Management of Pain During Labor
Objectives
2. Describe the factors that influence a woman’s comfort during labor.
3. Explain the physical causes of pain during labor.
4. Explain the role of endorphins in the body.
5. Discuss three nonpharmacologic pain control strategies.
6. Review the potential effect of sedatives and narcotics on the newborn.
7. Explain the advantages and limitations of pharmacologic methods of pain management.
Key Terms
anesthesia (ăn-ĕs-THĒ-zē-ă, p. 153)
blood patch (p. 155)
cognitive stimulation (KŎG-nĭ-tĭv stĭm-ū-LĀ-shŭn, p. 150)
cutaneous stimulation (kū-TĀ-nē-ŭs, p. 150)
effleurage (p. 148)
endorphins (p. 148)
epidural block (ĕp-ĭ-DOO-răl, p. 153)
gate control theory (p. 148)
pudendal block (pū-DĔN-dăl, p. 153)
sacral pressure (SĂ-krăl, p. 150)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
Pain Management
Labor pains exist for a short time only. However, within that short time, the discomfort progresses from a slightly unpleasant experience to intense sensations. To the woman in labor, discomfort or pain may seem endless, and she may wonder whether she can tolerate it. To the nurse, the process of labor is a challenge. Armed with knowledge of the characteristics of pain in the various stages of labor, interventions for pain relief, comfort methods, and cultural responses to labor pain, the nurse is able to design a care plan to meet the specific needs of the woman in labor. Working with the woman, family, and other health professionals, the nurse can meet the challenges of making each labor and birth a safe and satisfying experience.
Standards of Pain Management
The Joint Commission (TJC) recognizes the importance of pain control in all health care settings for all patients. Standards include:
The Unique Pain of Labor
Pain is universal. How it is experienced is both personal and subjective. Childbirth pain differs from pain experienced in other conditions in the following ways:
• The sources of pain are known. The purpose of the muscle contraction helps in the birthing process.
Pain control during labor can be managed by nonpharmacologic (non-drug) or pharmacologic (drug) methods. General nonpharmacologic comfort measures during labor, such as adjustment of the environment, breathing techniques, or maternal positioning, are discussed in Chapter 5.
Factors that Influence Labor Pain
Several factors cause pain during labor and influence the amount of pain a woman experiences. Other factors influence a woman’s response to and ability to tolerate or cope with labor pain.
Pain Threshold and Pain Tolerance
Two terms are often used interchangeably to describe pain, although they have different meanings. Pain threshold, also called pain perception, is the least amount of sensation that a person perceives as painful. Pain threshold is fairly constant, and it varies little under different conditions. Pain tolerance is the amount of pain one is willing to endure. Unlike the pain threshold, one’s pain tolerance can change under different conditions. A primary nursing responsibility is to modify as many factors as possible so that the woman can safely tolerate the pain of labor and delivery.
Sources of Pain During Labor
Physical sources are the main contributors to pain during labor:
• Dilation and stretching of the cervix (stimulates nerve ganglia)
• Pressure and pulling of pelvic structures (ligaments, fallopian tubes, and peritoneum)
• Distention and stretching of the vagina and perineum (splitting and tearing sensation)
• The intensity of labor contractions
• The length of time for cervical changes to occur
• The size and position of the fetus, which add to the length of labor
Other factors that contribute to the pain of labor include:
Gate Control Theory
The gate control theory of pain has application to labor and childbirth. According to the gate control theory, a gating mechanism occurs in the spinal cord. Pain sensations are transmitted from the periphery of the body along nerve pathways to the brain. Only a limited number of sensations can travel these pathways at one time. Distractions or focused activity can replace travel of pain sensation. When the activity fills the path, the gate is closed, and impulses are less likely to be transmitted to the brain. When the gate is open, pain impulses ascend to the brain. Similar gating mechanisms exist in the descending nerve fibers from the hypothalamus and cerebral cortex. These areas of the brain regulate a person’s thoughts and emotions and can influence whether pain impulses reach the level of conscious awareness. Effleurage, cutaneous stimulation by a patterned massage of the abdomen, may have a direct effect on closing the gate. The gate control theory, by using descending and ascending neural pathways, helps explain the effectiveness of various types of focusing strategies taught in childbirth preparation classes, such as breathing, listening to music, verbal coaching, and effleurage. Acupuncture, external analgesics, and back massage provide relief because they help close the “gate” to the discomfort.
Chemical Factors
Neuromodulators, also called endorphins or endogenous opiates, are protein chemicals found in the brain. They are produced by the anterior pituitary gland and the hypothalamus. They are natural opiate-like substances known to relieve pain. Endorphins (and enkephalins) are similar to morphine-like substances. They are believed to play a major role in the biologic response to pain. They may be produced by stress and increase the pain threshold, thus helping the woman tolerate the pain of labor and birth. Endorphins are believed to make the woman drowsy and sleepy. Studies have shown that the endorphin blood level in a woman during the birthing process is much higher than that of a nonpregnant woman. Women who have a positive attitude during labor and birth have more natural protection because of their body’s ability to produce its own endorphin analgesia.
Nonpharmacologic Pain Control Strategies
The United States is a multicultural society, and the nurse must understand the cultural traditions concerning expression of pain to provide culturally sensitive care and support. Fear, anxiety, and muscle tension increase catecholamine secretion and increase pain perception. All laboring women benefit from nursing interventions that can relieve fear, tension, and anxiety. The nurse must empower the mother to use her own method of dealing with pain.
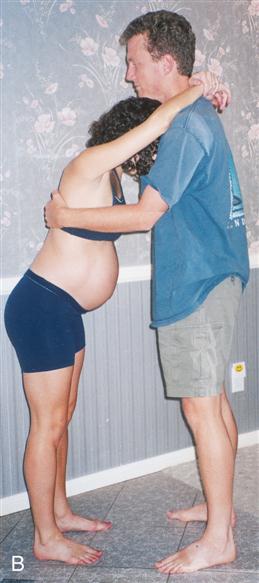
Various nonpharmacologic measures for control of labor pain are practiced (Box 8-1). Many of these techniques are learned in childbirth education classes. These include general support, imagery or visualization, distraction, changes in temperature, touch, comfort measures, and baths (whirlpool if available). The nurse’s role is to assist the woman in using the techniques she has learned during childbirth classes and to encourage support and participation of the partner or coach (Figure 8-1).
General Comfort Measures
General comfort can reduce stress and thus reduce pain. Also, comfort measures can encourage relaxation. It is important to eliminate sources of noxious (offensive) stimuli whenever possible. The nurse can try to relieve thirst, sweating, and heat through comfort measures. Providing ice chips and lollipops and repositioning the woman or adjusting the monitoring belts may provide relief.
Cognitive Stimulation
Several cognitive stimulation methods (mental stimulation) of pain control may be tried. Imagery (imagining a pleasant experience) can help the woman by serving as a distraction from the painful stimuli. Using a focal point or focusing on breathing patterns or a spot on the wall may help the woman block out painful sensations. This behavior requires her active participation.
Cutaneous Stimulation
Cutaneous stimulation, involving touching, rubbing, or massaging (back or shoulders), often decreases discomfort. Counter-pressure—a variation with the palm, closed fist, or firm object pressed at the point of back pain (sacral pressure)—is often helpful (Figure 8-2). Rhythmic stroking and massage of the abdomen (effleurage) during a contraction can also lessen discomfort (see Figure 5-13 and Chapter 21). Note that some women do not like to be touched.
Thermal Stimulation
During early labor, women may find a warm bath or shower relaxing. A cool, damp cloth applied to the forehead is especially comforting to some women in the later phases of labor. Hot or cold towels applied to the back may be effective, or the use of a shower or a disposable bottle filled with warm water can be used to provide warmth and mild pressure to the back.
Breathing Techniques
Breathing techniques change the focus during the contraction. There is no right or wrong breathing pattern, but rather the woman should use what she feels comfortable with (see Chapter 5). Breathing techniques can be taught to the unprepared woman while she is in labor (ideally during early labor). The nurse evaluates the breathing techniques used by the laboring woman.
Relaxation
Even if the woman has attended prenatal classes, she will need continued support in achieving relaxation of her voluntary muscles. The most effective teaching time, once labor has begun, is between contractions and during the first stage of labor.
Hypnosis
Hypnosis can be a powerful labor intervention that appears to be safe, is without known side effects, and has positive physical and psychological outcomes. With hypnosis, the woman retains a feeling of control. The nurse can optimize the woman’s hypnosis experience by understanding how his or her role in the labor room may be modified. Hypnosis is a technique that the mother may select during pregnancy; she is usually trained in self-hypnosis that can be used during labor. In the labor room, the nurse may help trigger self-hypnosis by using specific suggestions or playing specific audiotapes provided by the woman. The labor nurse must not interrupt the woman during a contraction when the woman is using self-hypnosis techniques. Characteristic signs of progression in labor may not be evident in a patient under hypnosis; therefore, careful observation and documentation concerning the progress of labor are essential.
Pharmacologic Pain Control Strategies
Physiology of Pregnancy and Its Relationship to Analgesia and Anesthesia
Specific factors in the physiology of pregnancy affect the pregnant woman’s response to analgesia and anesthesia:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree