Care of Patients with Cancer
Objectives
1. Identify characteristics of neoplastic (abnormal tissue) growth.
2. Identify at least five factors that may contribute to the development of a malignancy.
3. State at least four practices that can contribute to prevention and early detection of cancers.
5. Explain the advantages and disadvantages of the various treatments available for cancer.
7. Distinguish the stages of the grieving process experienced by the dying cancer patient.
1. Devise a general plan of nursing care for the patient receiving chemotherapy.
2. Formulate a teaching plan for the patient who has bone marrow suppression from cancer treatment.
5. Employ nursing interventions to help the cancer patient cope with death and dying.
Key Terms
benign (bĕ-NĪN, p. 145)
biopsy (BĪ-ŏp-sē, p. 153)
carcinogens (kăr-SĬN-ō-jĕnz, p. 147)
carcinoma (kăr-sĭ-NŌ-mă, p. 146)
cytology (sī-TŎL-ō-jē, p. 151)
cytotoxic (sī-tŏ-TŎK-sĭk, p. 162)
deoxyribonucleic acid (DNA) (dē-ŏx-ē-rī-bō-nū-KLĀ-ĭc ĂS-ĭd, p. 145)
encapsulated (ĕn-KĂP-sū-lāt-ĕd, p. 145)
hematoma (hē-mă-TŌ-mă, p. 146)
incidence (ĬN-sĕ-dĕns, p. 144)
leukemia (lū-kĒ-mē-ă, p. 146)
lymphoma (lĭm-FŌ-mă, p. 146)
malignant (mă-LĬG-nănt, p. 145)
melanoma (mĕl-ă-NŌ-mă, p. 146)
metastasis (mĕ-TĂS-tă-sĭs, p. 146)
mutation (mū-TĀ-shŭn, p. 147)
neoplasm (NĒ-ō-plăzm, p. 145)
occult blood (ŏ-KŬLT blŭd, p. 151)
oncogenes (ŎNGK-ō-jēnz, p. 147)
palliative care (PĂL-ē-ă-tĭv, p. 172)
prognosis (prŏg-NŌ-sĭs, p. 146)
promoters (prō-MŌ-tĕrz p. 148)
sarcoma (săr-kŌ-mă, p. 146)
TNM staging (p. 146)
transformation (trănz-fĕr-MĀ-shŭn, p. 149)
tumor markers (TŪ-mŏr, p. 154)
vesicants (VĔ-si-kĕnts, p. 163)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
The Impact of Cancer
Cancer is a group of diseases that characteristically grow in an uncontrolled manner with the spread of abnormal cells. In many instances, however, the growth can be controlled by specific treatment. In the early 1900s, there was little hope for survival once cancer was detected. This year, 4 of 10 people who are diagnosed with cancer will be alive in 5 years.
Excluding skin cancer, about 1,529,560 new cases of invasive cancer will be diagnosed in 2010 (American Cancer Society [ACS], 2010). It is estimated that an additional 1 million people in 2010 will be told that they have squamous cell skin cancer. The current rate of cancer is about the same as that of 1977, indicating little advance in the rate of cancer occurrence. The incidence of lung cancer in men declined during 2010 and the incidence in women stabilized. However, the incidence of breast cancer has increased over the past three decades and is mostly attributed to improved detection.
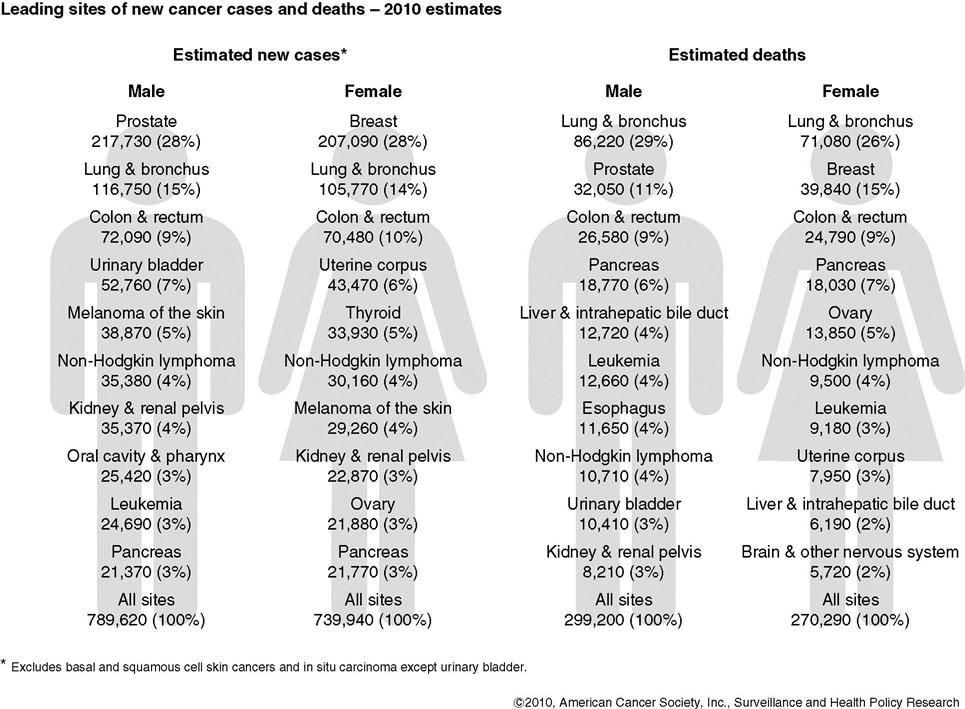
Death rates for many other major cancers have stabilized or declined since the 1930s. However, cancer still accounts for one in four deaths in the United States today. About 569,490 people will die from cancer in 2010 (1500 people per day). On the other hand, there are 11.1 million living Americans who have a history of cancer, and 68% of them were diagnosed over 5 years ago. That means that 66% of cancer patients are surviving. Because of earlier detection and improvements in treatment methods, patients who are diagnosed today may have much higher survival rates. More people can survive cancer if it is treated in its earliest stages. In fact, the American Cancer Society (ACS) estimates that if all the cancers that are detectable early were diagnosed in localized stages, the 5-year survival rate would be 95%. Figure 8-1 shows the leading sites of new cancer cases and deaths.
Physiology of Cancer
The human body is continuously producing new cells to replace those cells that are worn out, and to repair damage done to cells by illness and injury. An abnormal replication of cells results in a neoplasm (new growth of tissue, or tumor), which is not beneficial. The word benign indicates a neoplasm that is usually harmless. Benign growths are almost always encapsulated (surrounded by a fibrous capsule). The capsule prevents the release of cells and restricts their spread to other parts of the body. Benign growths can, however, create problems if they press against and interfere with the normal structure and function of nearby organs.
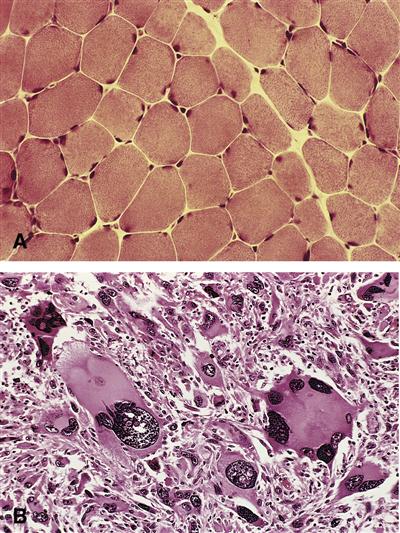
The cells of malignant (uncontrolled growth that can lead to death) growths are quite different from normal cells. Cells that exhibit malignant growth are known as cancer. Cancerous growth changes a cell’s deoxyribonucleic acid (DNA) makeup and function, and also the DNA structure and function of cells that are replicated; hence, cancer cells do not look like or behave like normal cells (Figure 8-2). DNA is the material that contains the genetic makeup of all future generations of a cell.
The nucleus of a malignant (cancer) cell is large and irregular. As the cancer cell divides and duplicates, it fails to follow the rules that regulate the reproduction of normal cells. Malignant cells do not seem to “know” when to stop multiplying. The offspring of cancerous cells proliferate (multiply) in great numbers, and they grow more and more disorganized, often forming tumorous masses. Some cancerous cells take on new characteristics, so that they do not resemble the cells of the original tissue. The malignant cells invade neighboring tissues and travel to other parts of the body. There they establish another colony of malignant cells. Their demand for nutrients depletes the supply of nourishment available for normal cells. This spread of tumor cells is called metastasis (movement of cancer cells from the original cancer site to other areas of the body). Not all malignant cells metastasize, but the great majority of malignant cells do.
Classification of Tumors
Tumors are often classified according to the organs or tissues from which they first began to grow; alternatively, tumors are classified according to the substances of which they are formed. The suffix -oma means tumor; this suffix is used in the names of various kinds of growths or swellings. Remember that -oma simply means tumor; the suffix -oma can designate any swelling, including a swelling in which there is a collection of fluids, as well as a swelling containing malignant cells. For example, hematoma (another word for bruise) is a combination of hema-, meaning blood, and -oma, meaning a swelling or collection of fluid or cells.
The prefixes used in classifying neoplasms indicate the kind of tissue in which they originate. For example, a tumor arising from fatty (lipoid) tissue is called a lipoma. A fibroma is a tumor composed of fibrous tissue. A leiomyofibroma contains both smooth-muscle tissue and fibrous connective tissue. Lipomas, fibromas, and leiomyomas are the most frequently occurring types of benign growths.
Malignant growths are divided into four main types. A sarcoma arises from mesenchymal tissues (bone, muscles, and other connective tissues). A carcinoma originates in epithelial tissues (skin and mucous membranes). These kinds of cancers make up the majority of cancers of the stomach, uterus, lungs, skin, and tongue. Leukemia and lymphoma are cancers of the blood-forming system. Malignancy of the pigment cells of the skin is called melanoma.
These are the main groups of cancers. More accurate naming can be done by adding modifying prefixes. For example, osteosarcomas arise from bone (osteo-), and adenocarcinomas arise from glandular (adeno-) structures.
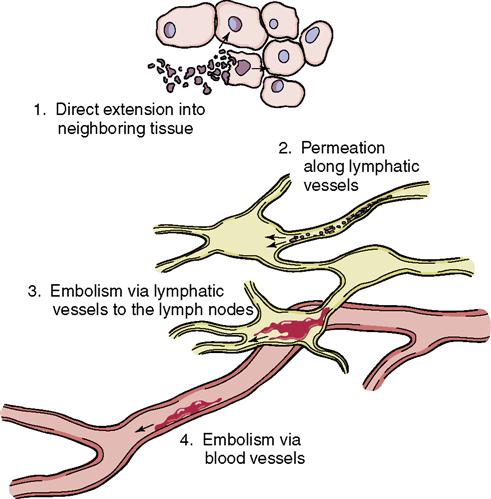
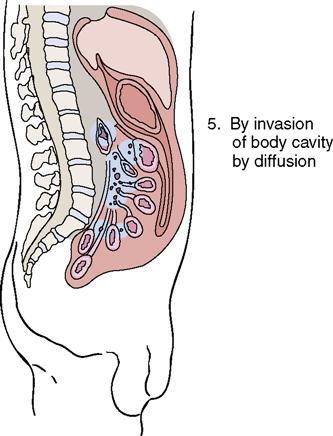
Metastasis
The word metastasis means the movement of cells from one part of the body to another. Metastasis refers to the moving of these malignant cells to another site. Malignant cells can metastasize by traveling in the blood and body fluids, in much the same way as do bacterial cells. It also is possible for free malignant cells to be directly transplanted from one organ to another during surgery when gloves and instruments that have these cells on them serve as vehicles for their transportation. Another way in which malignant cells can “contaminate” normal tissues and organs is by entering a body cavity and coming in contact with a healthy organ. For example, malignant cells may break off from a diseased organ, enter the abdominal cavity, and attach themselves to an ovary or the mesentery (tissues that connect the internal organs to the abdominal cavity wall) (Figure 8-3).
The prognosis (prediction of survival) for a patient with a malignancy depends on how much the malignant cells have attacked body tissues. A localized growth is one that remains at the original site (in situ) and has not yet released its cells, even though the growth may have invaded underlying tissues. At this stage the disease is much more easily destroyed.
A regional malignancy is one in which cells from the original malignancy have spread to the body area around the tumor, such as to nearby lymph nodes. The spread has been limited by the body’s protective mechanisms. These cells may continue to grow and multiply, and if the regional cancer is not successfully treated, malignant cells will eventually break away and spread throughout the body. This creates an advanced cancer that is often fatal.
One system that identifies cancers by how much the malignancy has spread is the TNM staging system. The three basic parts of the system are T for primary tumor, N for regional nodes, and M for metastasis. The number written beside each letter indicates how much the malignancy has spread and attacked other tissues. For example, T1, N0, M0 means that the tumor is small and localized (no involvement of regional lymph nodes and no metastasis). A label of T1, N2, M1 indicates a small (T1) tumor with moderate regional involvement (N2) that has metastasized to one distant site or organ (M1).
For example, T1, N0, M0 means that the tumor is small and localized (no involvement of regional lymph nodes and no metastasis). A label of T1, N2, M1 indicates a small (T1) tumor with moderate regional involvement (N2) that has metastasized to one distant site or organ (M1).
Causative Factors
All cancer results from defects in the DNA of genes. These defects either are inherited or are caused by mutation (a permanent change in the DNA sequence of a gene) during a person’s lifetime from exposure to chemicals or radiation. Several cancer-causing genes (oncogenes) are discovered each year. Oncogenes are mistakes in the instructions inside a cell’s DNA genetic code, whereby newly created cells are no longer normal. The defective gene tells the new cells to multiply at a higher rate. Also, the defective coding prevents newly created defective cells from dying and being reabsorbed. This results in a tumor, or mass.
Tumor suppressor genes are healthy, normal genes that control the growth of cells in the body. Each person’s body has a different ability to withstand the effects of cancer-causing substances (carcinogens), to mount a healthy immune response, and to repair damaged DNA. It is hoped that discoveries in molecular biology will allow individual risk profiles to be drawn that could be used to counsel people to avoid certain occupational and environmental exposures or to develop protective therapies.
In the external environment, many harmful agents exist that are known to be carcinogenic, and others are strongly suspected. Among these harmful agents are certain chemicals, sources of radiation, and viruses (Table 8-1). There are also some internal factors that affect an individual’s ability to cope with malignant cells. Hormones play an undetermined role in the development and progress of cancer, and several inherited genes have been discovered that increase a person’s chance of getting certain types of cancer. In some families there is a tendency to develop cancer in particular organs. This is shown in certain high-risk groups, described later in this chapter.
Table 8-1
Common Carcinogenic Substances
| Substance | Type of Cancer |
| Asbestos | Lung, peritoneal, pericardial |
| Benzene | Acute myelocytic leukemia |
| Tobacco | Lung, mouth, pharynx, larynx, esophagus, pancreas, bladder, kidney |
| Alcoholic beverages | Mouth, pharynx, larynx, esophagus, liver |
| Ionizing radiation | Leukemia, tumors of most organs |
| Sunlight (ultraviolet rays) | Skin |
| Diethylstilbestrol (prenatally) | Vagina |
| Estrogens, synthetic | Endometrial |
| Androgens, synthetic | Liver |
| Vinyl chloride | Liver |
| Aromatic amines | Bladder |
| Arsenic (inorganic) | Lung, skin |
| Chromium | Lung |
| Nickel dust | Lung, nasal sinuses |
| Chronic hepatitis B or C infection | Liver |
| Human T-cell lymphotropic virus type 1 (HTLV-1) | Adult T-cell leukemia and lymphoma |
| Human papillomavirus (HPV) | Cervix, mouth and throat |
| Phenacetin | Renal pelvis, bladder |
| Alkylating agents (used for chemotherapy) | Acute myelocytic leukemia |
| Cyclosporine (used to prevent transplant rejection) | Non-Hodgkin’s lymphoma |
Another factor that enters into the development of a malignancy is age. Although cancer can strike at any age, older people are more susceptible. Immunocompetence, or the capability of one’s immune system to deal with foreign cells—bacterial, viral, or malignant—is an important factor in the development of cancers; immunocompetence decreases with aging.
Chemical Carcinogens
More than 200 years ago (1775), Sir Percival Pott linked the occurrence of cancer to a substance in the environment when he observed that cancer of the scrotum was common among the chimney sweeps of London. He attributed this high incidence of cancer to repeated accumulations of soot on the skin of these young men, whose occupation required continuous contact with the coal soot in the chimneys they cleaned. Since that time, almost 500 different chemical carcinogens have been identified.
Many of the cancer-producing substances in the environment are related to occupations that involve repeated exposure to certain substances that are handled or inhaled. Petrofluorocarbons (polychlorinated biphenyls or PCBs) and some pesticides (e.g., DDT) are known carcinogens. These and other such chemicals decrease immunocompetence. For example, cancer of the skin often is related to the handling of pitch, asphalt, crude paraffin, and petroleum products. Lung cancer is linked to irritating substances in the air, such as tobacco smoke, asbestos, and chemical wastes from industry and automobiles. Cancer of the bladder is associated with certain substances in aniline dyes, which are present in the environment of workers in that industry. Vinyl chloride, nickel, arsenic, and chromate are linked to cancers in workers in industries that use those chemicals. Benzene, an ingredient in older unleaded gasoline, is linked to leukemia. These are but a few of the chemical agents that can contribute to the development of cancer in humans.
Chewing tobacco has been directly related to cancer of the tongue and structures of the mouth and throat. Cigarette smoking is a known direct cause of cancer of the lung and is thought to be linked to esophageal, pancreatic, bladder, and kidney cancers.
Immunosuppressive drugs used to suppress organ transplant rejection are a cause of non-Hodgkin’s lymphoma. Synthetic estrogens are linked to a higher incidence of endometrial cancer. Many cancer drugs affect the immune system and can predispose to other types of cancer.
Promoters
Promoters are substances that are not carcinogenic when found alone, but when they are in a person’s body with a known carcinogen, cancer occurs faster. Alcohol is such a substance. When nicotine is present, cancers occur at a faster rate in those who are heavy consumers of alcohol than in those who use nicotine but do not drink alcohol. It is thought that about 90% of all head and neck cancers are tobacco plus alcohol related.
Chronic Irritation
In one of the earliest theories about the causes of cancer, a skin cancer was attributed to long-term chronic irritation of the skin and mucous membranes. Although this condition may be a contributing cause of cancer, chronic irritation alone usually does not lead to malignancy. There must be other factors present, particularly a mole on the skin and/or exposure to a chemical carcinogen or ultraviolet rays, in order for the skin cancer process to begin.
Research on chemicals that may have this same type of influence is ongoing. Most likely the second substance involved, although not directly carcinogenic, has a harmful effect on the immune system, making the person more susceptible to malignant cell growth.
Physical Carcinogens
Radiation
Radiation may originate from x-ray machines and radioactive elements or from the ultraviolet rays of the sun. These rays are capable of penetrating certain body tissues and causing the development of malignant cells in the affected area. The relationship of intense and prolonged exposure to these rays and the production of cancer cells was first discovered when it was noted that there was a high incidence of cancer, particularly leukemia, among people who pioneered studies of x-rays, or worked with radium or uranium. Later it was found that survivors of atomic blasts at Hiroshima and Nagasaki at the end of World War II suffered an unusually high incidence of leukemia.
There is continued concern about the danger that excessive radiation in the environment presents, especially the long-term effects that are not immediately apparent but may eventually prove to be related to malignancy. In addition to leukemia, cancers of the skin, bone marrow, breast, lung, and thyroid are believed to be closely linked to exposure to radiation.
The ultraviolet rays of the sun can produce skin cancer. The deterioration of the Earth’s ozone layer is causing more ultraviolet rays to reach the earth than in the past, which compounds the problem. The susceptibility of the individual also is a factor: people with fair complexions have less protective pigment and therefore are more likely to develop skin cancer from ultraviolet radiation than are people with darker skin.
Radon Gas
People who live in areas that have more radon emission from the earth have a higher incidence of malignancy in the population than people in areas that are low in radon.
Viruses
In recent years, extensive research has been directed toward establishing a link between viruses and malignancy. Experiments involving animals have demonstrated that a number of cancers can be produced in animals by injecting them with a filtrate from virus-infected malignant growths. The hepatitis B virus is carcinogenic for liver cancer. The Epstein-Barr virus causes Burkitt’s lymphoma. Cases of adult T-cell leukemia and lymphoma are caused by human T-cell lymphotropic virus. Several types of the human papillomavirus (HPV) cause cervical carcinoma and are related to throat and mouth cancer in nonsmokers. These viruses are known as oncoviruses because of their ability to cause cancer.
After the transformation (change into something else) of a normal cell into a precancerous state, the malignant cell requires many conditions favorable to its multiplication and growth into a cancerous tumor. Viruses are capable of introducing new genetic material into a normal cell and transforming it into a malignant one. Furthermore, cell reproduction can be altered when viruses interact with carcinogens. Viruses such as the human immunodeficiency virus (HIV) can damage the immune system and decrease immunocompetence, causing the body to become more susceptible to the growth of abnormal cells. Such damage also reduces the body’s ability to fight off cancer-causing viruses, such as HPV. Some cancers—such as Kaposi sarcoma—are only seen in HIV-infected or severely immunocompromised patients (see Chapter 11 for more information).
Genetic Predisposition
All cancers are caused by genes that malfunction and cause the overgrowth of cells. Research is revealing that there is a genetic predisposition to various types of cancer. It has been known for many years that breast cancer is more likely to occur in women who have a close female relative who developed breast cancer before age 50. Gene markers have been found for colon cancer, breast cancer, prostate cancer, pancreatic cancer, and leukemia. However, only 5% to 10% of cancers are related to a directly inherited gene. The remaining cancers are caused by genes that are damaged (mutated) throughout the lifetime, and are not inherited. Some people are more susceptible to these mutations.
With the completion of the Human Genome Project, scientists are working to identify the genes that are related to specific cancers (National Cancer Institute, 2011). Currently, research is focused on finding genetic markers—or oncogenes—for other forms of cancer. Such markers, or the proteins they produce, could identify high-risk individuals who then might undergo more vigorous, regular diagnostic testing to detect any malignancy in the very earliest stages. Since several cancers have precursor lesions (such as adenomatous polyps in the colon) such early discovery would greatly increase survival rates.
Contributing Factors
Intrinsic Factors
Age, sex, and race are considered “predisposing factors” for certain types of cancers. Predisposition simply means that, statistically, certain types of cancer strike particular age, sex, or racial groups more frequently than others. For example, prostate cancer is far more common in black males than in white males. The incidence of cervical cancer is higher in black women than in white women. Breast cancer is more prevalent in white women than in Asian women. As for age factors, approximately 76% of cancers occur in people age 55 and older.
Stress
Another factor that seems to play a role in the development of cancer is stress. Considerable stress over long periods has an adverse effect on the immune system; stress can make the immune system less effective in ridding the body of invading organisms and stress decreases the body’s ability to destroy abnormal cells. Stress is one more factor that may tip the scales in favor of the growth of malignant cells. When one partner of a long-term relationship dies, the stress of the loss and adjustment to life without the partner seems to increase the likelihood of cancer in the surviving partner.
Diet
Most experts agree that approximately 30% of cancers could be reduced through proper nutrition and exercise. There is strong evidence that healthy diet and normal body weight are crucial in the control of cancer. Cancers of the breast, colon, rectum, endometrium, esophagus, uppermost abdomen, gallbladder, pancreas, liver, and kidney are all linked to excess weight and obesity. Although there is no universal agreement about the role of fiber in the prevention of malignancy, high-fiber foods such as fruits, vegetables, and cereals are recommended as a wholesome substitute for fatty foods.
Measures to Prevent Cancer
The nurse can be instrumental in educating the public about ways to prevent cancer. Each nurse should teach patients the following measures at every opportunity.
Diet and Nutrition
Encourage maintenance of normal weight. Obesity is considered a risk factor in many cancers. It also makes early detection of many cancers difficult. One study noted that men and women who were overweight by 40% or more have a 33% and 35% greater risk, respectively, for developing cancer than do persons with normal weight.
Nitrite and nitrate food additives are also known to be cancer stimulators (encouraging cancer). However, research has indicated that if foods containing nitrites are eaten in combination with foods containing vitamin C (ascorbic acid), the formation of nitrosamines is blocked. This means, for example, that if orange juice is consumed along with a meal containing bacon, there is less chance of carcinogenic nitrosamines damaging the body. In this instance, the vitamin C is a cancer inhibitor (discouraging cancer).
These recommendations are from a report by a special committee on nutrition and cancer and are based on studies conducted for more than 20 years by the ACS’s research program. Although no direct cause-and-effect relationship between diet and cancer has been demonstrated, there is ample evidence that avoidance of obesity and modification of the diet can help prevent some types of cancers.
Alcohol
Moderation in the drinking of alcohol is recommended, because alcohol consumption alone has been shown to increase risk for several cancers. Excessive alcohol consumption also can lead to liver damage, and possibly to liver cancer.
Environment
Because groundwater is so often contaminated with chemicals that have leached into it from fertilizers, pesticides, and industrial wastes, it is wise to know the chemical makeup of the local water supply. If the geographic area is highly contaminated, filtered or bottled water might help prevent further damage to immunocompetence, and thereby decrease the incidence of cancer.
Identifying High-Risk People
Studies of individuals who have developed cancer—their medical history, lifestyle, and family history—have shown that some people are more likely to develop certain kinds of cancer. Table 8-2 shows information on high-risk groups published by the ACS in order to develop an awareness of the need for frequent and thorough examinations to detect cancer early in those who are susceptible to developing a malignancy.
Table 8-2
| Type of Cancer | Risk Factors | Signs |
| Lung | Persistent cough, blood in the sputum, chest pain, recurring pneumonia or bronchitis | |
| Breast | Lump in breast, nipple discharge, thickening, dimpling, nipple retraction, pain or tenderness of the nipple | |
| Colon-rectum | Blood in stool; alteration in bowel pattern (e.g., constipation alternating with diarrhea) | |
| Uterine-cervical | Unusual bleeding or discharge | |
| Uterine-endometrial | Unusual bleeding or discharge | |
| Skin | Change in the size, color, or appearance of a mole or spot on the skin; scaliness, oozing, bleeding or change in appearance of a bump or nodule; spread of pigmentation beyond the border; change in sensation of any skin lesion | |
| Oral | White patch in the mouth or on the tongue; nodules | |
| Ovary | None until well advanced | |
| Prostate | Difficulty urinating; hesitancy, blood in the urine; need to urinate frequently; pain in lower back, pelvis, or upper thighs | |
| Stomach | Nonspecific; indigestion, feeling of fullness or pressure; pain and weight loss are late signs | |
