular disease. This risk assessment is based on consideration of the following five major risk factors: age, sex, smoking habit, systolic blood pressure and ratio of total to HDL-cholesterol.]
The optimal total cholesterol target for all those in these high risk groups is <4 mmol/L, and that for LDL-cholesterol <2.0 mmol/L. The previous recommended targets contained in the National Service Framework for CHD prevention (total cholesterol <5.0 mmol/L and LDL-cholesterol <3.0 mmol/L) have thus been revised downwards in the light of accumulating evidence that reducing total and LDL-cholesterol yet further has benefit in terms of reducing both morbidity and mortality due to cardiovascular disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree