Section 8. Chemotherapy
8.1. Cancer chemotherapy
In cancer there is uncontrolled multiplication of body cells that invade and destroy adjacent structures and spread to distant sites (metastasise). It can occur in most cell types and is named according to the tissue of origin – for example, cancer occurring in epithelial cells is carcinoma and in blood-producing cells is leukaemia. It does occur in most plants as well as animals.
Sometimes cancer is referred to as a malignant tumour or neoplasm and these terms have the same meaning.
▪ The rate of growth of malignant tumours varies as does their speed of spread around the body. Some cancers grow very slowly and others extremely quickly. Their response to treatment is also variable.
▪ Cancer cells are no longer within the body’s control and fail to respond to the regulation of cell division.
▪ They are also invasive and spread to other parts of the body by local invasion, the lymphatic system or the circulatory system. Cancers grow by progressive infiltration, invasion, destruction and penetration of surrounding tissue.
▪ Normally if a cell spreads outside its normal tissue it would die, but cancer cells do not. They can continue to grow in another organ so, for example, a breast cancer may spread to the brain and produce a secondary tumour there.
▪ Cancer occurs in 1 in 3 of the population in their lifetime and approximately 25% of people in the UK die from cancer.
▪ Treatment may be by surgical removal, chemotherapy, radiotherapy or sometimes all of these.
Cell division and cytotoxic drugs
The majority of cells consist of a nucleus surrounded by cytoplasm and a cell membrane. The nucleus contains the genetic material in the form of deoxyribonucleic acid (DNA) and this replicates in cell division. Also within the nucleus is ribonucleic acid (RNA) which determines the type of proteins manufactured by the cell.
▪ Most cytotoxic drugs target DNA or RNA but cannot do this just in the cancer cells. This means that normal body cells are also affected giving rise to side effects.
▪ Rapidly dividing cells are usually most sensitive to cytotoxic drugs. They are killed more readily as they are constantly reproducing their DNA.
The cell cycle
Some cells within the body have the ability to divide rapidly because they are constantly replaced as they wear out. Examples include the epidermis of the skin, the lining of the gastrointestinal tract and the blood-producing cells in the bone marrow. Other cells e.g. liver rarely divide but retain the ability to divide in organ damage and cells such as neurones have little or no ability to divide when mature.
The cell cycle is the period from the beginning of one cell division to the beginning of the next. It is the orderly sequence of events by which a cell duplicates its contents and divides in two.
▪ Cell division replaces dead or injured cells and adds new ones for tissue growth.
▪ When a cell divides, each original cell becomes two daughter cells.
▪ Both will be genetically identical to the parent cell.
The cell cycle involves five phases. These are G 1, S, G 2, M and G 0 and are shown in Figure 8.1. Interphase is the period from cell formation to cell division (G 1, S and G 2 phases), during which the DNA in the nucleus replicates.
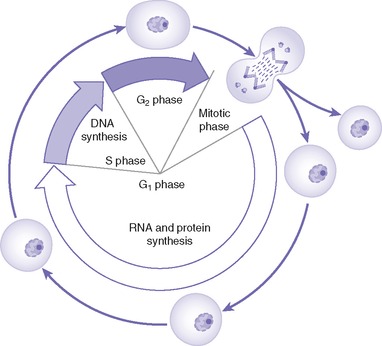 |
| Fig. 8.1 Phases in the cell cycle. Reproduced with permission from Trounce’s Clinical Pharmacology for Nurses, 17th edn, by Ben Greenstein, 2004, Churchill Livingstone, Edinburgh. |
G 1 phase
▪ Occurs immediately after a new cell has been produced.
▪ G stands for ‘gap’ or ‘growth’ and G 1 is the period between the end of cell division and DNA replication.
▪ It is a period of growth, RNA and protein synthesis.
▪ It is the most variable phase in terms of length. Cells with a rapid division time have a G 1 of minutes or hours in length. In those that divide slowly, it can last days or even years.
S phase
▪ It lasts about 6–8 hours but is variable.
G 2 phase
▪ This is the second gap phase and growth continues.
▪ It is very brief, about 4–6 hours.
▪ Synthesis of enzymes, RNA and other proteins needed for division is completed.
▪ Before mitosis can occur, the cell must approximately double its mass and contents.
M (mitotic) phase
Division of the cell that involves both division of the nucleus and of the cytoplasm.
The duration varies according to the type of cell; it is typically about 2 hours from start to finish.
G 0 phase
The cell is in a resting state. In adult tissue, not all cells divide at once and many are in this resting state.
Control of cell division
▪ Chemical signals released by other cells and the availability of space have an influence.
▪ Normal cells stop dividing when they are touching. This is contact inhibition and it is lost in cancer cells.
▪ Doubling time is the time a cancer cell takes to complete the cell cycle once.
▪ Cancer cells may not complete the cell cycle more rapidly than normal cells and some take much longer.
Drugs used in cancer chemotherapy
Drugs were first used to kill cancer cells in the 1970s and the number available has been steadily increasing. As understanding of cellular biology and cell death increases, new drugs with greater selectivity for the cancer cell are likely to be developed.
Mechanism of action
Most drugs target the rapidly dividing cancer cell although they have a variety of mechanisms and act at different points in the process of DNA synthesis during the cell cycle.
▪ By targeting the rapidly dividing cell the drugs affect our normal body cells less but will attack those cells that are still dividing regularly such as the lining of the gastrointestinal tract. Because of this, many cancer drugs have the same side effects and are extremely toxic.
▪ Cells that are resting in the G 0 phase are resistant to many anticancer drugs.
▪ Sensitivity of the cancer depends on the number of its cells that are in the growth phase when the anticancer drug is given.
▪ We can sometimes target different points of the cell cycle with different drugs.
▪ Burkitt’s lymphoma is an extremely fast-growing cancer and nearly all the cells are in the growth phase. It is extremely responsive to even one dose of chemotherapy.
▪ In slow-growing tumours such as most types of colorectal cancer only about 5% of cells are in the growing phase and this makes the tumour relatively insensitive to chemotherapy.
▪ Complete eradication of the cancer is needed or the growth can recur. This is not usually possible because of the side effects of the drugs.
▪ Drugs kill a certain percentage of cells each time they are given and so multiple treatments are needed.
▪ Sometimes clinical remission is induced in fast-growing tumours such as acute myeloid leukaemia and small-cell lung cancer, but if all cells are not eradicated the fast-growing cells can quickly produce a clinical relapse.
Resistance
Cancer cells may develop resistance to chemotherapy by several different mechanisms. They may:
▪ reduce drug uptake by a transporter as in methotrexate
▪ inactivate the drug as with cisplatin
▪ increase removal of the drug from the cancer cell by a glycoprotein pump as occurs with multiple drug resistance (MDR) to unrelated compounds such as etoposide and taxanes. The pump can be inactivated by unrelated drugs such as nifedipine, ciclosporin and tamoxifen. More effective inhibitors are being developed
▪ decrease the activation of a prodrug as with cytarabine
▪ reduce sensitivity of the target of the anticancer drug as with anthracyclines.
Unwanted effects of drugs
Rapidly-growing cells in normal body tissue are often affected by cytotoxic drugs. Many have a therapeutic index of 1, meaning that the dose needed to be effective is also the toxic dose. They are the most toxic group of drugs used in therapeutics and courses have to be planned so that healthy cells such as those in the bone marrow can recover between doses of the drug. The cancer cells do not recover as fully and so more are eradicated with each dose of the drug.
The adverse effects listed here are common to many anticancer drugs.
Nausea and vomiting
This can be severe with high doses of certain drugs. It is worse with cisplatin, cyclophosphamide and dacrabazine and may limit the patient’s tolerance of the drug.
▪ Patients vary in their susceptibility to nausea and vomiting but it often increases with the number of treatments.
▪ The most effective antiemetics are the 5-HT 3 antagonists such as ondansetron and in those at high risk of vomiting this may be combined with other drugs such as the corticosteroid dexamethasone or the anxiolytic lorazepam.
▪ Aprepitant is a neurokinin 1 receptor antagonist licensed to control vomiting with cisplatin.
▪ Nabilone is a synthetic cannabinoid that may be used if patients are unresponsive to other antiemetics.
▪ The cytotoxic drug may be given at night so that the patient can be sedated and sleep may reduce the nausea.
▪ Antiemetics are given 24 hours before starting the therapy and continuously to prevent symptoms.
▪ Delayed nausea and vomiting may occur more than 24 hours after treatment. This is best controlled using dexamethasone often combined with an antiemetic such as metoclopramide.
Bone marrow suppression
All cytotoxic drugs except vincristine and bleomycin cause bone marrow suppression usually 7–10 days after they are given but this may be longer in some cases. This leads to a fall in blood cells, especially white cells, and so increased risk of infection by bacteria, viruses and candidiasis (thrush).
▪ The treatment cannot be given if the WCC is too low because the bone marrow has not recovered from the last drug treatment.
▪ If the temperature is raised in those with a low WCC it must be treated immediately with a broad-spectrum antibiotic as sepsis may be fatal.
▪ Sometimes bone marrow growth factors may be given.
▪ Red cell transfusions are used to treat anaemia.
Sore mouth
This is a common complication especially with fluorouracil, methotrexate and the anthracyclines.
▪ The aim is to prevent mucositis and ulceration by good mouth care. This includes rinsing the mouth frequently and brushing the teeth with a very soft toothbrush.
▪ Ice chips may be sucked during short infusions of fluorouracil.
▪ The sore mouth is difficult to treat when it has occurred.
▪ Saline mouthwashes may be given.
Gastrointestinal tract
Ulceration here may be associated with diarrhoea.
Alopecia
Reversible hair loss occurs with many drugs due to the effect on the hair follicle.
Reproductive function
Most of these drugs are teratogenic and so should not be administered in pregnancy, especially the first 3 months.
▪ Contraception should be used prior to, during and for a period following therapy.
▪ In women, menstrual irregularity or amenorrhoea may occur.
▪ Occasionally infertility may occur and is commoner with alkylating agents. This is more frequent in women over 35 and men. Sperm may be banked prior to therapy.
▪ Women may have a shortened reproductive life and an early menopause.
Tumour lysis syndrome
This is due to the breakdown of so many cells.
▪ Features include raised levels of potassium, uric acid and phosphates but low levels of calcium in the blood.
▪ It may lead to renal damage and cardiac arrhythmias.
▪ Allopurinol is used to prevent hyperuricaemia and is given prior to treatment in certain lymphomas and leukaemias where this is common.
▪ The patient should be well hydrated.
Thromboembolism
There is an increased risk in cancer and this is raised when chemotherapy is used.
Growing tissues
▪ Cytotoxic drugs can impair growth in children.
The individual groups of drugs will now be listed and briefly described under the headings of their mechanism of action.
 Extravasation of intravenous drugs can lead to severe tissue necrosis and drugs must only be administered by those trained in their use.
Extravasation of intravenous drugs can lead to severe tissue necrosis and drugs must only be administered by those trained in their use.Specific cytotoxic agents
Those affecting DNA synthesis and function
Alkylating drugs
Cyclophosphamide, chlorambucil, busulfan, carmustine, lomustine, melphelan, thiotepa, treosulfam
▪ They damage DNA and so interfere with cell replication, preventing DNA and RNA synthesis.
▪ They are not cell cycle specific.
▪ Some may be given orally.
▪ Widely used group of drugs that were also some of the earliest to be licensed.
▪ First developed from nitrogen mustard gas used in the First World War as chemical warfare.
Unwanted effects
▪ Gametogenesis is severely affected giving impaired fertility.
▪ Long-term use is associated with an increased risk of acute myeloid leukaemia.
▪ Bone marrow depression and neutropenia.
▪ Pulmonary fibrosis with busulfan, carmustine and treosulfan.
▪ Skin pigmentation with busulfan and treosulfan.
▪ Haemorrhagic cystitis with cyclophosphamide and ifosfamide. This is prevented by treatment with mesna before therapy. There is an increased risk of bladder cancer years later.
Platinum compounds
Cisplatin, carboplatin, oxaliplatin
These enter cells and break the DNA chain by crosslinking guanine units. This is a similar action to the alkylating drugs.
▪ Used in ovarian and testicular cancer. Oxaliplatin is used in advanced colorectal cancer.
▪ Not absorbed well orally and are given intravenously.
Unwanted effects
▪ Severe nausea and vomiting especially with cisplatin.
▪ Nephrotoxicity with cisplatin so renal function must be monitored. Good hydration reduces the risk.
▪ Peripheral neuropathy may also occur.
▪ These effects are less with carboplatin but bone marrow suppression is greater.
▪ Ototoxicty that can result in tinnitus and deafness.
Topoisomerase I inhibitors
Cytotoxic antibiotics
Dactinomycin, doxorubicin, epirubicin, idarubicin (anthracyline antibiotics), bleomycin, mitomycin, mitoxantrone
Some increase reactive chemicals (free radicals) and these cause DNA damage.
Some cause breaks in the strands of DNA while others interfere with cell membrane function.
▪ Widely used drugs but many of them are radiomimetics and should not be used alongside radiotherapy as this increases toxicity.
▪ Not usually cycle specific.
▪ Not well absorbed so given intravenously.
Unwanted effects
Dozorubicin, epirubicin and mitoxantrone cause myocardial cell damage that is dose dependent.
Bleomycin and mitomycin cause dose-related pulmonary fibrosis.
Antimetabolites
Interfere with normal metabolism and prevent normal cellular division by either combining with enzymes needed or by being falsely incorporated into new DNA.
Methotrexate
Inhibits the enzyme dihydrofolate reductase and blocks the synthesis of purines and pyrimidines that are needed to make DNA, RNA and proteins.
▪ Active in the S phase of the cell cycle and slows G 1 to S phase.
▪ Used in acute lymphatic leukaemia and nonHodgkin’s lymphoma.
▪ Is also used to treat nonmalignant conditions such as rheumatoid arthritis and psoriasis.
Unwanted effects
Include bone marrow suppression and pulmonary fibrosis with chronic administration.
▪ Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin may reduce renal excretion and so increase blood levels into the toxic range.
▪ Folinic acid ( leucovorin) is often administered after high doses to provide folate and rescue some of the normal body tissues so reducing suppression of the bone marrow and inflammation of mucous membranes.
Base analogues
Capecitabine, cladribine, cytarabine, fludarabine, fluorouracil, gemcitabine, mercaptopurine, talitrexed, tegafur, tioguanine
▪ These drugs have been produced by modifying purine and pyrimidine bases and so interfering with DNA synthesis.
▪ Suppression of the bone marrow is usually severe.
Capecitabine is metabolised to fluorouracil. It is given alone or with oxaliplatin in treatment of advanced colorectal cancer. It is also used in gastric cancer.
Cytarabine is used to produce a remission in acute myeloid leukaemia.
Gemcitabine is first-line treatment for pancreatic cancer where surgery is not possible.
Details of other drugs in this group can be found in the British National Formulary (BNF).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