| Pancreas | No signs | |
| Bladder | • Smoking | Painless blood in the urine; need for frequent urination |
| Leukemia | Frequent infections, easy bruising, fatigue, weight loss, nosebleeds, paleness |
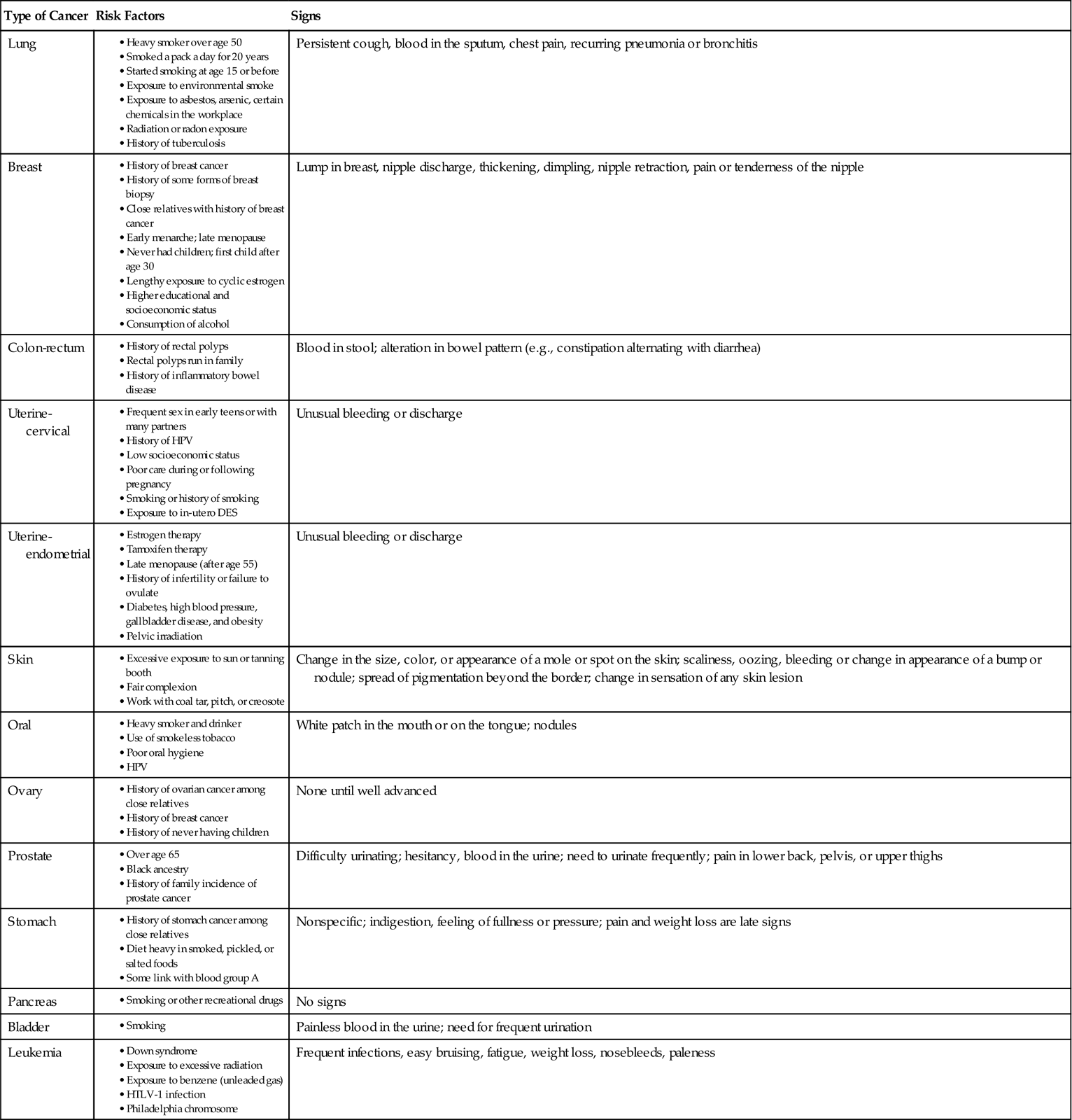
DES, diethylstilbestrol; HPV, human papillomavirus; HTLV-1, human T-cell lymphotropic virus type 1.
Detection of Cancer
Cancer is a group of diseases. It can strike any organ of the body, affect different organs with different functions, and therefore can present an untold number of symptoms as it progresses. To be able to identify the symptoms of cancer in its earliest stages, it is important to be aware of its warning signals. The purpose of screening large segments of a population is to identify as many people with cancer as possible.
In addition to the medical history and thorough physical examination that are essential components of any health status evaluation, the health care professional also conducts certain tests to determine whether a malignancy is present. Recommendations of the ACS for routine checkups and early detection of cancer are shown in Box 8-1.
One widely used technique to detect cancer is to examine cells under a microscope to determine whether they are malignant or premalignant. This technique is called cytology, and the most widely used cytology test is the Papanicolaou (Pap) smear to detect cervical cancer. A cytologic examination can be done by obtaining a sample of secretions containing cells that have been released from adjacent tissue. The technique involves either scraping or brushing a sample of cells from the area or collecting body secretions that contain cells. These secretions may be cervical discharges, sputum, gastric washings, pleural fluid, or urinary washings. The specimen is placed on a slide or put in a liquid medium and sent to a laboratory, where a specially trained technologist or pathologist examines the cells microscopically. If “suspicious” cells are found, the patient is referred to a health care professional for more extensive diagnostic tests. Another screening technique, used for colorectal cancer, is the simple test for occult blood (hidden blood) in the stool. This can be obtained through a fecal occult blood test (FOBT) or a newer test called the fecal immunochemical test (FIT). The person simply collects one or more stool specimens (depending on the particular test being used), applies a thin smear on the container provided, and returns the specimens to the health center, clinic, or clinical laboratory. Occult blood in the stool is not always an indication of cancer of the bowel or rectum. Other conditions also can produce this symptom.
Research continues on identifying proteins produced by mutated DNA that might be used to diagnose various types of cancer. These tests may soon be available for those at high risk for bladder, cervical, lung, breast, colon, and prostate cancer. If these tests prove reliable, they may well be incorporated into a normal part of routine medical care.
Other procedures used to identify lesions that are possibly malignant include radiologic studies, endoscopy, sonography, magnetic resonance imaging, computed tomography, clinical laboratory testing of enzymes and other substances in the blood, and studies specific to the system in which the cancer is suspected. Tests for viruses are now being done to identify increased risk for some cancers. For example, a test for the presence of high-risk types of HPV is available to identify women at risk for cervical cancer.
Diagnostic Tests
Biopsy
Biopsy of a tumor and examination of the cells obtained are the most certain techniques for establishing a diagnosis of malignancy in most neoplasms. Malignancies involving blood cells, such as in leukemia, are diagnosed by examining these cells. A biopsy is the removal of living cells for the purpose of examining them under a microscope. The cells may be removed by surgical excision (cutting out) of a small part of a tumor, by the aspiration (suction) of cells through a needle introduced into the growth, or by brush biopsy. If the tumor is small, the entire growth may be removed. The specimen obtained is examined under the microscope by a pathologist.
If the sample is taken in the operating room and the surgeon is waiting for the results to determine the extent of surgery needed to remove all the malignant cells, the tissues may be frozen for quick examination. This technique is called preparing a frozen section.
New procedures, such as fine-needle aspiration (FNA) and percutaneous (through the skin) large-core breast biopsy, are used for diagnosing breast cancer without the disfigurement of traditional surgical breast biopsy. Breast biopsy is combined with imaging techniques such as ultrasound to verify correct placement of the biopsy needle. Then FNA is combined with computer analysis of the samples obtained.
Radiologic Studies
Mammography is a radiologic examination of the breast that is useful in diagnosing malignant growths, and x-ray films are particularly helpful in diagnosing bone and hollow organ tumors. Mortality rates can be cut by 31% when routine mammography screening is performed (Tabar et al., 2003 ). The respiratory, digestive, and urinary tracts can be visualized on a radiograph if a radiopaque (not penetrated by the x rays) substance is used. The substance passes through the hollow organ and, since it is radiopaque, the inner structure of the organ is clearly demonstrated on the radiograph.
). The respiratory, digestive, and urinary tracts can be visualized on a radiograph if a radiopaque (not penetrated by the x rays) substance is used. The substance passes through the hollow organ and, since it is radiopaque, the inner structure of the organ is clearly demonstrated on the radiograph.
Another radiologic technique involves the use of a radioactive substance (radionuclide or isotope) that is given to the patient before the x-ray filming. The isotope is a “tumor-seeking” chemical that searches for the tumor and may or may not concentrate around it. A special scanning apparatus moves back and forth over the subject’s body; as the scanner moves, it records information about the concentration of the isotope in the area being examined. If the substance is concentrated in the tumor, the growth shows up as a “hot spot” on the screen of the scanning apparatus. If the tumor does not accept the isotope, the normal tissue around the tumor concentrates the isotope, and the tumor shows up as a “cold spot.” This technique is commonly used in the investigation of thyroid tumors.
A commonly used radiologic scanning technique is computed tomography (CT) scanning. This method is noninvasive and involves relatively small amounts of radiation exposure for the subject. The term noninvasive means that no surgical procedures are needed to reveal the size, shape, contour, and density of an organ. The procedure requires minimal preparation.
In CT scanning, the x-ray source moves past the subject in one direction while the film moves in another. In this way, three-dimensional cross sections, or “slices,” of tissue can be obtained. The scanner rotates an entire 180 degree (half circle) around the area being examined, filming as it rotates 1 degree at a time. Information received by the scanner is relayed to a computer, which presents an image of the tissues one slice at a time. The “picture” presented by the computer is an interpretation of the varying densities of tissues, fluids, and bones. Tumors, as well as other abnormal structures within the body tissues, can be seen in this way.
Another imaging technique is called magnetic resonance imaging (MRI). As in CT scanning, MRI produces views of “slices” of tissue. MRI can sometimes “see” tumors and abnormalities that other techniques miss. It is currently used as a breast screening tool—in addition to mammography—for patients at high risk for breast cancer because of family history. MRI can also be used in real time to monitor cancer treatments. Patients with pacemakers, certain metal fragments, clips, or shrapnel in the body cannot use MRI because the powerful magnets used in this technique can bend and twist metal and can damage the body.
Endoscopy
An endoscope is an instrument used for direct visualization of internal body parts. It is designed so that it can be inserted and passed along the interior of hollow organs and cavities.
Types of endoscopes include the colonoscope for the colon, the bronchoscope for the trachea and bronchi, the laparoscope for the contents of the abdominal or pelvic cavity, and the cystoscope for inside the bladder. During an endoscopy, a sample of cells may be taken from a suspicious area so they can be examined more precisely under a microscope (biopsy).
Laboratory Tests
Although no one blood test can establish a definite diagnosis of cancer, certain tests are used to ascertain specific information. A complete blood count is helpful in diagnosing leukemia. The presence of a high level of prostate-specific antigen (PSA) may indicate prostate cancer. Current recommendations include offering a baseline PSA test for men over age 50, to be repeated at various intervals depending on the patient’s risk factors (Box 8-2).